Abstract
The pressure wire has revolutionised cardiology by moving the focus of revascularisation from anatomy to physiology. This review provides a comprehensive viewpoint on the foundations of the field of intracoronary physiology, with emphasis on the development and clinical evidence of fractional flow reserve (FFR). Additionally, we critically appraise clinical decision making based on the evolving area of resting coronary physiology. The emerging role of coronary flow reserve and its complementariness with FFR is also discussed, and the importance of the invasive assessment of the coronary microcirculation in outlining prognosis is put into perspective. Overall, this review summarises the capacity of invasive coronary physiology indices to guide revascularisation and to discriminate patients at high risk of an adverse cardiovascular outcome.
Introduction
The pressure wire has revolutionised interventional cardiology by moving the focus of revascularisation from anatomy to physiology. This review provides a comprehensive viewpoint on the foundations of the intracoronary physiology field, critically appraises clinical decision making based on fractional flow reserve (FFR) and the evolving area of resting coronary physiology, puts into perspective the re-emerging role of coronary flow reserve and its complementariness with FFR, and finally describes some aspects of the importance of the invasive assessment of the coronary microcirculation. Overall, this review summarises the capacity of invasive coronary physiology to guide revascularisation and to discriminate patients at high risk of an adverse cardiovascular outcome (Table 1).
Past of the pressure wire
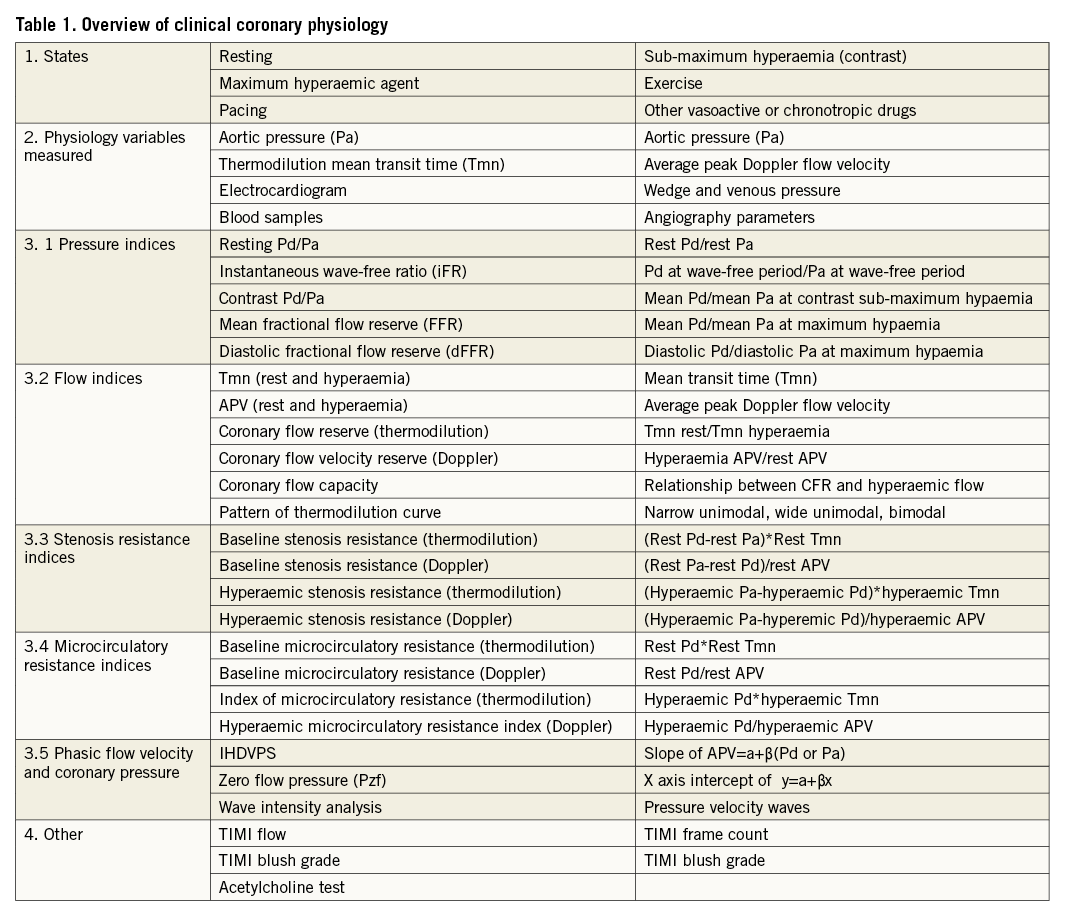
For those who were medical students in the 1970s, the complex equation of Donald Young was the best approach to understand coronary physiology as described in his landmark paper in Circulation Research (Figure 1)1. Soon after, several authors applied these equations2, but it was not until 1978 that Lance Gould firstly determined the applicability of these equations to vasoactive coronary arteries in the awake animal and secondly proposed a simplified and generalised form of the equations3. The Poiseuille principle was represented in the equation by the viscous friction (f) between layers of flow, and Bernoulli’s principle by the loss of kinetic energy at the exit of the lesion, with vortex formation as a result of the separation (s) of laminar layers of flow. R. Kirkeeide popularised the equation in 1986, by introducing quantitative coronary angiography exit angle, entry angle and reference and minimum lumen areas; the drop of pressure could be inferred from the equation4. For those who like historical proof, in 1988 in the American Journal of Cardiology the haemodynamic results immediately after stenting were reported for the Bernoulli and Poiseuille resistance at coronary flows of 0.5, 1 and 3 ml/sec5.
