“As is our confidence, so is our capacity” – William Hazlitt
Coronary flow reserve (CFR) was originally formulated as a functional index to explore the functional relevance of coronary stenoses1. In a communicative way, the rationale behind CFR could be expressed as follows: “If you want to know if a stenosis is severe, go and ask the microcirculation”. A clever approach - coronary stenosis first causes subtended arterioles to vasodilate to maintain resting flow and, eventually, also causes a decrease in maximal hyperaemic flow. All this trims the range of microvascular vasodilation, indirectly measured by CFR.
Today, in the catheterisation laboratory, CFR has been virtually abandoned as a stenosis assessment method, and its original role has been taken by pressure-based methods such as fractional flow reserve (FFR) or instantaneous wave-free ratio (iFR). However, CFR is far from being dead: it is widely used in non-invasive ischaemia detection tests and is increasingly used in studying non-obstructive coronary disease (INOCA). Furthermore, new approaches such as coronary flow capacity (CFC) have been proposed to address some of the limitations of CFR2.
CFC provides a conceptual map depicting different scenarios of myocardial ischaemia, as outlined by hyperaemic myocardial flow and CFR values. Although CFC was originally proposed for positron emission tomography (PET) imaging, our groups contributed to adapting it for Doppler- and thermodilution-based intracoronary measurements3,4. Let’s take two examples illustrating how CFC provides a richer picture of coronary haemodynamics than CFR (Figure 1). The first scenario (left panel) is low CFR with preserved hyperaemic flow, which is compatible with high resting flow (triggered by different factors) but otherwise preserved myocardial perfusion. The second (right panel) is low hyperaemic flow with preserved CFR, which can be interpreted as preserved dynamicity of the coronary circulation (normal CFR) in a relatively small amount of non-ischaemic myocardium.
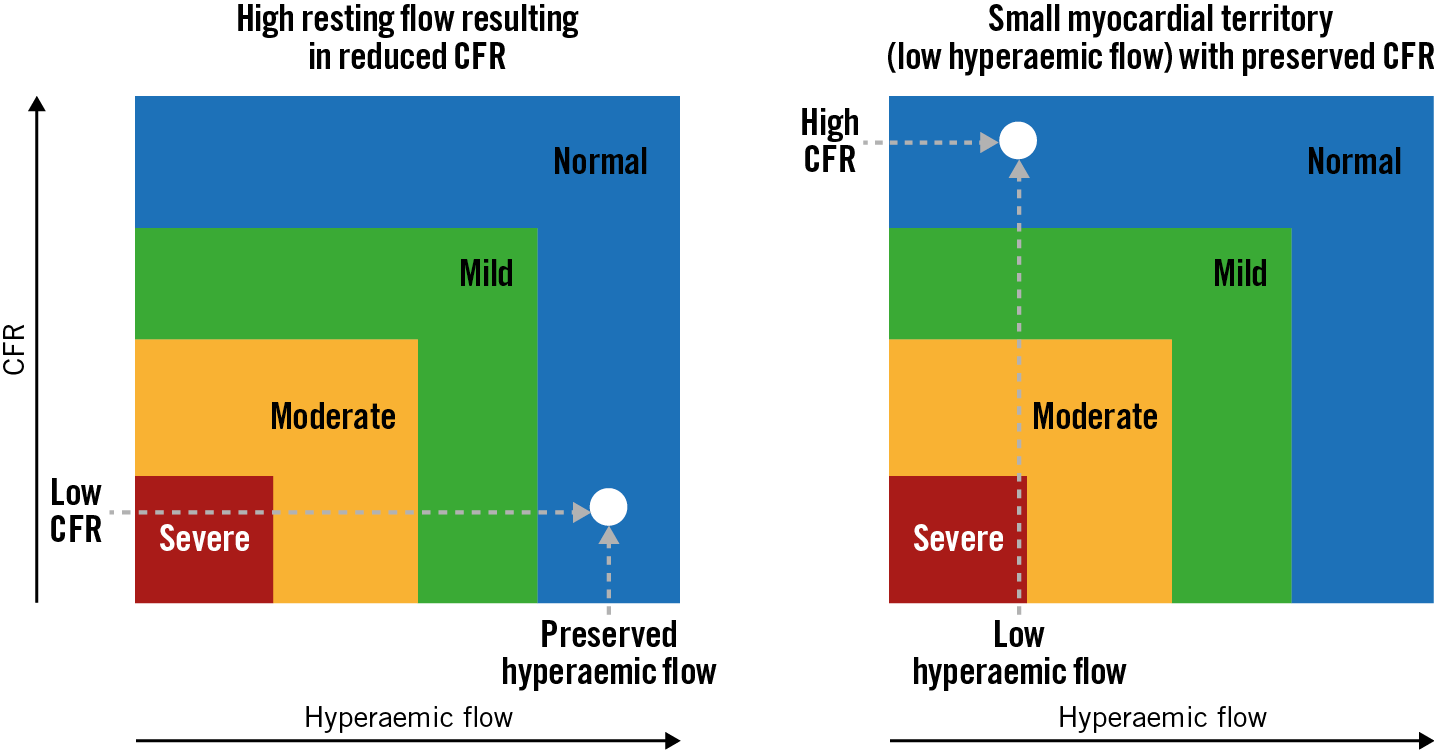
Figure 1. Added value of coronary flow capacity (CFC). Two examples of how CFC, compared to coronary flow reserve (CFR), can improve our understanding of coronary haemodynamics. Coloured areas correspond to different degrees of myocardial ischaemia according to CFC. See text for details.
In this issue of EuroIntervention, Stegehuis et al report on whether clinical and haemodynamic factors may influence CFR and CFC in a different manner5.
The investigators merged individual data from two trials from the 1990s, performed in patients undergoing percutaneous coronary intervention (PCI) in whom additional intracoronary Doppler measurements were made in a non-obstructed vessel. Based on data from 390 patients, the authors identified age and female gender as independent predictors of CFR, and age as the only predictor of CFC. From this, the authors conclude that CFC is more independent of clinical factors than CFR.
