Abstract
Aims: Fractional flow reserve (FFR) allows accurate investigation of the functional significance of intermediate coronary stenoses. The present study set out to study the impact of gender on FFR measurements.
Methods and results: Three hundred and seventeen intermediate (40-70% at angiography) stenoses were assessed with FFR in 270 patients (mean age 65.8±10.3 years, 84 females). Resting Pd/Pa (the ratio of mean blood pressure measured distal to the stenosis to mean aortic blood pressure in resting conditions), FFR (Pd/Pa during adenosine-induced hyperaemia) and the ΔPd/Pa (calculated as the change in Pd/Pa during hyperaemia) were measured. There was no difference in the location and degree of stenoses between genders (p>0.5). Similarly, there was no difference in age and in the prevalence of cardiovascular risk factors (all p>0.2). Resting Pd/Pa also did not differ between genders (0.92±0.08 vs. 0.93±0.05, p=0.23). In response to adenosine, however, a significantly larger ΔPd/Pa (0.14±0.07 vs. 0.11±0.07, p=0.001) and a significantly lower FFR (0.79±0.12 vs. 0.82±0.10, p=0.008) were observed in males. This difference was maintained in a multivariate regression analysis.
Conclusions: We observed gender-based differences in FFR data in daily routine. Further studies are necessary to test the mechanism of this observation and how these differences impact on the assessment of haemodynamically relevant stenoses.
Introduction
Although coronary angiography remains the cornerstone for the assessment of the presence of epicardial coronary lesions in the catheterisation laboratory, there are several well-known limitations to the accuracy of this technique1. The development of fractional flow reserve (FFR) as a tool for the assessment of the haemodynamic relevance of angiographically intermediate stenoses has brought a dramatic improvement in our diagnostic capacities, facilitating decision making in the catheterisation laboratory and leading to a substantial improvement in patients’ prognosis2-7.
FFR expresses the ratio of the maximum blood flow achievable in the presence of a stenosis to the maximum blood flow achievable in its absence, and is calculated as the ratio of the mean blood pressure distal to the stenosis divided by the mean blood pressure proximal to the stenosis during hyperaemia. FFR only provides information on the epicardial circulation but, since the procedure requires that maximal hyperaemia is achieved, the routine application of this method is based on the assumption that blood flow responses to fixed doses of vasodilatators invariably reproduce exercise-induced hyperaemia in all patients, and that this hyperaemia remains constant over time. A number of studies, however, provide evidence that the regulation of coronary blood flow is complex, varies across individuals and over time, and is affected by a number of factors and by the presence of comorbidities such as diabetes, hyperlipidaemia and hypertension8-11. Further, some authors have suggested that drug-induced hyperaemia might not reproduce “physiological” exercise-induced coronary flow reserve12.
While the use of FFR has been validated in the presence of diabetes and hypertension13, a number of other factors might have an impact on this parameter. Among these factors, the existence of gender-based differences in the mechanism, extent, and sequelae of ischaemia is well accepted14. To date, data on the impact of gender on FFR responses are limited. For instance, studies aimed at validating the use of FFR and setting the best cut-off values for the discrimination of haemodynamically relevant from non-relevant stenoses included a majority of male subjects15-18, and no gender-specific analysis was performed. This study was designed to investigate retrospectively the existence of gender differences in FFR data obtained in patients with intermediate focal coronary stenoses.
Materials and methods
FFR measurements performed in our institutions between May 2008 and May 2011 were reviewed retrospectively. Patients undergoing catheterisation for any reason other than stable (suspected) coronary artery disease (e.g., for hypertensive crisis associated with troponin elevation, or acute coronary syndromes) and those with known chronic inflammatory diseases, severe valvular disease, dialysis, myocardial disease or decompensated heart failure were excluded. Additional exclusion criteria comprised previous myocardial infarction in the coronary distribution under study, diffuse atherosclerosis or lesions longer than 5 mm, or the presence of more than one focal stenosis in the target vessel.