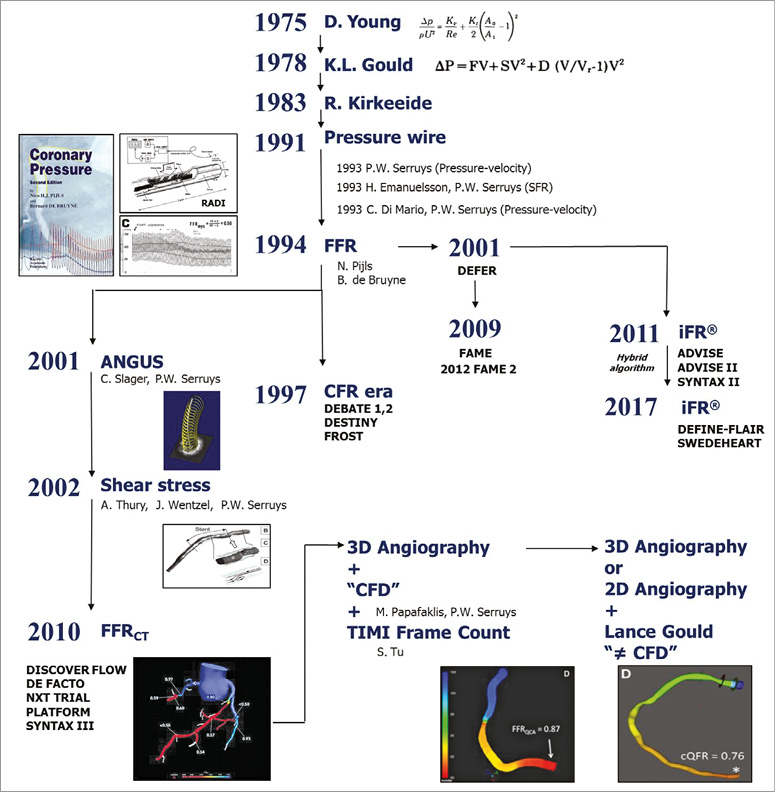
Figure 1. A helicopter view of the field of coronary physiology, its development and ramifications.
Around 1987, the Doppler wire was introduced and, although we could measure coronary flow velocity and coronary flow reserve (CFR)6,7, it quickly became unclear which was the CFR criterion for normality8. In animal models, it was in the range of 4 to 5 but after the first human studies we saw the emergence of various CFR cut-offs. We may have forgotten, but important trials such as DEBATE I, II and DESTINY combined percent diameter stenosis with CFR to improve clinical decision making and help define which lesions could be safely deferred from percutaneous coronary intervention (PCI)9,10.
The introduction of the pressure wire in 1991 by a Swedish company, RADI, ushered in a new era of coronary physiology. The work of Nico Pijls on coronary collaterals in dogs inaugurated the FFR era11. It took him some time to move from coronary collaterals to FFR but, together with Bernard de Bruyne, he was able to evaluate the diagnostic accuracy of FFR against exercise testing, thallium scintigraphy and stress echocardiography12. DEFER in 2001, FAME in 2009 and FAME 2 in 2012 translated the FFR concept from the bench to clinical practice, and finally, FFR has become an accepted parameter by the interventional community for clinical decision making13-15.
In parallel to this rather simple FFR measurement, on both sides of the Atlantic, in Stanford, Boston and Rotterdam, techniques combining intravascular ultrasound and angiography were developed (the so-called ANGUS) able to measure shear stress in human coronary arteries16. It was a tedious and cumbersome procedure, since it involved a three-dimensional (3D) reconstruction of the vessel (with the correct positioning of the intravascular ultrasound cross-section on the centreline of the vessel filmed in biplane angiography), the creation of a mesh of finite elements, calculation of shear stress and drop in pressure. Around 2010, the community was “destabilised” by the introduction of FFR derived from computed tomography angiography (FFR-CT). This technology was developed by HeartFlow under the leadership of Charles Taylor, and a series of trials popularised the colour-coded assessment of FFR-CT17. Around the same time, we were also “destabilised” by the introduction of the instantaneous wave-free ratio (iFR) by Justin Davies, looking into diastole, where microcirculatory resistance is stable18,19. iFR triggered many debates, because for the pioneers it was difficult to be challenged by a new technique not based on their “credo” – that both the epicardial vessel and microcirculation have to be fully dilated to assess the stenosis. Credit has to be given to the pioneers of the iFR, because very quickly they moved from ADVISE I and II, small clinical trials, to the large randomised DEFINE-FLAIR and iFR-SWEDEHEART studies, aiming as trialists to evaluate the rate of major adverse cardiac events (MACE) with FFR or iFR guidance19-22.
History is still not complete, since the colourful FFR-CT has triggered, in the most conventional field of angiography, attempts to create pseudo-FFRs, by combining angiographic data with computational fluid dynamics, including the Lance Gould equation. In 2014, the Boston group, together with Rotterdam and Ioannina, and Shengxian Tu, published the first non-commercial academic angiography-derived FFR, the so-called quantitative flow ratio (QFR)23. Whether large corporations will succeed in putting this technology online remains to be seen. While, at present, in 2017, it might look like we are going in circles, the reality is that we have made real progress in assessing the physiology of the coronary artery.
Present of the pressure wire
FRACTIONAL FLOW RESERVE
CONCEPT
In 1993, Piljs et al described and experimentally validated the theoretical basis for the calculation of coronary flow from coronary pressure in the different components of the coronary circulation11. Here, it was shown that, at maximal hyperaemia, the ratio of distal-to-aortic pressure in a stenosed coronary artery was linearly and strongly correlated to the ratio of stenotic-to-normal mean arterial Doppler-derived blood flow velocity (Figure 2). Consequently, the authors suggested that the derivation of flow reserve from pressures was possible. This was a dramatic step forward in the field, because coronary pressure is easier to measure than coronary flow. FFR was herein defined as the maximum achievable flow in the presence of a stenosis divided by the maximum flow expected in the same distribution in the absence of a stenosis11. Then, and because of the linear relationship between pressure and flow during hyperaemia, it was evidenced that FFR could be inferred from pressure, as the ratio of distal pressure (Pd) to aortic pressure (Pa) during maximum hyperaemia, assuming a negligible venous pressure. This elegant and clinically meaningful theory provided FFR with very useful characteristics. For example, the highest possible FFR value is 1.0, which denotes a normal epicardial conductance. An FFR value of 0.70 implies that the maximum flow to the distal myocardium only reaches 70% of what it would be if the artery were to be normal11. FFR takes into account the contribution of collaterals, is little influenced by systemic haemodynamics (although this argument has recently been challenged24), has reached a single cut-off prospectively validated in randomised trials, and displays a continuous relationship with MACE, such that the largest risk and revascularisation benefit accumulates in the most severe lesions11,25. All of these have made FFR an excellent index for clinical decision making in the catheterisation laboratory.
