Abstract
Aims: Adoption of fractional flow reserve (FFR) remains low (6-8%), partly because of the time, cost and potential inconvenience associated with vasodilator administration. The instantaneous wave-Free Ratio (iFR) is a pressure-only index of stenosis severity calculated without vasodilator drugs. Before outcome trials test iFR as a sole guide to revascularisation, we evaluate the merits of a hybrid iFR-FFR decision-making strategy for universal physiological assessment.
Methods and results: Coronary pressure traces from 577 stenoses were analysed. iFR was calculated as the ratio between Pd and Pa in the resting diastolic wave-free window. A hybrid iFR-FFR strategy was evaluated, by allowing iFR to defer some stenoses (where negative predictive value is high) and treat others (where positive predictive value is high), with adenosine being given only to patients with iFR in between those values. For the most recent fixed FFR cut-off (0.8), an iFR of <0.86 could be used to confirm treatment (PPV of 92%), whilst an iFR value of >0.93 could be used to defer revascularisation (NPV of 91%). Limiting vasodilator drugs to cases with iFR values between 0.86 to 0.93 would obviate the need for vasodilator drugs in 57% of patients, whilst maintaining 95% agreement with an FFR-only strategy. If the 0.75-0.8 FFR grey zone is accounted for, vasodilator drug requirement would decrease by 76%.
Conclusion: A hybrid iFR-FFR decision-making strategy for revascularisation could increase adoption of physiology-guided PCI, by more than halving the need for vasodilator administration, whilst maintaining high classification agreement with an FFR-only strategy.
Introduction
Despite the evidence demonstrating the benefits of coronary revascularisation guided by fractional flow reserve (FFR)1-3, its adoption into widespread clinical practice remains low: estimated as 6-8% worldwide4,5. The reasons for this are multifactorial4, including incomplete reimbursement, lack of widespread easy access to vasodilator drugs and challenges associated with technicalities of the procedure.
The need for vasodilator administration for FFR calculation is perhaps a common contributor to all these factors. Therefore, a diagnostic strategy which decreases the proportion of patients which needs vasodilator administration could potentially simplify assessment and reduce procedural time and costs. Such an approach would have the potential to bring physiology-guided revascularisation to many more patients, thereby improving clinical outcomes and improving healthcare cost-efficiency6.
The instantaneous wave-Free Ratio (iFR) is a novel pressure-only invasive index of coronary stenosis severity which does not require the administration of vasodilator drugs, such as adenosine7. Like FFR, iFR uses only pressure and is performed with a standard coronary pressure guidewire. However, in contrast to FFR, iFR is calculated at rest, without pharmacological provocation. Recent studies which directly compared the classification of intermediate coronary stenoses by iFR and FFR7-9 revealed a consistent pattern of agreement between the two methods: 1) outside of the intermediate range of iFR and FFR values agreement is very high (>90%), whilst 2) disagreements are of small magnitude and concentrated in the zone near their cut-offs8. Trials with clinical endpoints will evaluate whether these small disagreements in the uncertain zone around the current FFR cut-off affect patient outcome.
Meanwhile, the high classification agreement between FFR and iFR outside of the intermediate zone may provide the opportunity for a staged, hybrid iFR-FFR decision-making strategy, in which only patients within a certain range of intermediate iFR values would require adenosine for FFR classification of lesions. This hybrid iFR-FFR strategy might achieve a high classification agreement with an FFR-only approach (and thus continue to deliver an FFR-based classification of lesions), whilst significantly reducing the number of patients who require vasodilator administration.
In this study, we sought to evaluate the proportion of patients in clinical practice which could be free from vasodilator administration in a hybrid iFR-FFR decision-making strategy of revascularisation whilst matching the stenoses classification of an FFR-only strategy.