Coronary angiography and FFR measurements were performed using the standard Judkins approach. Briefly, all patients received unfractionated heparin. A 6 Fr guiding catheter was positioned at the ostium of the coronary, and a previously calibrated 0.014” XT Certus pressure-monitoring guidewire (St Jude Medical, Inc., St Paul, MN, USA) was advanced after equalisation of catheter and wire pressures in the periphery of the target vessel. Systolic, diastolic and mean blood pressures were measured proximal and distal to the stenosis at rest after administration of 200 μg of nitroglycerine i.c. After baseline measurements, adenosine was administered using one of two previously validated19 ways: intracoronary bolus (100 μg for the left and 60 μg for the right coronary) or intravenous infusion (via a 4 Fr sheath in the vena femoralis) at 140 or 170 μg/kg*min. The ratio of the mean distal intracoronary pressure (Pd) to the mean arterial pressure (Pa) was calculated at rest (Pd/PaRest) and during maximal hyperaemia (fractional flow reserve, FFR). Typically 60-90 seconds (i.e., until stable FFR values for at least 15 seconds were observed) are allowed before FFR measurements in the case of intravenous infusions. In the case of intracoronary bolus, FFR measurements were performed immediately. The change in FFR (ΔPd/Pa) was calculated by subtracting the FFR value after adenosine injection from the Pd/Pa value (FFR before adenosine injection) and as a % change in the Pd/Pa from baseline. Pullback was used to exclude the presence of diffuse coronary atherosclerosis in all cases (except those who received an adenosine bolus) and tracings with progressive normalisation of the FFR were excluded from the study. The adenosine infusion was maintained until the coronary wire had reached the ostium of the vessel under study. Angiographic lesion severity was determined off-line in randomised order by an investigator blinded to FFR data using quantitative coronary angiography (Xcelera; Philips, Eindhoven, The Netherlands).
CORONARY RISK FACTORS
The body mass index was calculated as the ratio between weight in kilogramme and the square of the height in meters. Coronary risk factors were defined as: smoking (or previous smoking); hyperlipidaemia (total serum cholesterol >220 mg/dL and/or serum triglycerides >200 mg/dL); hypertension (systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg on two consecutive seated measurements or therapy with antihypertensive medication); family history (first degree relatives with cardiovascular disease); diabetes mellitus (fasting serum glucose levels >126 mg/dL or therapy with oral hypoglycaemic agents or insulin).
STATISTICAL ANALYSIS
Data are presented as mean±SD or number (%). The t-test, the Fisher’s test or analysis of variance were used to compare continuous or nominal variables across genders as appropriate. The t-test or analysis of variance for unpaired data was used to assess the effect of nominal variables on FFR and ΔPd/Pa. Linear regression analysis was used to assess the association between single continuous variables, and a stepwise multivariate regression analysis was used to identify parameters independently associated with ΔPd/Pa and FFR (cut-off for entry: 0.05, for removal: 0.10). Variables included in the original equation comprised gender, age, body mass index, diabetes, hypertension, hyperlipidaemia, smoking, site of the stenosis (vessel involved as well as location in the proximal versus mid or distal third), quantitative coronary angiography parameters, type of hyperaemic stimulus and the sequence of the vessels studied in cases where more than one vessel was studied in the same patient. Coefficients are presented. All tests of significance were two-tailed. Statistical significance for the primary endpoint (the impact of gender on ΔPd/Pa and FFR upon multivariate analysis) was defined as a p-value of less than 0.05; all other p-values are reported but are formally to be considered exploratory. The statistical software MedCalc (MedCalc Software, Mariakerke, Belgium) was used for all statistical calculations.
Results
A total of 270 patients (mean age 65.8±10.3 years, 84 females) undergoing coronary angiography for suspected coronary artery disease (typical angina pectoris and/or positive provocative test and/or ECG suggestive of ischaemia) were included in the database. FFR data were available for a total of 317 intermediate (40-70% at angiography) focal (<5 mm) stenoses.