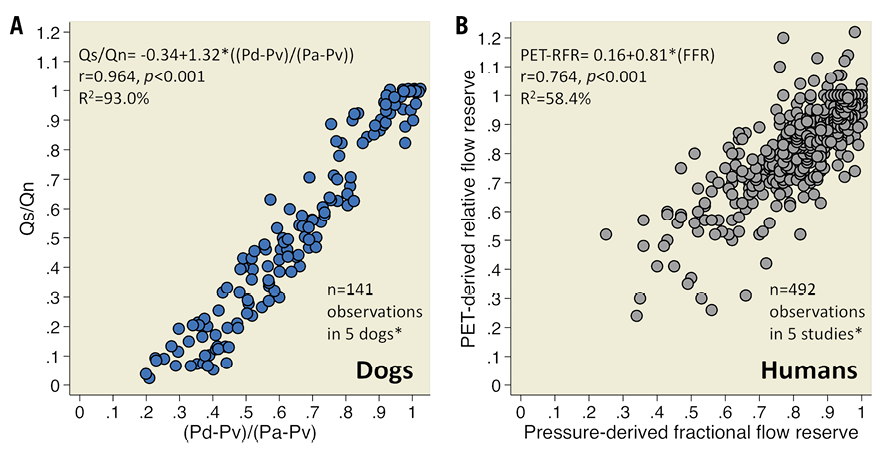
Figure 2. Derivation of relative flow reserve from pressure. Summary of the relationship between relative flow reserve (RFR) and pressure-derived FFR in experimental and human studies. Individual data points were manually extracted from available scatters with dedicated software. Regressions are hence approximate*. Panel A summarises the five dogs of the FFR validation experiment11. Panel B summarises all available peer-reviewed scatters of the relationship between PET-derived RFR and FFR in humans32,47-50. A total of 563 vessels were included in these studies. However, only 492 (87.4%) vessels could be extracted and included in the Figure.
EVIDENCE
FFR revolutionised cardiology by moving the focus of revascularisation from anatomy to physiology (Figure 3). The three most important FFR trials are DEFER, FAME and FAME 2. In DEFER, if FFR was ≥0.75, patients with coronary artery disease (CAD) and intermediate stenosis were randomly assigned to deferral (n=91) or performance (n=90) of PCI13. If FFR was <0.75, PCI was performed (n=144). Event-free survival at five years was not different between the defer and perform groups (80% and 73%, respectively; p=0.52). Moreover, the risk of cardiac death or myocardial infarction related to FFR ≥0.75 stenosis was <1% per year, and not decreased by stenting. FAME randomised 1,005 patients with multivessel CAD to FFR-guided or angiographically guided complete PCI14. The MACE-oriented primary endpoint was 18.3% in the angiography group and 13.2% in the FFR group (p=0.02). FAME demonstrated that FFR-guided PCI results in better clinical outcomes as compared to angiography-guided complete PCI. FAME 2 hypothesised that, in patients with FFR-significant stenoses, PCI plus optimal medical therapy would be superior to medical therapy alone15. The study was positive and recruitment halted prematurely (n=1,220, ±54% of projected sample size), because of a significant difference in the percentage of patients who had a primary endpoint event (4.3% in the PCI group versus 12.7% in the medical therapy alone group, p<0.001), which was mostly driven by a lower rate of urgent revascularisation in the PCI group15. Altogether, these trials demonstrated that deferral of PCI on the basis of FFR is safe at long term and that FFR-guided PCI improves patient outcome as compared to medical therapy alone and angiography-guided PCI. These are the reasons why FFR received a class 1A recommendation in the 2014 ESC EACTS guidelines on myocardial revascularisation for the identification of relevant stenosis when evidence of ischaemia is not otherwise available26.
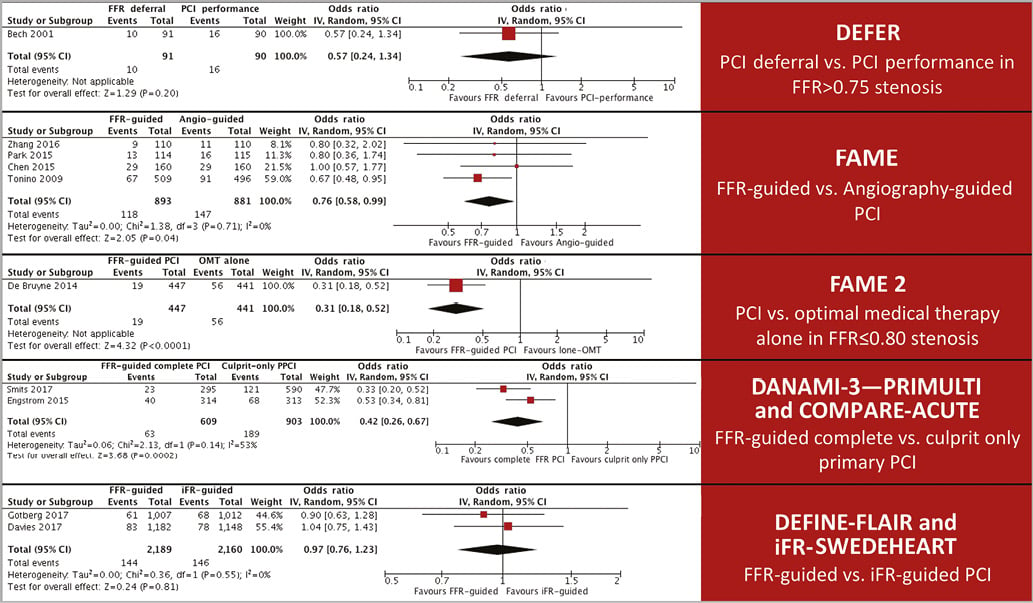
Figure 3. FFR-randomised trials. Summary of all published FFR-randomised clinical trials with MACE as primary endpoint13-15,21,22,51-55. MACE of each individual study were combined with the random-effects model based on the DerSimonian and Laird method (RevMan 5.2 software) because of different inclusion criteria. FFR-guided PCI was associated with a lower risk of MACE compared to angiography-guided PCI and optimal medical therapy alone. FFR-guided complete PCI was also associated with a lower risk of MACE compared to culprit-only primary PCI. No differences were observed in the rate of MACE between FFR- and iFR-guided PCI.