Methods
PATIENT POPULATION
This study evaluated 577 coronary stenoses from 550 patients in which iFR and FFR was compared. Studies and centres contributing data were: the European ADVISE Registry study population (Hospital Clínico San Carlos in Madrid, Spain; Guy’s and St Thomas’ NHS Foundation Trust, London, UK; and the Academic Health Science System of Imperial College London, UK; N=339)8; and an independent South Korean study (Seoul National University Hospital and Keimyung University Dongsan Medical Center; N=238)9.
HAEMODYNAMIC DATA COLLECTION AND ANALYSIS
Acquisition of physiological data for FFR calculation was performed according to conventional practice10 using commercially available FFR systems (RadiView console and PressureWire Certus; St. Jude Medical, Minneapolis, MN, USA; and Combomap console and Prestige pressure guidewire; Volcano Corporation, San Diego, CA, USA). In the European cohort (N=339), intravenous adenosine was used for the calculation of FFR in 98% of the cases, administered via a central line, with doses ranging from 140 mcg/Kg/min to 200 mcg/Kg/min; in the remaining 2% of the cases the intracoronary route was used. In the South Korean cohort, both intravenous and intracoronary routes were used in each patient (140 mcg/Kg/min intravenously and 40 mcg-80 mcg for intracoronary), and the lowest value of FFR was chosen for analysis. Digital data was extracted from FFR console platforms and processed off-line in a core laboratory (International Centre for Circulatory Health, National Heart and Lung Institute, UK) using a custom software package with Matlab (Mathworks, Inc., Natick, MA, USA). Each iFR trace was evaluated blinded from its FFR counterpart. iFR was calculated using fully automated algorithms applied to time-aligned pressure traces over the wave-free period of diastole over a minimum of five beats, before adenosine administration, as previously described7. iFR is defined as the ratio of distal coronary pressure to proximal coronary pressure during the wave-free period in diastole. Resting Pd/Pa was calculated from baseline traces, as the ratio of mean distal (Pd) to proximal (Pa) coronary pressures, over the entire cardiac cycle.
COMPARISON BETWEEN HYBRID IFR-FFR STRATEGY AND FFR-ONLY STRATEGY
This study retrospectively compared two possible strategies to guide coronary revascularisation:
STRATEGY 1: FFR-ONLY STRATEGY
This strategy was used as the reference. All interrogated stenoses received adenosine for FFR calculation and all decisions were based on the final FFR result using the currently recommended 0.8 cut-off value. No decision was taken based on the iFR result.
STRATEGY 2: HYBRID IFR-FFR STRATEGY
A series of two independent iFR values was identified: one with a high negative predictive value (exceeding 90%) to exclude FFR-significant stenoses (defer iFR value) and another with a high positive predictive value (exceeding 90%) to identify FFR-significant stenoses (treatment iFR value). A positive result was defined as FFR or iFR ≤0.8 and it was assumed that only stenoses with iFR values between the defer and treatment iFR values would have been given adenosine and followed standard FFR classification of lesions (Figure 1).
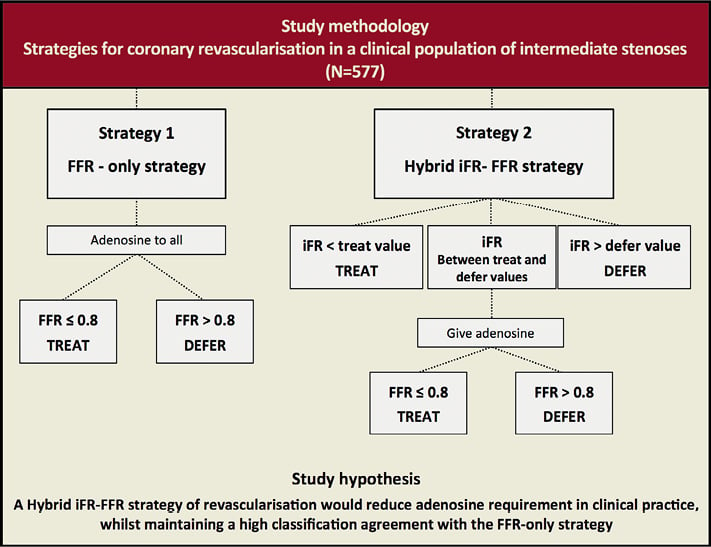
Figure 1. Study methodology flowchart and study hypothesis.