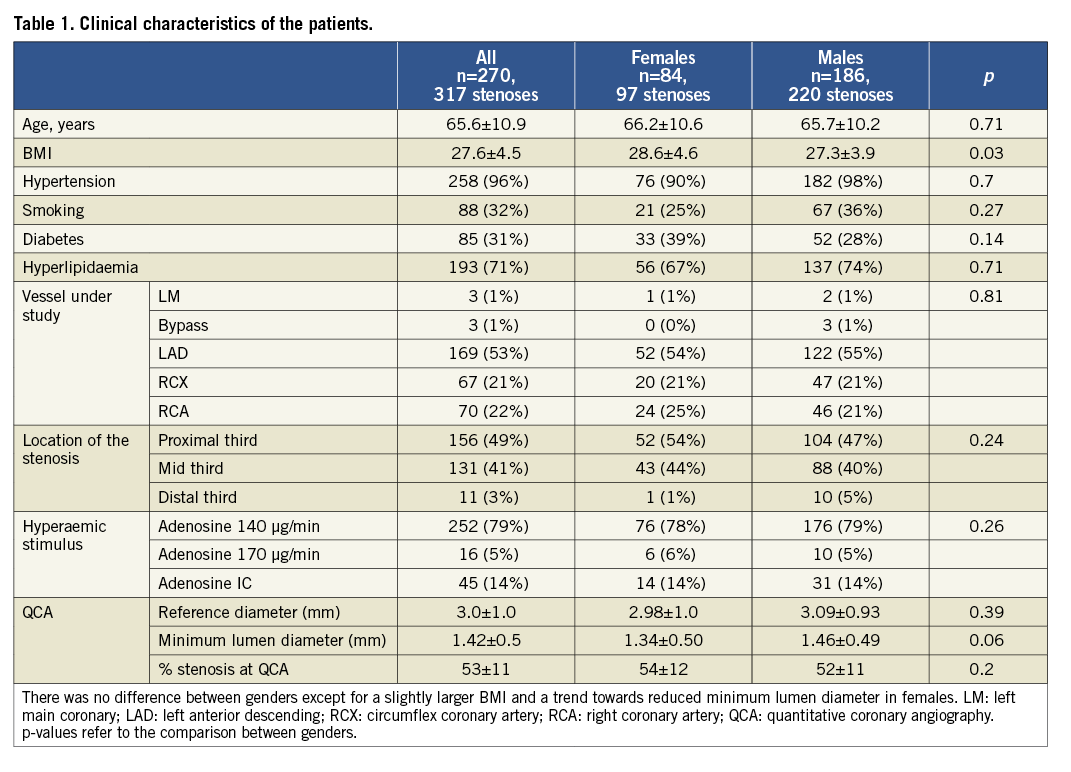
CLINICAL AND ANGIOGRAPHIC CHARACTERISTICS
The baseline clinical features of the study patients are shown in Table 1. There were no significant differences between genders in age, prevalence of risk factors, arterial blood pressure, vessel involved, or location of the stenosis under investigation. The body mass index was slightly larger in females. The angiographic characteristics of the stenoses and vessels under study were also similar between genders: there was no difference in reference diameter (p=0.39), minimum lumen diameter (p=0.06, showing a trend towards smaller vessels in females) and % stenosis at quantitative coronary angiography (p=0.20).
BLOOD PRESSURE RESPONSES DURING ADENOSINE INFUSION AND THE IMPACT OF GENDER
Data are presented in Table 2, Figure 1 and Figure 2. Pa, Pd and Pd/PaRest were similar between genders with a trend towards higher blood pressure values in females (respectively, p=0.12, p=0.06 and p=0.23). None of the blood pressure parameters was influenced by any of the risk factors, age or location of the stenosis.