LIMITATIONS
The FFR model applies only during maximum hyperaemia when all resistances are constant and the derivation of flow reserve from pressure is possible11. The development of “true maximum hyperaemia” in clinical practice, however, is hampered by several factors, including a heterogeneous response to vasodilator agents and the functional status of the microcirculation. Indeed, only 84% of patients achieve “maximum“ hyperaemia with intravenous adenosine when compared to intracoronary papaverine27, and the functionality of the microcirculation may raise concerns, particularly in patients suffering from acute coronary syndromes, where local neurohumoral reflexes, epicardial spasm, microvascular vasoconstriction, compression and plugging, and elevated left ventricle end-diastolic pressure may lead to transitory microcirculatory dysfunction (MCD) in culprit and remote myocardial beds28. This is of paramount importance, because the proportion of patients with acute coronary syndromes undergoing catheterisation is steadily increasing worldwide28.
Another fundamental limitation of FFR stems from its lone-pressure nature. Although coronary pressure and flow are closely related, flow is primarily more important for the maintenance of myocardial function25. It should be emphasised that FFR was designed to assess the relative contribution of the stenosis to the overall degree of myocardial flow impairment11. If myocardial flow is truly impaired in the myocardium, however, it cannot be known from FFR alone25,29. That is to say, even if a stenosis is contributing significantly to myocardial flow impairment (i.e., FFR ≤0.80), the maximum achievable flow might suffice to avoid ischaemia. On the other hand, even if a stenosis is not contributing significantly to myocardial flow impairment (i.e., FFR >0.80), the maximum achievable flow might not suffice and ischaemia may be present (Figure 4). Both conditions are not anecdotal and could exist in as many as 30% of clinically assessed vessels29. These limitations of FFR theory indicate room for further refinement and clearly support the need for a more comprehensive invasive diagnosis of CAD.
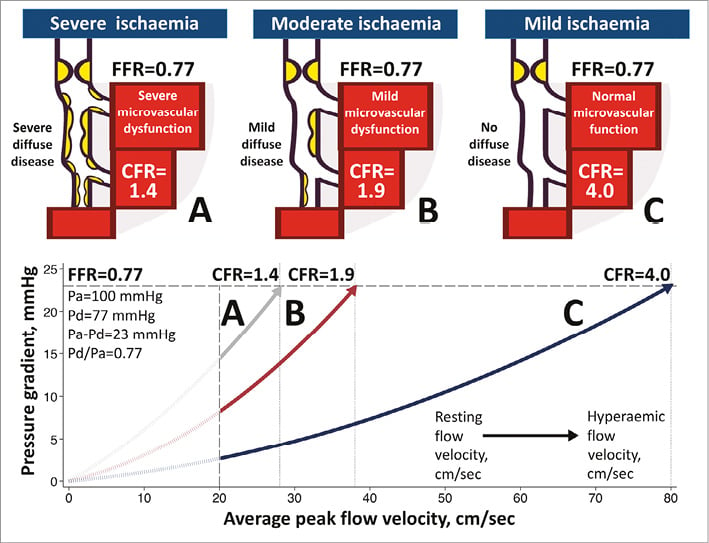
Figure 4. FFR and CFR discordance. This figure conceptually illustrates three scenarios of a same hypothetical FFR value within the FFR grey zone. In vessel C, diffuse and microvascular disease are minimal. CFR is normal and ischaemia unlikely. Vessel B represents the most common case, where moderate diffuse and microvascular disease contribute, in addition to the stenosis, to exhausting the CFR. Vessel A is highly affected by diffuse and microvascular disease. Here, CFR is severely exhausted and profound ischaemia highly likely, even if FFR is only moderately affected.
INSTANTANEOUS WAVE-FREE RATIO
CONCEPT
In 2010 it was recognised that the resting Pd/Pa ratio was strongly correlated with FFR30. At that time, Davies et al had already shown how wave intensity analysis could be used to identify and quantify the pressure-velocity waves in normal human coronary arteries18. A detailed analysis of these waves in stenosed coronary arteries was later performed by Sen et al, who identified that, during mid to late diastole, there is a finite period of time where the formation of new pressure-velocity waves is absent19. Within this wave-free period, the authors observed that microvascular resistance was lower than mean whole-cycle resting resistance, and not statistically different from mean hyperaemic whole-cycle resistance. Moreover, the coefficients of variation of the wave-free microvascular resistance and the hyperaemic whole-cycle resistance were not significantly different. Therefore, the authors postulated that, during the wave-free period, microcirculatory resistance is naturally stable and minimised which, as discussed above, are the theoretical prerequisites for the derivation of flow reserve from pressure. The iFR was therefore proposed as a vasodilator-free index of stenosis severity comparable to FFR, and defined as the ratio of mean Pd to mean Pa both during the wave-free period19.