ENDPOINTS FOR COMPARISON BETWEEN FFR-ONLY AND HYBRID IFR-FFR STRATEGIES
This study used the following endpoints to compare the two strategies:
OVERALL CLASSIFICATION AGREEMENT BETWEEN STRATEGIES
Given its proven safety as a guide to revascularisation, the classification of stenoses by the FFR-only strategy was used as the reference. The overall classification agreement (when both strategies classified a stenosis as significant or not significant) between the iFR-FFR strategy and the FFR-only strategy was calculated. An overall agreement of 95% was considered ideal.
PROPORTION OF PATIENTS ADENOSINE-FREE
In the hybrid iFR-FFR strategy, the proportion of stenoses which fell outside the adenosine requirement zone (which would be free from adenosine in a hybrid iFR-FFR strategy) was calculated for each level of overall agreement with the FFR-only strategy. For comparison, in the FFR-only strategy, all interrogated stenoses (100%) required adenosine administration. In the hybrid iFR-FFR strategy, the size of the zone between the defer and treatment iFR values was calculated (in 0.01 iFR units). This zone represented the iFR values within which administration of adenosine was required for FFR calculation.
COMPARISON WITH A HYBRID Pd/Pa-FFR STRATEGY
The same methodology was then applied for the evaluation of a Pd/Pa-FFR hybrid strategy. The proportion of vessels which would be free from adenosine with a hybrid Pd/Pa-FFR strategy was compared to the iFR-FFR strategy, for each level of agreement with the FFR-only strategy.
STATISTICAL ANALYSIS
Statistical calculations were performed using Matlab (Mathworks, Inc.). Data were expressed as mean±standard deviation for continuous variables and percentages for categorical variables.
Results
POPULATION CHARACTERISTICS
Patient demographics and stenosis characteristics are summarised in Table 1. The majority of stenoses were physiologically intermediate, representative of patients undergoing FFR assessment of intermediate lesions in daily clinical practice. Mean FFR was 0.81±0.10; 80% of stenoses had FFR between 0.6 and 0.9; and only 13% had FFR ≤0.7 (Figure 2).
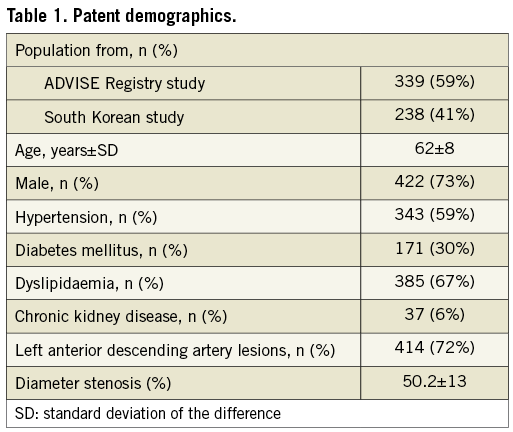
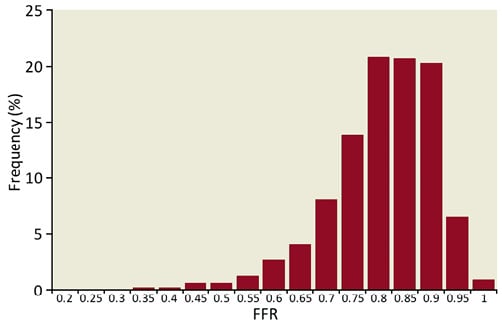
Figure 2. Frequency histogram of study population: distribution of FFR values. The majority of lesions were classified as physiologically intermediate, with mean FFR 0.81±0.1 and 80% of FFR values between 0.6 and 0.9.