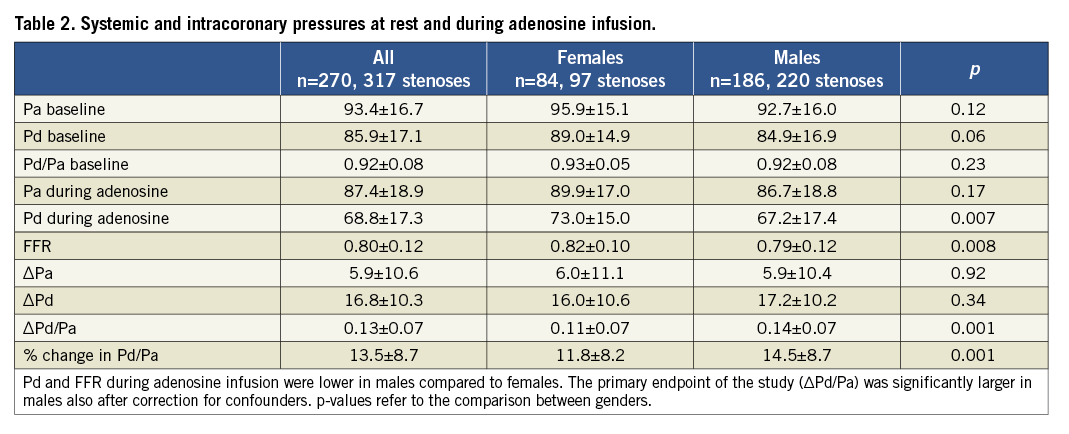
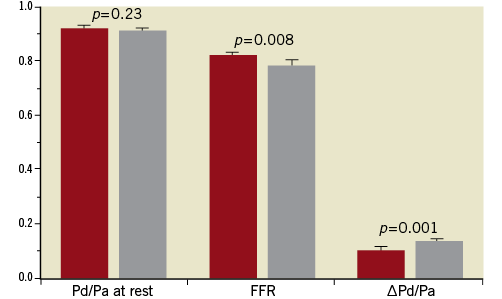
Figure 1. Percent change in Pa (aortic pressure) and Pd (pressure distal to the stenosis) in response to adenosine infusion. The percent change in Pd in females (red) was smaller than in males (grey bars).
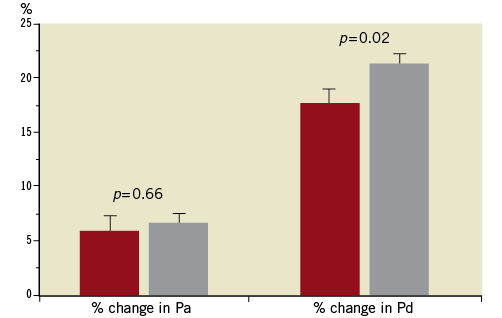
Figure 2. Pd/Pa values at rest and during adenosine (FFR). FFR was lower and ΔPd/Pa larger in males (grey bars). ΔPd/Pa was calculated as (Pd/PaRest) – FFR.
Adenosine was administered via intracoronary bolus in 49 cases (15 females), intravenous infusion at 140 μg/kg*min (251 cases, 76 females) or 170 μg/kg*min (17 cases, 6 females), with no difference between genders (p=0.26).
Pa also remained similar between genders during adenosine infusion (p=0.29). It decreased by 5.9±10.4 mmHg in females (p<0.0001 for the comparison between baseline and during adenosine) and by 6.0±11.1 mmHg in males (p<0.0001), without difference between genders (p=0.92). In contrast, there was a significant difference between genders in Pd (p=0.007), with a lower Pd in males compared to females. Pd decreased by 16.0±10.6 mmHg in females and by 17.2±10.2 mmHg in males (p<0.0001 within each gender, p=0.34 for the comparison between genders). There was also a significant difference in FFR and in the ΔPd/Pa (Pd/PaRest minus FFR) between genders, with a lower FFR and a larger ΔPd/Pa in males compared to females (respectively, p=0.008 and p=0.001). Similarly, the % decrease in Pd/Pa was lower in females than in males (p=0.001). Thirty-five stenoses in females and 102 in males had an FFR lower than 0.8 (p=0.08).
OTHER DETERMINANTS OF ΔPD/PA AND FFR
There was a very mild association between age and both ΔPd/Pa and FFR, i.e., the decrease in Pd/Pa was smaller and FFR was higher in older individuals (R2 respectively =0.07 and =0.02, p-values <0.0001 for both regression analyses). In contrast, BMI (p=0.53), the presence of diabetes (p=0.58), smoking (p=0.18), hyperlipidaemia (p=0.94), and hypertension (p=0.48) had no impact on ΔPd/Pa. Similarly, these factors had no impact on FFR (p-values respectively 0.37, 0.13, 0.13, 0.18 and 0.73). ΔPd/Pa (R2=0.02 and p=0.01) and FFR (R2=0.03, p=0.003) showed a very weak association with reference diameter, such that larger coronaries were associated with smaller ΔPd/Pa and larger FFR. The vessel under study also proved to have an influence on FFR and ΔPd/Pa, possibly as a result of differences in the distribution territory (Figure 3). As expected, FFR showed strong associations with Pd/PaRest (R2=0.59, p<0.0001) and % stenosis (R2=0.12, p<0.0001).