EVIDENCE
Several groups put iFR through scrutiny. Most of these were summarised in RESOLVE, a comprehensive (n=1,593 retrospective pressure traces) core-laboratory analysis of the diagnostic accuracy of iFR and resting Pd/Pa against FFR31. RESOLVE documented a moderate linear relationship between both iFR and Pd/Pa with FFR (R2=0.66 and 0.69, respectively), with an overall, and non-statistically different, diagnostic accuracy of ~80% for both non-hyperaemic indices. RESOLVE results were similar to the findings of the meticulous and prospective ADVISE II study20, that permits to conclude that the iFR and FFR relationship in clinical populations is weaker than that reported in the original iFR description, and that, for FFR diagnosis, iFR is not statistically superior to resting Pd/Pa20,31. In this interpretation, however, it should be kept in mind that, despite the clinical benefits of FFR, there is no gold standard for the detection of myocardial ischaemia, and that many other ischaemia tests are also supported by vast outcome data. Investigators thus decided to evaluate the diagnostic accuracy of iFR, Pd/Pa and FFR against alternative arbiters of myocardial flow impairment (Figure 5)32-34. Notably, and as compared to most of the alternative tests, both iFR and Pd/Pa were found to be non-inferior to FFR for the detection of ischaemia-generating stenosis. This strongly suggests that resting pressure indices provide enough – although physiologically incomplete – information for appropriate triggering of revascularisation. JUSTIFY CFR, the largest (n=216) of these studies, demonstrated that, of all pressure indices, iFR had the highest diagnostic accuracy against CFR, and that, as compared to Pd/Pa, iFR was statistically better for detecting an exhausted flow reserve34. This is important because CFR is emerging as a powerful tool for MACE discrimination25. This higher agreement with CFR, a larger range of possible values and a smaller vulnerability to pressure drift made iFR the best resting index for randomised clinical testing.
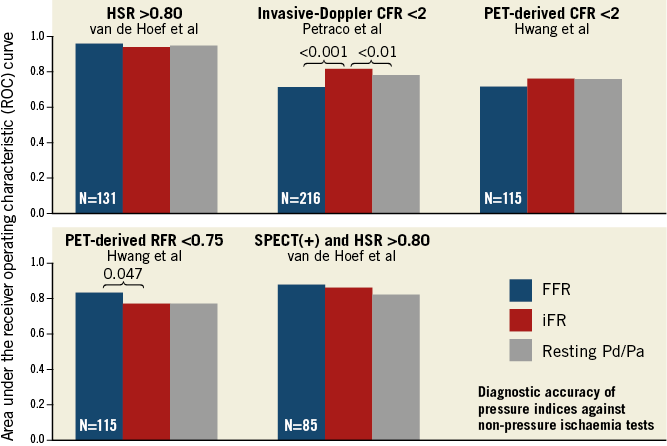
Figure 5. Diagnostic accuracy of pressure indices against non-pressure ischaemia tests. All published studies comparing the diagnostic accuracy of FFR, iFR and resting Pd/Pa against non-pressure ischaemia tests are summarised in this Figure33,34,50,56. Only p<0.05 are shown. HSR: hyperaemic stenosis resistance; SPECT: single photon emission computed tomography; PET: positron emission tomography
The effectiveness of iFR to guide revascularisation, as compared to FFR, was put to the test in DEFINE-FLAIR and iFR-SWEDEHEART, the largest coronary physiology randomised clinical trials performed to date21,22. Herein, >4,500 patients were randomised in two different studies in a 1:1 fashion to either iFR-guided or FFR-guided PCI, with iFR ≤0.89 and FFR ≤0.80 as pre-specified treatment thresholds. Both studies were designed to show the non-inferiority of iFR to FFR with respect to the subsequent risk of MACE. The primary endpoint, a composite of death from any cause, non-fatal myocardial infarction, or unplanned revascularisation at one year, occurred in DEFINE-FLAIR and iFR-SWEDEHEART, in 6.8% and 6.7% in the iFR groups, and in 7.0% and 6.1% in the FFR groups, respectively. Since the differences in event rates fell within the trials’ pre-specified non-inferiority margins, it can be concluded that revascularisation guided by iFR is non-inferior to revascularisation guided by FFR with respect to the risk of MACE at one year (Figure 6). Moreover, in the iFR groups, the number of functionally significant stenoses and rates of revascularisation were lower, the duration of the procedure was shorter, and the percentage of patients who reported adverse procedural symptoms was smaller. These additional advantages and the robustness of the two trials have set the basis for the inclusion of iFR as an appropriate substitute for FFR in the recent ACC 2017 Appropriate Use Criteria for Coronary Revascularization in Patients With Stable Ischemic Heart Disease35.
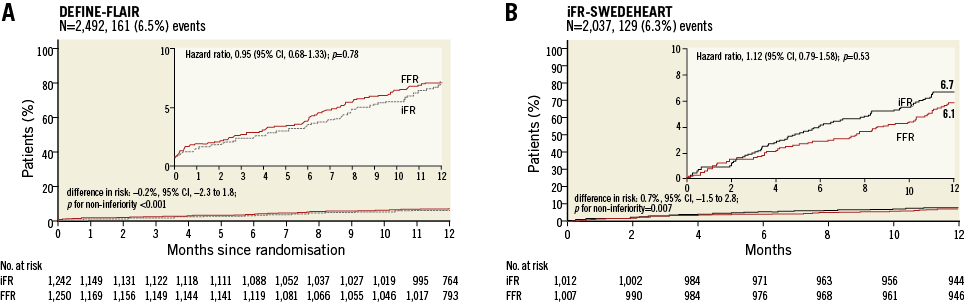
Figure 6. iFR as tool to guide revascularisation. Cumulative risk of the composite of death from any cause, non-fatal myocardial infarction, or unplanned revascularisation at one year in DEFINE-FLAIR (A) and iFR-SWEDEHEART (B). Reprinted with permission from Davies et al and Götberg et al21,22.