OVERALL CLASSIFICATION AGREEMENT BETWEEN HYBRID IFR-FFR STRATEGY AND FFR-ONLY STRATEGY
Using a deferral iFR value of >0.93, a treatment iFR value of <0.86 and with adenosine only given to stenoses with iFR values between 0.86 and 0.93, resulted in an overall 95% agreement with the FFR-only strategy (Figure 3). A deferral value of iFR >0.93 demonstrated a negative predictive value of 91% to exclude FFR-significant stenoses and a treatment iFR value of <0.86 had a positive predictive value of 92% to identify FFR-significant stenoses.
Figure 3. Hybrid revascularisation strategy with instantaneous wave-Free Ratio (iFR) and fractional flow reserve reduces the adenosine requirement in clinical practice: coronary revascularisation decisions can be made without adenosine when iFR is <0.86 (positive predictive value of 92%) or when iFR is >0.93 (negative predictive value of 91%). In clinical practice, such iFR-based decisions can be made in 57% of patients. When iFR values fall between 0.86 and 0.93, adenosine is given and the FFR cut-off of 0.8 is used to guide revascularisation. This hybrid iFR-FFR approach has a 95% classification agreement with an FFR-only, adenosine-to-all, strategy. Green dots represent the agreement between iFR and FFR and red dots show disagreement points. Grey dots inside the grey zone represent the stenoses which will be classified by FFR, following adenosine administration.
REDUCTION IN ADENOSINE REQUIREMENT WITH HYBRID IFR-FFR STRATEGY
The utilisation of a hybrid iFR-FFR strategy would have significantly reduced the number of patients in whom adenosine was required. For an overall classification agreement of 95% with the FFR-only (adenosine-to-all) strategy, in the hybrid iFR-FFR strategy 57% of the stenoses would have become adenosine-free (Figure 3 and Figure 4). For a classification agreement between the strategies of 85% and 90%, respectively, the stenosis population predicted to be free of adenosine was 88% and 74%, respectively (Figure 4 and Figure 5).
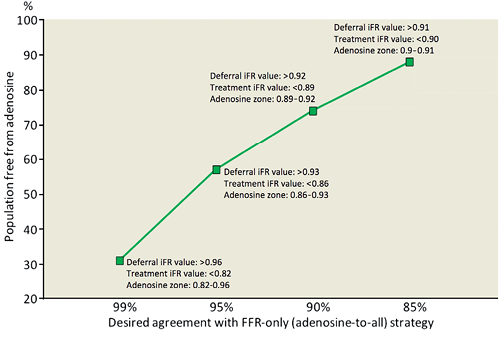
Figure 4. Hybrid iFR–FFR strategy reduces the number of patients requiring adenosine for any desired agreement with an FFR-only strategy. Using a hybrid iFR-FFR approach can reduce adenosine requirement in clinical practice by 74% with a 90% agreement with an FFR-only, adenosine-to-all, approach. For 95% and 99% agreement, the reduction in adenosine requirement would be 57% and 31%, respectively.