The observation on the effect of age on both indices is in agreement with studies showing an age-dependent decrease in maximal myocardial flow that affects both components of CFC6, and contributes to viewing ageing as a facilitating factor for myocardial ischaemia of microvascular origin. The effect of gender on CFR and CFC is particularly interesting. As in previous studies, female gender was associated with higher resting coronary flow, repeatedly pointed to as a major cause of false-positive CFR results. The results provide a signal on the corrective effect of CFC over CFR: most likely, female patients with low CFR due to high resting flow were reclassified as having normal CFC values whenever hyperaemic flow was preserved (Figure 1).
The authors should be congratulated for their research which contributes to a better understanding of these two physiological indices. However, it is important to keep in mind some problems that limit generalisation of the findings. For example, the dose of adenosine used in the source studies (12-20 mcg) was much lower than recommended nowadays to ensure maximal hyperaemia (>100 mcg). As no information on long-term outcomes of the patients was reported, we do not know if CFC was superior to CFR in terms of prognostication. Finally, despite the fact that Doppler measurements were made in vessels without stenoses, we should bear in mind that these were patients with ischaemia of obstructive origin undergoing PCI. The findings should not be extrapolated to patients with INOCA, in whom microvascular derangements are the most frequent cause of myocardial ischaemia.
The latter aspect is particularly relevant. There is growing evidence that INOCA patients with low CFR caused by high resting flow constitute a specific endotype of microvascular dysfunction, with reduced coronary perfusion efficiency during stress and higher rates of global myocardial ischaemia than those with normal CFR7. Patients with high resting coronary flow and impaired CFR have a worse prognosis than patients with normal CFR8. The existence of an underlying pathological substrate is also supported by the fact that high resting coronary flow improves with exercise, dietary changes and treatment with angiotensin-converting enzyme inhibitors9,10. As CFC does not take into account resting flow, its prognostic power in this subset of patients remains unknown.
We are currently living through the transition from a stenosis-centred paradigm of myocardial ischaemia to one that acknowledges the existence of previously overlooked non-obstructive causes. This study provides valuable information on the use of CFC in the context of the first paradigm; however, dedicated studies on the value of CFR and CFC in patients with INOCA are needed. Only then will assessment of the capacity of coronary circulation be performed with full confidence.
Conflict of interest statement
J. Escaned reports speaker/consultancy fees from Abbott, Boston Scientific and Philips. T. Kakuta has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.