Fractional flow reserve (FFR) is defined as the ratio of distal-to-proximal (i.e., coronary-to-aortic) pressure measured during maxi-mum hyperaemia, assuming a negligible venous pressure. By comparing the maximum flow in a stenosed coronary artery to the theoretical maximum flow in the same vessel without stenosis, FFR provides an objective estimate of the functional severity of the stenosis, moving the focus of revascularisation from anatomy to physiology1.
An FFR-guided percutaneous coronary intervention (PCI) strategy has been reported to produce better clinical outcomes as well as improved cost-effectiveness compared to angio-guided PCI2,3,4. Recently, the FAME 2 trial (Fractional Flow Reserve Guided Percutaneous Coronary Intervention Plus Optimal Medical Treatment vs Optimal Medical Treatment) reported that a composite outcome of death, myocardial infarction, or urgent revascularisation (which largely drove the composite outcome) at five-year follow-up was significantly lower in patients undergoing FFR-guided PCI versus those receiving medical therapy only5.
Might these intriguing outcomes observed in the setting of PCI be translated to the coronary artery bypass grafting (CABG) setting as well? This question has indeed fueled great interest and has been addressed in at least three clinical trials.
The FARGO trial (Fractional Flow Reserve Versus Angiography Randomization for Graft Optimization)6 evaluated graft patency and clinical outcomes at six months in 100 patients randomised to angiography-guided CABG and complete anatomical revascularisation, or FFR-guided CABG, in which coronary arteries with angiographically significant stenoses but with an FFR >0.80 were deferred (not bypassed). No between-group differences were found with respect to the primary outcome measure of graft failure (16% vs 12%). Moreover, there were no differences in the rates of death, myocardial infarction, revascularisation and stroke. Of note, >75% of grafts in FARGO were saphenous vein grafts (SVGs).
In the IMPAG (Impact of Preoperative FFR on Arterial Bypass Graft Functionality) trial7, both coronary angiography and FFR were performed as part of the diagnostic workup of patients who were subsequently submitted to total arterial CABG. Surgeons were aware of FFR results and the grafting strategy was left to the operating surgeons’ discretion. At six-month follow-up, FFR but not angiographic stenosis severity was a predictor of arterial anastomosis patency and functionality; of note, anastomoses performed to coronary arteries with an FFR <0.78 had a patency rate of 97%. In IMPAG only arterial grafts were used.
In this issue of EuroIntervention, Toth and colleagues report the one-year results of the GRAFFITI (GRAft patency after FFR-guided versus angiography-guided CABG) trial8.
Patients with stable coronary artery disease (n=172) underwent angiographic evaluation along with FFR assessment but the FFR values were initially kept concealed. After a surgical revascularisation plan was formulated (based on angiographic data only), patients were randomised to angiography- or FFR-guided CABG (84 and 88 patients, respectively). In the latter group, the surgeon was informed on the FFR values (cut-off for revascularisation was set at 0.80). At one year, no difference in overall graft patency (80% vs 81%, respectively; p=0.885) or in the composite of death, myocardial infarction, target vessel revascularisation and stroke was found. The trial was probably underpowered for both clinical and angiographic outcomes. In fact, due to slow enrolment, GRAFFITI was halted at 83.5% of the initially proposed sample size. In addition, angiographic control was not performed in 33% and 37% of the patients in the angiography- and FFR-guided groups, respectively. Finally, surgeons’ reluctance to base their surgical strategy on FFR might have jeopardised the signifi-cance of FFR guidance in the trial; indeed, in the FFR-guided group, 29% of the deferred vessels had FFR ≤0.80 and 11% of bypassed vessels had FFR >0.80. In GRAFFITI, the ratio of arterial to venous grafts used was 1:1.
So, what do we know at present on FFR-guided CABG? In terms of graft patency, data from IMPAG contradict the findings from FARGO and GRAFFITI. This is probably related to the difference in the types of graft used in the different trials (all arterial grafts in IMPAG, a high percentage of vein grafts in the other two). It is well known that SVGs are less susceptible to competitive flow than arterial grafts and this is the most likely reason for the apparently contradictory findings (Figure 1). In terms of clinical outcomes, and accepting that all the trials were very largely underpowered, no clinical benefit of FFR-based CABG has been shown so far.
