Background
The era of coronary revascularisation has now entered its fifth decade but despite unparalleled advances in non-invasive stress testing, stent technology, adjunctive devices, and the pharmacotherapeutic armamentarium, all contributing to a positive impact on clinical outcomes, the debate over mechanical intervention versus an initial conservative strategy for the management of stable coronary artery disease continues to simmer beneath the surface. Central to resolving this controversy has been the synergy created between accurate morphologic characterisation of a coronary stenosis allied to a validated assessment of its functional significance. Despite its topographical precision, further augmented by the use of quantitative analysis, coronary angiography only provides a 2-dimensional silhouette of what is a 3-dimensional intravascular environment. It has been shown to correlate poorly with the physiological impact of equivocal coronary lesions of 30-80% severity. Since its inception and subsequent validation, fractional flow reserve (FFR) has been widely accepted as a robust, pressure-derived, index of flow across a coronary lesion. Together, coronary angiography and FFR, allow the interventionist to tailor an effective therapeutic strategy for those patients presenting with intermediate diameter stenoses (Figures 1 and 2).
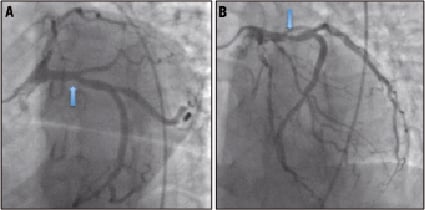
Figure 1. A proximal left circumflex (LCx) artery lesion of debatable anatomical significance by coronary angiography. Plate A: Left anterior oblique caudal view in which the LCx artery appears to have a 40%-50% proximal stenosis (arrow). Plate B: Left anterior oblique cranial view in which the same proximal LCx stenosis now looks in the order of 70%-80% (arrow). Images courtesy of Dr Tim Lockie.

Figure 2. A subsequent pressure wire study of the same proximal LCx artery lesion gives an FFR of 0.72 suggesting the stenosis is of haemodynamic significance. Image courtesy of Dr Tim Lockie.
FFR is defined as the ratio of maximal hyperaemic myocardial blood flow across a stenosed artery to the maximal myocardial blood flow across the same artery in the theoretical absence of the stenosis. By applying Ohm’s Law, and at maximal hyperaemia where resistance is assumed to be minimal and constant, pressure can be used as a surrogate marker of flow. Since the pressure in a normal coronary artery is equivalent to aortic pressure (Pa), the FFR can simply be derived as a ratio of the mean distal coronary pressure (Pd) at a point past the stenosis to the Pa during maximal hyperaemia where FFR=Pd/Pa. This calculation, however, is based on an assumption that central venous pressure is close to zero at maximal hyperaemia. Some investigators would argue that the right atrial pressure (Pra) should be actively measured and used as a more precise estimate of central venous pressure such that FFR=(Pd–Pra)/(Pa–Pra).
The theoretical FFR of a normal coronary artery is 1.0, regardless of patient or vessel characteristics. FFR <0.75 is invariably associated with myocardial ischaemia with an overall accuracy of 93% whereas an FFR >0.80 is associated with negative ischaemic results and a predictive accuracy of 95%. This leaves a “grey zone” of uncertainty (i.e., 0.75–0.80) for which the interventionist must apply sound clinical judgement. By incorporating the Pra into the equation, rather than assigning a fixed value for central venous pressure, this “grey zone” has been reported to become less of an issue.
Indications
Current European Society of Cardiology and European Association for Cardio-Thoracic Surgery guidelines on myocardial revascularisation published in 2010 recommend the use of FFR for the physiological assessment of “moderate” coronary stenoses when functional information is lacking.
The most recent percutaneous coronary intervention guidelines issued by the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions in 2011 go one step further. They assign a Class IIa, Level of Evidence A (largely based on results of the landmark DEFER and FAME trials), recommendation on the use of FFR to assess intermediate coronary lesions (50% to 70% diameter stenosis) and suggest that FFR can be “useful” for guiding revascularisation decisions in patients with symptomatic coronary disease.
Methods
There are currently two main pressure wire systems available, manufactured by Volcano Corporation (San Diego, CA, USA) and St Jude Medical (St Paul, MN, USA). Both incorporate 0.014-inch hydrophilic pressure-sensored angioplasty guidewires which are inserted through a guide catheter and in to the target artery. Prior to crossing the lesion, the pressure wire signal is first calibrated to the guide catheter signal and then passed across the stenosis under investigation. Maximal arteriolar vasodilatation is most commonly induced by using intravenous or intracoronary adenosine. FFR is then calculated as the ratio of distal coronary pressure as measured by the pressure wire and mean aortic pressure as measured by the guiding catheter. A catheter placed in the right atrium to measure Pra, via the femoral vein, may also be used.
Difficulties
Potential difficulties can arise when assessing FFR in specific anatomical situations such as:
– diffuse or serial stenoses;
– bifurcation lesions;
– left main stem or ostial disease assessment;
– multivessel coronary artery disease;
– coronary artery bypass graft conduit patency; and
– in the context of left ventricular hypertrophy and acute coronary syndromes.
A thorough analysis of this along with practical tips and tricks and the common pitfalls associated with FFR measurement are included in the complete online version of this article, as is an overview of the emergence of novel catheter-based physiological assessments of coronary haemodynamics beyond FFR.
Funding
A. Myat and K. Asress acknowledge financial support from the Department of Health via the National Institute for Health Research (NIHR) comprehensive Biomedical Research Centre award to Guy’s & St Thomas’ NHS Foundation Trust in partnership with King’s College London and King’s College Hospital NHS Foundation Trust along with Clinical Research Training Fellowships awarded by the British Heart Foundation.
Acknowledgements
We would like to thank Dr. Tim Lockie for kindly allowing us to reproduce his images.
Conflict of interest statement
The authors have no conflicts of interest to declare.