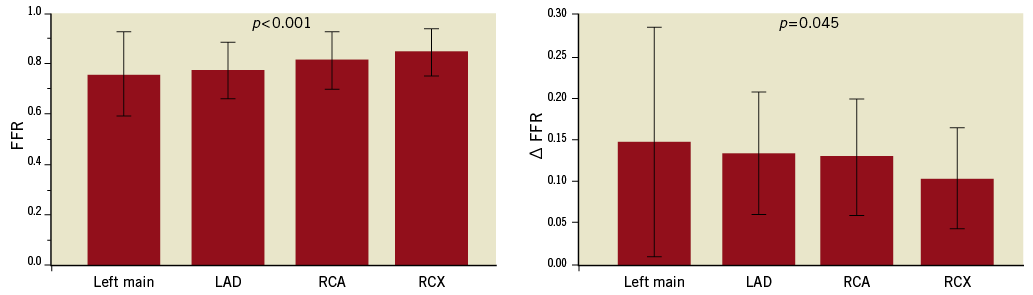
Figure 3. FFR and ΔPd/Pa data as a function of the vessel under study. The largest drop in ΔPd/Pa (and lowest FFR) was observed in the left anterior descending coronary artery. p<0.001 by ANOVA for FFR, p=0.045 for ΔPd/Pa.
Finally, a stepwise multivariate regression was performed to investigate the independent determinants of FFR and ΔPd/Pa among the variables described above. Age (p=0.0002, correlation coefficient=0.002), % stenosis at QCA (p<0.0001, correlation coefficient -0.28), gender (p=0.001, correlation coefficient 0.04), diabetes (p=0.048, coefficient =0.03), and vessel under study (p=0.0001, coefficient 0.02) were all associated with FFR (ANOVA p<0.001). The R2 of this model was 0.18. In a regression analysis including only patients who underwent infusion of adenosine 140 μg/kg*min via vena femoralis, age, gender, diabetes and % stenosis remained independent predictors (p=0.007, =0.0009, =0.03 and <0.00001, respectively). When the same analysis was performed for ΔPd/Pa, % of stenosis at QCA (p<0.0001, correlation coefficient 0.15), age (p=0.0005, coefficient –0.001) and gender (p=0.01, correlation coefficient 0.03) were retained in the model, with a R2 of 0.13. In a regression analysis including only patients who underwent infusion of adenosine 140 μg/kg*min via vena femoralis, age, gender and % stenosis remained independent predictors (p=0.0008, 0.002, 0.0003, respectively). After FFR assessment, 128 lesions (100 in males and 28 in females, p=0.008) received FFR-guided percutaneous coronary intervention.
Discussion
The introduction of FFR as an invasive method to study coronary physiology brought a dramatic improvement in our capacity to determine the haemodynamic impact of intermediate or complex stenoses and to identify those that may induce ischaemia3,16,20. Since FFR measures the relevance of a stenosis during hyperaemia, it is influenced by at least two factors: the first is the severity of the atherosclerosis of epicardial vessels (which, in the case of single focal stenoses translates into the severity of the stenosis); the second is the hyperaemia induced by the vasodilator infused and the extent of the myocardial perfusion area. A number of factors may influence these parameters. In this scenario, the impact of gender on FFR data remains poorly investigated.
INTERPRETATION OF THE PRESENT FINDINGS
Despite similar baseline clinical characteristics and similar coronary stenoses, we demonstrate that female patients show smaller ΔPd/Pa and larger FFR responses during adenosine infusion. These data emphasise the concept that FFR measurements may be determined, beyond stenosis severity (which was obviously the strongest determinant of FFR), also by a complex interaction of several factors. In our multivariate analysis, beyond gender and (as expected) % degree of stenosis, age, the presence of diabetes, and the vessel under study also showed a weak independent association with FFR data.