LIMITATIONS
Shortly after its introduction, the foundation premises of iFR were challenged and not reproduced in a larger cohort of human coronary arteries. Here, wave-free resting microvascular resistance significantly and consistently exceeded mean whole-cycle hyperaemic resistance36. Whilst a definitive answer to this conundrum is lacking, it seems that the most plausible explanation is a significant difference in the physiology severity of the investigated vessels19,36. A report from the Iberian-Dutch-English (IDEAL) collaborators sheds some light on this issue, by demonstrating in humans how, with progressive anatomic stenosis severity, trans-stenotic pressure gradient increases, hyperaemic flow decreases, while resting coronary flow is maintained, by compensatory reduction in microvascular resistance37. Additionally, hyperaemic microvascular resistance remains unchanged with increasing stenosis severity, whereas resting microvascular resistance decreases, to levels as low as those achieved with hyperaemia. Thus, resting microvascular resistance will fall dramatically in response to vasodilators in mildly stenosed vessels while it will not decrease further in tightly stenosed vessels. Whether these findings explain the above-mentioned conundrum on the iFR foundation premises remains to be proved. An interesting proposal of the IDEAL investigators is that, since resting flow is preserved at the expense of distal coronary pressure, changes in distal pressure could represent to what degree the stenosis is exhausting autoregulation, and could hence represent the true physiological impact of the stenosis in the distal myocardium37. This argumentation provides further support for the use of resting indices but should be challenged by future research.
CFR AND FFR ASSESSMENT
EMERGING PROGNOSTIC ROLE OF CFR
CFR is the ratio of hyperaemic to baseline flow, and reflects the capacity of both the epicardial vessel and the microcirculation to satisfy demand, by increasing flow25. Therefore, and because CFR interrogates the coronary circulation as a whole, CFR can identify whether, and in spite of an epicardial stenosis, myocardial flow supply is or is not normal. This is a key diagnostic characteristic, intimately related to risk, because ultimately myocardial function thrives on flow, as assessed by CFR, and not on perfusion pressure, as assessed by FFR25,29. This physiology foundation has received reassuring sustenance from a wealth of clinical data (Figure 7). For example, in a large clinical cohort (n=2,783) investigated with positron emission tomography, a CFR <1.5 was associated with an univariate 16-fold increased risk in mortality at medium term, as compared to a normal flow supply (CFR >2)38. In a different study, where 4,313 patients with known or suspected CAD were evaluated with stress echocardiography including CFR evaluation of the left anterior descending artery, the four-year mortality was markedly higher in patients with CFR ≤2, in both the group with (39% vs. 7%, p<0.001) and the group without (12% vs. 3%, p<0.001) inducible ischaemia, as compared to patients with preserved flow supply (CFR >2)39. Since the capacity of CFR to stratify the risk for mortality hence extends beyond the presence or absence of stress-induced ischaemia – the ultimate objective of FFR – little doubt now exists on the incremental information that CFR provides to FFR assessment.
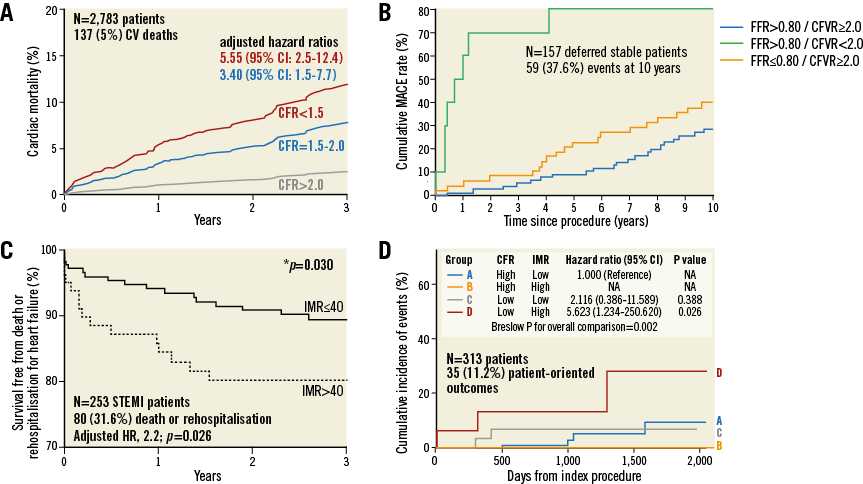
Figure 7. Risk discriminative capacity of CFR and IMR. Murthy et al38 (A), van de Hoef et al42 (B), Fearon et al44 (C), and Lee et al45 (D) provide supportive data for CFR and IMR as tools for risk discrimination. CFR: coronaray flow reserve; CVFR: Coronary flow velocity reserve; IMR: index of microvascular resistance. All reprinted with permission.
CONTEMPORARY REINTERPRETATION OF THE FFR AND CFR RELATIONSHIP
FFR and CFR were both envisaged to estimate coronary stenosis severity. However, it was quickly evidenced that FFR and CFR disagree in around 30% of vessels (Figure 8)29,40. A recent model proposed by Johnson et al suggests that this discordance is not due to methodology but is rather a consequence of the complex interaction between focal stenosis, diffuse atherosclerosis and MCD29. Figure 8 explains this model. A non-ischaemic lesion will be characterised by both adequate and concordant FFR and CFR (red in Figure 8). A severe flow-limiting stenosis (blue in Figure 8) will exhaust flow supply (CFR <2), because autoregulation cannot compensate for high epicardial resistance (FFR ≤0.80). In the discordant group with FFR ≤0.80 and CFR ≥2, the theoretical substrate is a focal lesion with minimum diffuse disease and a functionally preserved microcirculation. A CFR >2.0 would reflect that flow supply suffices to avoid ischaemia, even if FFR is ≤0.80 (orange in Figure 8). Finally, the discordant group with FFR >0.80 and CFR <2 would be explained by predominant diffuse atherosclerosis (yellow in Figure 8) or MCD if the pressure loss is trivial (<5 mmHg) (grey in Figure 8). In this quadrant, the flow supply is significantly impaired (CFR <2) and ischaemia highly likely, even if the relative contribution of the stenosis to the overall degree of flow impairment is only minor (FFR >0.80). On the basis of the preserved myocardial function at low perfusion pressures when flow remains sufficient, and of the above-mentioned encouraging clinical data for preserved CFR, the ongoing DEFINE-FLOW study (clinicaltrials.gov NCT02328820) hypothesises that deferring revascularisation in stenosis with low FFR but preserved CFR is safe. Results are expected in one year.