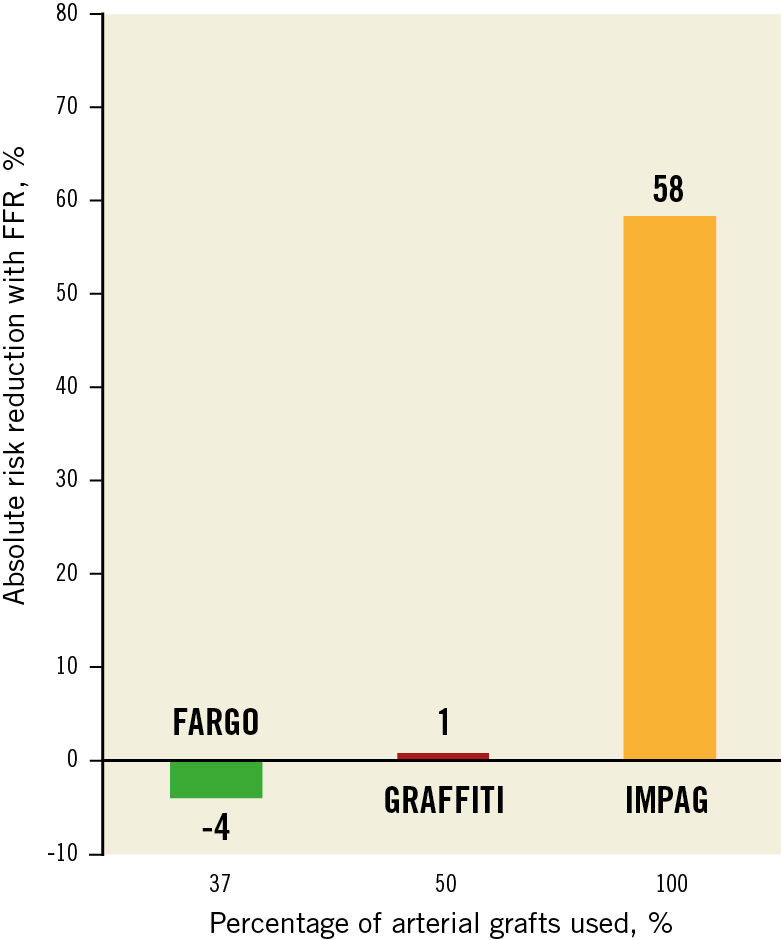
Figure 1. Potential reduction in graft dysfunction with FFR in relation to the type of graft used. The percentage of arterial grafts in the study is plotted on the x-axis and absolute percentage risk reduction using FFR on the y-axis.
On the other hand, using FFR to guide surgical revascularisation may have important theoretical downsides. In addition to providing direct revascularisation, angiography-based CABG exerts a protective effect from coronary events independently of the severity of the target vessel stenosis by providing what has been defined as “surgical collateralisation”9. An implicit risk of FFR-guided CABG is that this collateralisation effect of surgery may be lost – something that clearly does not apply to the PCI setting.
In addition, it is well known that anatomically incomplete revascularisation is a strong negative prognostic determinant after CABG10. The consequences on an increase in the rate of anatomically incomplete revascularisation due to the use of FFR are unknown at present. It must be highlighted that all the current evidence on CABG (including the comparison with medical therapy and PCI) is founded in studies that used anatomic (not functional) criteria to guide grafting.
Based on the current evidence, FFR seems an important tool for the decision on which type of graft to use (arterial for lesions with an FFR <0.78, venous for those with higher values). However, in the absence of data from larger trials powered to detect differences in clinical outcomes, the use of FFR to guide the indication to the revascularisation strategy (CABG or PCI) or the target vessels to be grafted should be discouraged.
Conflict of interest statement
The authors have no conflicts of interest to declare.