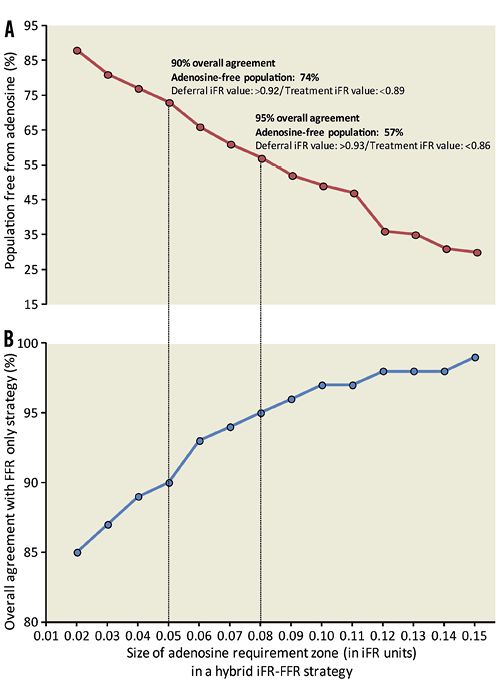
Figure 5. Population free from adenosine and the overall agreement with an FFR-only strategy depends on the size of the adenosine requirement zone: if adenosine is given to a larger window of iFR values, the diagnostic agreement with a FFR-only strategy increases (lower panel), albeit at a cost of fewer patients being free from adenosine (upper panel).
SIZE OF ADENOSINE REQUIREMENT ZONE
For a hybrid iFR-FFR strategy with a 95% classification agreement with the FFR-only strategy the width of the adenosine requirement zone was 0.08 iFR points (from 0.86 to 0.93), which represented 43% of this study population. The larger the adenosine requirement zone, the higher the overall agreement between a hybrid iFR-FFR strategy and the FFR-only strategy. However, increasing the adenosine zone also decreased the proportion of stenoses which became adenosine-free (Figure 5).
INCREMENTAL BENEFITS OF A HYBRID IFR-FFR STRATEGY COMPARED TO A HYBRID PDPA-FFR STRATEGY
iFR is superior to PdPa when used in a staged approach with FFR. For the same level of agreement with the FFR-only strategy, a hybrid iFR-FFR strategy significantly increased the number of adenosine-free patients when compared to a hybrid PdPa-FFR strategy. For magnitudes of agreement of 90%, 96%, respectively, the proportion of adenosine-free patients gained with iFR (over Pd/Pa) was 21%, and 28% (Figure 6).
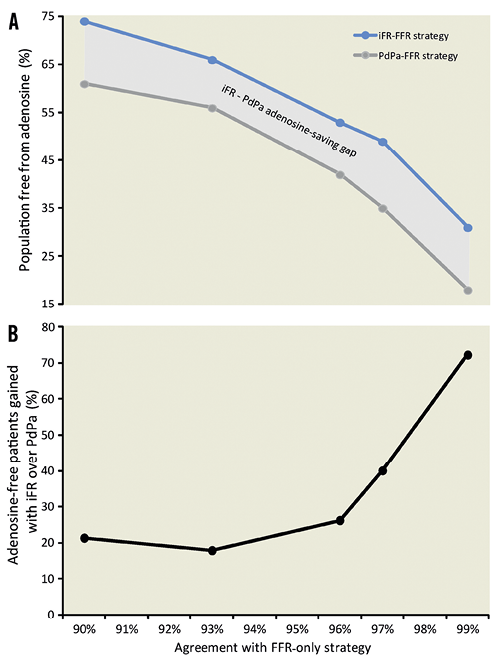
Figure 6. Incremental adenosine-saving benefits of iFR over resting PdPa. For each level of agreement with an FFR-only strategy, the utilisation of a hybrid iFR-FFR strategy significantly increases the adenosine-free population, when compared to a hybrid PdPa-FFR strategy. The absolute number of patients saved with each strategy is shown in the top panel, with the incremental benefit of iFR over PdPa demonstrated in the bottom panel.
Discussion
Whilst we await clinical trials which evaluate the safety of iFR as an independent tool to guide coronary revascularisation, this study shows that a hybrid decision-making strategy of coronary revascularisation with iFR and FFR has the potential to foster adoption of physiology-guided PCI. Our results demonstrate that such an approach has the potential to reduce drastically the need for adenosine administration whilst maintaining a 95% classification agreement with an FFR-only strategy.