We also show that gender and, to a lesser extent, age are independent determinants of ΔPd/Pa beyond stenosis severity. Importantly, ΔPd/Pa, which expresses the increase in the transstenotic pressure gradient observed during hyperaemia, has been proposed to have an independent prognostic power, as a smaller ΔPd/Pa (independently of FFR) was associated with a worse prognosis during a 36±17 months follow-up21. While future studies are necessary to test the potential role of this parameter in clinical practice, the present data suggest that gender differences need to be taken into account (and the mechanisms of the associations demonstrated here need to be clarified) when these data are interpreted.
Further, our data also suggest a note of caution in the interpretation of FFR data. The studies which led to the identification of 0.75 or 0.8 as the threshold value for a positive FFR15,16 included a majority of males and did not perform a gender-specific analysis. Similarly, in the FAME and DEFER studies, the impact of FFR values below 0.80 was, until very recently, not formally analysed based on gender17,18,22. Suggesting that gender might have an impact on FFR values, however, in the 1996 paper by Pijls et al15 the proportion of females was different between FFR-positive and FFR-negative patients: in those with an FFR <0.75 this proportion was as low as 28%, while females were 46% of the patients with an FFR >0.75. This observation was substantiated in a very recent and important post hoc subanalysis of the FAME database, where Kim et al reported lower FFR values for males across different ranges of angiographic severity23. In this report, differences in age, prevalence of hypertension and unstable angina, vessel size and, most importantly, stenosis length were reported among genders. The impact of gender on FFR was confirmed in our database, where the above baseline differences were not present. While caution still needs to be exerted when trying to interpret retrospective observations mechanistically, it needs to be acknowledged that the impact of gender on FFR measurements is pathophysiologically interesting and might also have a clinical relevance in particular settings. For instance, while the differences between genders shown here are apparently small in absolute terms, we report mean FFR values of 0.79 in males and 0.82 in females, i.e., just below and just above the threshold usually used for the definition of haemodynamically relevant stenosis. While gender did not modify the benefit of performing FFR measurements in the FAME study23, the current data, in agreement with those of Kim et al23, suggest that angiographically similar stenoses might result in lower FFR values in males. Of note, weaker associations were also shown in our database with age, the presence of diabetes and the vessel under study. Differences in microvascular reactivity and in myocardial mass might also help to explain these observations, but these hypotheses remain speculative and further studies are needed.
Limitations of the study
There are a number of limitations to this study. The first, and most important, is that the cross-sectional, retrospective nature of this dataset makes it unfit to provide mechanistic explanations, and future studies are necessary to test the mechanisms of the observed differences (for instance differences in plaque composition, vessel size, clinical presentation, distribution area, intrinsic differences in the responsiveness to adenosine). Also, the clinical impact of gender-based differences in the parameters under study needs to be studied further. Second, adenosine was administered in different dosages and using different pathways. Previous studies have, however, shown that the different formulations of adenosine have no impact on FFR data19. Also, the statistical analysis was corrected for the formulation of adenosine used showing no impact on ΔPd/Pa and FFR, and a separate analysis was performed including only those patients who received adenosine via the femoral vein in the dosage of 140 μg/kg*min. Thirdly, we do not provide direct information on the role of microvascular responses (for instance using mean transit time, index of microvascular resistances and/or coronary flow reserve), capillary density, myocardial mass or contractility, and a variety of other potential mechanisms for the present observations, which remain to be investigated. Whatever the mechanism, however, gender-based differences in ΔPd/Pa and FFR are important given the role of these parameters in clinical practice. Further, stenosis length and severity also have an obvious role, and in order to limit the impact of these confounding variables we limited our study to focal lesions and intermediate stenoses (40-70% lumen diameter), which are in any case the usual target of FFR studies. Finally, one cannot theoretically exclude that classical angiography might have overestimated stenoses in females compared to males, such that the two groups might have differed in their baseline characteristics, explaining the difference in FFR. However, QCA analysis performed in a randomised blinded order showed that the trend was rather in the opposite direction (more severe stenoses in females compared to males, p=0.06, Table 1).
Conclusions
We report on the existence of gender-based differences in FFR data. Mechanistic studies are now important to determine the pathophysiology of this observation, and prospective studies will need to test whether these observations have clinical implications.
Acknowledgements
Part of the data presented here is included in the MD thesis of D. Orphal.
Conflict of interest statement
The authors have no conflicts of interest to declare.