ASSESSMENT OF THE CORONARY MICROCIRCULATION
A sizeable body of evidence nowadays substantiates how the coronary microcirculation contributes to ischaemia and influences patient symptoms and outcomes. For example, more than half of women and around one third of men with stable angina undergoing coronary angiography are found to have non-obstructive CAD41. MCD seems to account for at least one third of these cases41. Furthermore, the quality of life of patients with MCD is significantly affected, as >40% are admitted for recurrent angina28,41. This means high healthcare costs, similar to those of obstructive CAD41. Although some non-invasive tests inform on the functional status of the coronary microcirculation, its most certain evaluation remains invasive, because non-invasive techniques cannot differentiate between epicardial and microvascular disease.
The first technology able to assess intracoronary flow in humans was Doppler-flow velocity, and most of our basic understanding of the function of the coronary artery and microcirculation in health and disease stemmed from these sensors28. Although its clinical use is still limited by a difficult acquisition of appropriate signals, recent studies are renewing interest in the technology28,42. For example, a recent study (n=160) observed that the Doppler-derived hyperaemic microcirculatory resistance index measured immediately after primary PCI was a strong independent predictor of microvascular injury defined with cardiac magnetic resonance and MACE at three years43. The second available technology capable of assessing coronary flow is the thermodilution method28. Advantages over Doppler-flow velocity are its technical ease and a better correlation with absolute coronary flow. The thermodilution-derived index of microcirculatory resistance (IMR) is reproducible, and mounting evidence supports its value as a meaningful diagnostic tool (Figure 7). In patients with acute myocardial infarction, high IMR values are associated with larger infarct size, worse wall motion scores, and decreased myocardial viability and left ventricle recovery28. A multicentre study (n=253) of patients with ST-elevation myocardial infarction observed that patients with IMR >40 U immediately after primary PCI had higher rates of death or re-hospitalisation for heart failure at one year than patients with IMR ≤40 (17.1% versus 6.6%, p=0.027)44. Likewise, a recent prospective natural history study of stable patients (n=313) with CAD and FFR-negative stenosis addressed the prognostic capacity of CFR and IMR45. Herein, both CFR and IMR improved risk stratification, and patients with low CFR and high IMR had a worse prognosis. IMR thus seems capable of correctly discriminating patients at higher risk, in both acute and stable clinical settings. It is important to state, however, that, as with all intracoronary physiology tests, the coronary thermodilution method carries intrinsic limitations, such as a high sensitivity of the measurements to the displacement of the sensor, an inherent variability in the thermodilution curve, and the necessity of an adequate mixture of the indicator with blood before the bolus reaches the sensor. Finally, and in spite of the growing evidence supporting the value of the invasive assessment of the coronary microcirculation (especially with microcirculatory resistance indices), specific treatment options for MCD are very limited.
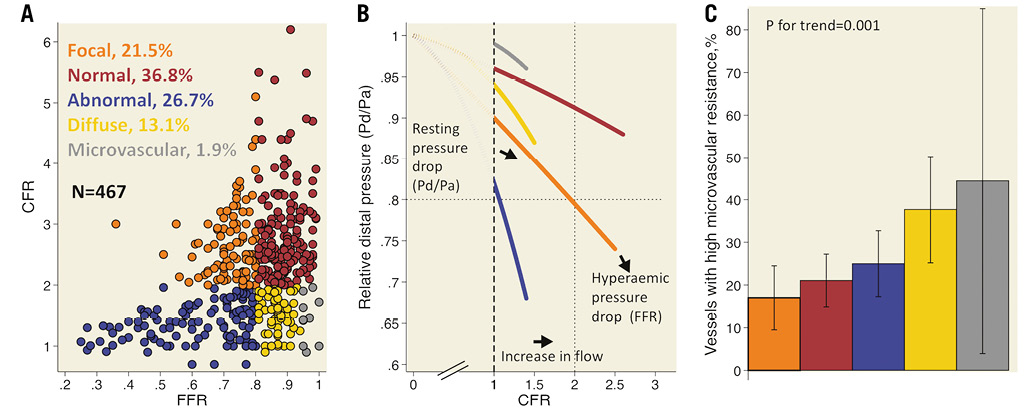
Figure 8. CFR and FFR relationship. Synopsis of 467 vessels: 299 assessed with Doppler in the AMC Heartcentre, Amsterdam, the Netherlands; 167 assessed with thermodilution in the Hospital Clínico San Carlos, Madrid, Spain. Panel A shows the overall CFR and FFR relationship, with CFR <2 and FFR ≤0.80 as cut-offs. Panel B exhibits a quadratic fit that starts at a hypothetical zero flow and zero pressure drop, crosses the vertical dotted line at the median resting Pd/Pa observed in each category, and ends at each category median CFR and FFR values. Panel C shows the prevalence of vessels with high microcirculatory resistance (above the 75th percentile in each Doppler and thermodilution data set) in the CFR and FFR regions. Modified with permission from: Coronary Stenosis Imaging and Physiology - ISBN 978-2-37274-007-4.
Future
Pressure guidewires are still used predominantly to ascertain the functional relevance of intermediate coronary stenoses. It is foreseeable that interrogation will be expanded to vessels with severe CAD to obtain relevant information to plan PCI. Intracoronary pressure mapping allows identification of the segments that contribute more to haemodynamic impairment caused by diffuse narrowing and that, therefore, should constitute the primary revascularisation target. This is facilitated by the use of resting indices such as iFR, which do not require hyperaemia and have less haemodynamic crosstalk between stenoses46.