IMPLICATIONS OF THE INCREASED ADOPTION OF PHYSIOLOGY-GUIDED PCI
Adding to the evidence already provided by the DEFER and FAME trials1,2,11, the FAME II study recently demonstrated that, when compared to medical therapy alone, percutaneous coronary intervention (PCI) can reduce coronary events, when flow-limiting lesions are identified by FFR3. It is therefore unfortunate that currently 92 to 94% of all coronary interventions worldwide are performed without any invasive physiological guidance4,5,12, and it is clearly in the patients’ interest to make physiology-guided PCI available to all. As the need for the administration of adenosine is one of the impediments to FFR utilisation4,13-15, a hybrid strategy with iFR could potentially facilitate the application of pressure wire interrogation, decrease procedural time13, costs6, avoid the small risks associated with central venous access and adenosine administration and minimise patient inconvenience. Also, as the need for a femoral venous sheath would be avoided in the majority of patients, a hybrid iFR-FFR strategy could potentially increase the number of radial procedures, which is in itself associated with improved outcomes16. Our results, therefore, suggest that a hybrid revascularisation strategy with iFR and FFR has the potential to significantly increase adoption of physiology-guided PCI in clinical practice, by combining iFR and FFR in the same diagnostic pathway (Figure 3 and Figure 7).
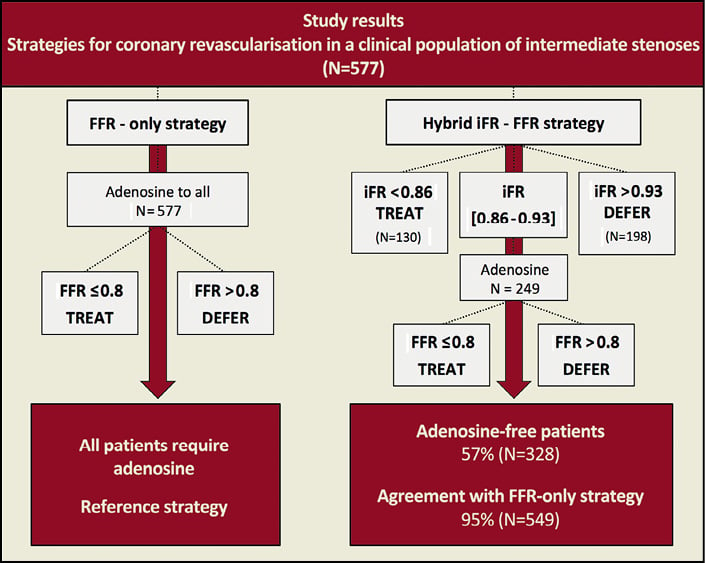
Figure 7. Summary of the predicted results of a hybrid decision-making revascularisation strategy with instantaneous wave-Free Ratio (iFR) and fractional flow reserve (FFR).
ADENOSINE-FREE POPULATION DEPENDS ON DESIRED AGREEMENT WITH FFR
The desired magnitude of agreement between a hybrid iFR-FFR strategy and an FFR-only strategy will determine the proportion of adenosine-free patients in any given population and the iFR values chosen to make deferral or treatment decisions (Figure 4).
If limits of iFR were chosen to achieve an overall 95% agreement with FFR we found that this would free 57% of patients from adenosine during physiological assessment in the cathlab. We believe this represents a safe and clinically meaningful balance between classification match and potential for increased adoption of physiology-guided procedures. However, if a 90% overall match with an FFR-only strategy was to be accepted, the proportion of patients free from adenosine would increase to 74%, with iFR values to defer and treat of <0.89 and >0.92, respectively (adenosine would be required when iFR falls between 0.89 and 0.92). Finally, if clinicians were only happy to accept a 99% agreement between strategies, 31% of patients would still be spared from administration of adenosine if iFR and FFR were used in a staged approach (Figure 4 and Figure 5).
CLINICALLY REPRESENTATIVE STUDY POPULATION
The results of our study are relevant to the daily clinical application of physiological interrogation of angiographic intermediate stenoses, as our sample was formed by two independent populations of patients undergoing clinical FFR measurement from sites in Europe and Asia8,9. Importantly, patients in this sample were not specifically recruited for a research study, and therefore reflect the daily clinical practice of physiological interrogation of angiographically intermediate coronary stenoses. Because the majority of our patients had physiologically intermediate stenoses straddling the FFR treatment cut-off (mean FFR of 0.81, with 80% of FFR values falling between 0.6 and 0.9), 43% of them would still have to receive adenosine for a 95% agreement with an FFR-only strategy. It is likely that in other study populations, which included patients with more severe lesions (away from the intermediate range), even more patients would be free of adenosine for the same magnitude of agreement with an FFR-only strategy.
For instance, if we apply the same hybrid iFR-FFR strategy to the ADVISE study population7 (which had mean FFR of 0.72±0.2, with only 41% of stenoses between 0.7 and 0.9), using the same iFR values to defer and treat stenoses (>0.93 and <0.86, respectively) we would obtain a similar classification match with an FFR-only strategy (96%). However, the proportion of adenosine-free patients would significantly increase to 77%.
This example demonstrates that, in populations which include more patients with physiologically severe stenoses, such as the ones encountered in the DEFER1 (mean FFR 0.73), FAME2 (mean FFR 0.71) and FAME II3 (mean FFR 0.68) studies, the application of a hybrid iFR-FFR strategy is likely to free a proportionally higher percentage of patients from adenosine.
ALLOWING FOR AN FFR 0.75-0.8 GREY ZONE
The analysis presented in this study was performed using a fixed FFR cut-off of 0.8, as mandated by current clinical guidelines10,12 as a result of the FAME2 and FAME II3 studies. However, the DEFER trial1 and, more importantly, its 5-year follow-up results11, left little doubt about the safety of deferring stenosis with FFR ≥0.75. This overlap between FAME and DEFER FFR cut-offs is the widely acknowledged 0.75-0.8 FFR grey zone17, within which it is both mandated to treat, and known to be safe to defer, coronary lesions.
Therefore, if clinicians opt to use a hybrid iFR-FFR strategy which accounts for this FFR grey zone, the number of patients free of adenosine would increase to 76% (Figure 8). For this purpose, an iFR value of >0.90 could be used to defer revascularisation in stenoses (with 94% negative predictive value to exclude stenoses with FFR <0.75), whilst an iFR value of <0.86 would be used to treat stenoses (with a 93% positive predictive value to identify stenoses with FFR ≤0.8).
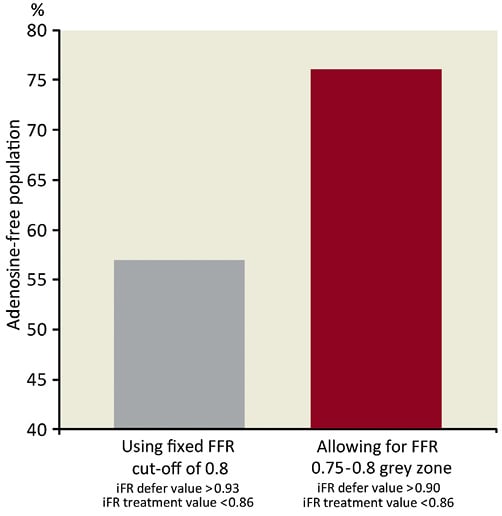
Figure 8. Adenosine-free population increases if FFR grey zone is accounted for: if the widely acknowledged FFR 0.75-0.8 diagnostic grey zone is accounted for, the proportion of patients free of adenosine in a hybrid iFR-FFR strategy would increase to 76%. In this scenario, a deferral iFR value of >0.90 could be used with a negative predictive value of 94%, maintaining an overall agreement with FFR-only strategy of 95%.