Translation of intracoronary physiology findings to angiography-based actions, such as identification of the coronary segment to be treated and subsequent stent deployment, will be facilitated by co-registration of physiological data with angiography. Currently, this can be done with static coronary images, but technological improvements in dynamic roadmapping will most likely enable such physiological guidance to be performed also using moving images (Figure 9).
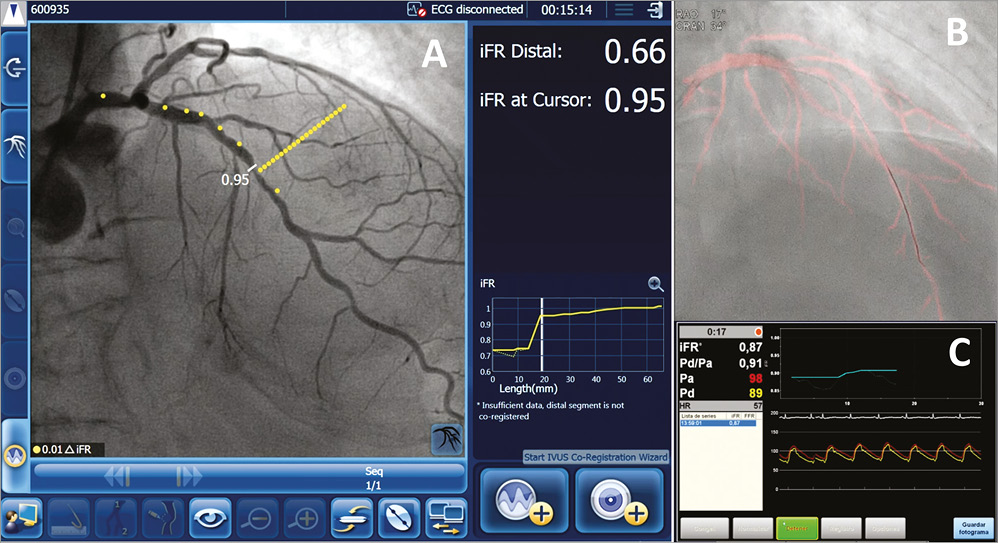
Figure 9. Future of the pressure wire. Panel A shows the result of co-registering iFR pullback data with coronary angiography in a left anterior descending coronary artery with several irregularities. Each yellow dot represents a modification of 0.01 iFR units. The co-registered image shows with clarity the vessel region accounting for most of the haemodynamic impairment, allowing identification of the PCI target segment and translation to angiography during stent deployment. Panel B and Panel C show an iFR pullback performed during dynamic roadmapping (pink colour moving mask generated from prior angiographic run), allowing clear correlation between changes in iFR and specific anatomical landmarks.
Physiological interrogation after PCI will be performed routinely to document the haemodynamic result of the intervention25. This might lead to further optimisation or to documenting the residual haemodynamic effect of non-treatable lesions.
Perhaps the major pending advance in clinical coronary physiology will be the adoption of a comprehensive assessment of the coronary circulation, which will address both the epicardial vessel and the microcirculation29,42. Previous paragraphs have discussed the advantages of this approach but, to be adopted by the majority of cardiologists, at least two requirements will have to be fulfilled. The first will be the availability of new user-friendly technologies for measuring coronary flow and calculating combined press-flow indices in the catheterisation laboratory. Current technologies for coronary flow estimation are too complex and time-consuming for most interventionalists, and are available on old guidewire platforms. Phasic information will be required to perform interrogation of specific intervals of the cardiac cycle. The second will be the existence of conclusive evidence supporting the benefit of such assessment for the patient.
One of the clinical scenarios in which physiological interrogation may potentially play an important role is in acute myocardial infarction. Recent and ongoing studies are investigating the potential value of FFR and iFR in assessing non-culprit stenoses in such patients. However, in addition, there is growing evidence that interrogation of the culprit vessel immediately after primary PCI with specific indices informs on the degree of microcirculatory and myocardial damage caused by ongoing myocardial no-reflow, which can occur despite the achievement of angiographic normal flow28. In particular, estimation of the zero flow pressure can be important, as this has been shown to be a predictor of myocardial damage28. Determining which therapeutic actions, implemented at the time of primary PCI or immediately after, may reduce myocardial damage constitutes an area of current interest28.
Over the last 10 years, the theoretical framework of FFR and iFR has been adopted by post-processing of coronary imaging, either non-invasive (FFR-CT) or invasive (QFR). It is quite likely that these techniques will be used to circumvent the limitations of planar coronary angiography in assessing functional stenotic relevance. Yet, as these approaches will not be able to address many of the advantages of invasive physiological assessment discussed above, it is foreseeable that the use of intracoronary guidewires fitted with sensors will continue to expand.
Conclusions
Coronary physiology indices are more than ever important for the interventional cardiologist. They allow a further refinement in the selection of revascularisation targets and have the potential to identify patients at high risk for MACE.
Authors’ perspective
Physiology has always been at the core of interventional cardiology and is now more than ever at the front line of the diagnostic and therapeutic evaluation. The field is evolving quickly and is exposed to a double tension: to simplify physiology as FFR and iFR have done, to foster its adoption and thus to translate to more patients the benefits that have been demonstrated in trials, or, on the contrary, to confront the intricacy of CAD, with combined pressure and flow indices. Which approach is the more successful remains to be seen.
Conflict of interest statement
M. Echavarria-Pinto has served as speaker at educational events organised by St. Jude Medical and Volcano Corporation. C. Collet reports a research grant from HeartFlow Inc. J. Escaned has served as speaker at educational events organised by St. Jude Medical and Volcano Corporation. J.J. Piek is a consultant for Philips/Volcano Corporation. P.W. Serruys is a member of the International Advisory Board of Abbott Vascular.