DISAGREEMENT BETWEEN STRATEGIES IS INFREQUENT AND OF SMALL MAGNITUDE
The overall 95% agreement between the hybrid iFR-FFR strategy and the FFR-only strategy in practice means that only one in 20 stenoses would have a different classification with the two approaches. Although this number is small (95% agreement between test modalities being unusual in clinical practice), it is still clinically relevant to understand the magnitude of such disagreement, when it occurs.
At the upper range of iFR values (negative iFR), disagreements only represented 3.1% of the overall population (18 out of 577 cases). Out of those cases, 67% (12) fell within the FFR grey zone of 0.75-0.8 and only in three cases FFR was <0.7. At the lower range of iFR results (positive iFR), disagreements represented only 1.7% of the overall population. Out of those cases, in 60% FFR fell between 0.8 and 0.85, and only one above 0.88.
Therefore, given the small magnitude of disagreement between strategies compared with the range of uncertainty within trial-based FFR-guided management itself, it might be speculated that classification of the small number of lesions differently by the hybrid iFR-FFR strategy from the FFR-to-all strategy will not have a significant effect on the risk of cardiac events. The scope for such small disagreements would need to be seen in the context of the opportunity for bringing rapid, symptom-free physiological targeting of PCI to a significantly higher number of patients with coronary disease.
FUTURE STUDIES
The relationship between iFR and FFR across different study populations reveals that the majority of differences in stenosis classification occur close to the iFR and FFR cutpoints, which could potentially have little or no effect on patient outcome8. However, prior to the application of a single dichotomous iFR cutpoint and implementation of iFR in clinical practice as an independent method to guide coronary revascularisation, clinical studies are warranted to demonstrate the safety and efficacy of iFR. Until such studies clarify the usefulness of iFR as an independent diagnostic modality, a hybrid iFR-FFR strategy provides a pragmatic strategy to increase adoption of physiology-guided revascularisation in the catheter laboratories.
LIMITATIONS
This study was a retrospective analysis performed on data collected from two clinical cohorts of patients who underwent FFR evaluation, using different doses and routes for adenosine administration. The proposed hybrid iFR-FFR revascularisation strategy was not tested prospectively against clinical outcomes. The positive side of this real-world, retrospective analysis is that our proposed FFR-only strategy (with varying doses of adenosine) reflects the clinical practice of interventionists in catheterisation laboratories across centres in Europe and Asia.
The comparison between the classification of coronary stenoses by the two revascularisation strategies was made without an independent discriminator, such as a non-invasive perfusion modality or invasive coronary flow. Therefore, when strategies disagreed in classifying a lesion as significant/non-significant, it is not possible to infer which of them correctly identified or excluded flow-limiting lesions.
Conclusions
Whilst we await the results of clinical trials which evaluate efficacy of iFR as a sole method to guide coronary revascularisation, a hybrid decision-making revascularisation strategy guided by iFR and FFR could drastically reduce the need for adenosine administration in clinical practice and maintain a high diagnostic agreement (≥95%) with FFR classification of stenoses. Therefore, the adoption of a hybrid iFR-FFR approach could expand the utilisation of physiology-guided revascularisation in clinical practice and improve patient outcome.
Funding sources
This study was funded by the National Institute for Health Research (NIHR) and Imperial College Healthcare NHS Trust Biomedical Research Centre. R. Petraco (FS/11/46/28861), J.E. Davies (FS/ 05/006), D.P. Francis (FS 04/079) and K.N. Asrress (FS/11/43/28760) are British Heart Foundation fellows. S. Sen (G1000357) and S.S. Nijjer (G1100443) are Medical Research Council fellows. C. Di Mario is a senior NIHR investigator.
Conflict of interest statement
J.E. Davies and J. Mayet hold patents pertaining to this technology, which is under licence to Volcano Corporation. J.E. Davies is a consultant for Volcano Corporation. The other authors have no conflicts of interest to declare.

