Coronary angiography remains the gold standard in the diagnosis of coronary artery disease in the cardiac catheterisation laboratory. However, the limitations of angiography for assessing epicardial stenosis severity led, in the 1990s, to the introduction of sensor-equipped guidewires that measure coronary pressure and flow selectively distal to a lesion1. The most frequently used parameter is fractional flow reserve (FFR), defined as the ratio of the pressure distal to a lesion relative to the aortic pressure that assumes minimal influence of the microvascular resistance during hyperaemic conditions2. An alternative is the assessment of coronary flow reserve (CFR), defined as the ratio of the distal hyperaemic flow relative to baseline flow3. CFR is considered to be less lesion-specific when compared to FFR as it is determined by the resistance of both the epicardial lesion and the distal microvasculature4.
The use of combined pressure flow measurements using a single wire (ComboWire®; Philips Volcano, Thornton, CO, USA) allows the calculation of the hyperaemic microvascular resistance index (hMVR)5,6. This allows two important observations to be made. The first is that there is a large variation in hMVR between patients in contrast to the assumption underlying the FFR concept7. Secondly, variation in hMVR significantly determines the pressure gradient across a lesion7. This is a fundamental observation, as it demonstrates that even the highest dose of adenosine infusion cannot increase blood flow to the severely diseased microcirculation. Thus, when evaluating the same stenosis when blood flow is low, the pressure gradient is low, whereas when blood flow is high the pressure gradient is high. Together, these findings suggest that the validation studies in healthy animals in FFR2 are overly simplistic, and cannot be translated directly to humans8.
FFR and CFR discordance
The distal pressure-flow measurements using wires equipped with both pressure and flow sensors show that every epicardial stenosis can be characterised according to its pressure-flow curve (Figure 1). The steepness of the curve indicates the severity of the lesion. However, the magnitude of the pressure gradient is dependent on the magnitude of maximal flow velocity. This behaviour of the coronary circulation according to pressure-flow relationship is relevant for the interpretation of FFR-CFR discordance9,10. A low hMVR may result in the combination of a normal CFR but abnormal FFR, whereas a high hMVR may result in the combination of a normal FFR but abnormal CFR, even though the curve remains the same11. This phenomenon explains the discordance between FFR and CFR that occurs in 30-40% of the patients with intermediate lesions9,12. Critically, discordance is driven by the flow velocity, which is determined by the degree of microcirculatory resistance.
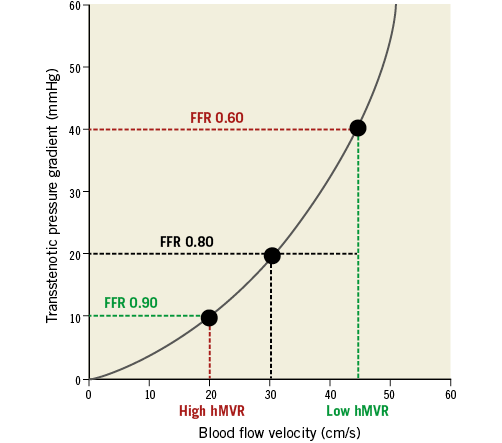
Figure 1. The transstenotic pressure gradient is determined by anatomical stenosis severity, hyperaemic microvascular resistance and coronary flow velocity characteristics.
The report in this issue of EuroIntervention from Young-Woo Seo et al13 confirms earlier findings between FFR and hMVR7.
In contrast to earlier angiographic studies, they used intravascular ultrasound for more accurate lesion assessment (minimal lumen area [MLA]) in combination with pressure-Doppler flow assessment. They also demonstrated a large variability in hMVR and its association with FFR whereby a low hMVR leads to a lower FFR and a high hMVR leads to a higher FFR. By dividing MLA and hMRV into tertiles they elegantly demonstrate the interactions between FFR, MLA and hMVR (Figure4 in Seo et al13). For any lesion assessed by MLA, there is a clear positive association between FFR and hMVR, in particular in the range of intermediate lesions (MLA 2.1-2.9 mm²) where it is most relevant for clinical decision making. This analysis provides further evidence that FFR is susceptible to the health and status of the vasodilatory response of the coronary microcirculation9,10.
The diagnostic triangle
This clinical decision making of coronary intervention should ideally be based upon an appropriate interpretation of the patients’ complaints, the results of non-invasive diagnostic testing as well as the result of intracoronary haemodynamic measurements for guidance of interventions. This diagnostic triangle should be the basis for our clinical decision making during cardiac catheterisation. In daily clinical practice, there is frequently a paucity of documentation of myocardial ischaemia prior to cardiac catheterisation. In the present report, it is notable that there is no information of non-invasive stress tests in the diagnostic workup of this well-equipped intervention centre. In the absence of non-invasive stress tests, an operator depends upon the interpretation of the complaints of the patients and the results of intracoronary diagnostic techniques to guide ad hoc coronary interventions. This approach requires an intimate knowledge of the limitations and pitfalls of the diagnostic techniques applied. The FAME trials14,15 reported the potential of FFR, leading to a class I indication, level of evidence A for clinical decision making in stenosis assessment. However, the results of FAME 2 also showed that 60% of the patients with lesions and an FFR <0.80, allocated to optimal medical therapy, did not require a PCI during a two-year follow-up period15, probably because of inclusion of non-flow-limiting lesions (low resistance and high flow) that did not induce myocardial ischaemia and thus exhibited a good long-term prognosis16. In this respect, it is important to note that the patient, and not the diagnostic technique, should always be considered as the gold standard.
Clinical implications
What do the results of the present study mean for our daily clinical practice? Next to FFR, the instantaneous wave-free ratio (iFR) has been introduced as a tool to measure the transstenotic pressure ratio during the wave-free period in diastole17. It is an attractive alternative to FFR because it does not require hyperaemia. The development of iFR has recently led to the reporting of two large, randomised, prospective multicentre clinical trials –DEFINE-FLAIR18, and iFR SWEDEHEART19. Both of these studies demonstrated in ~4,500 patients that iFR was non-inferior to revascularisation guided by FFR with respect to major adverse cardiac events (MACE) at one year18,19. Furthermore, a markedly lower incidence of patient discomfort and unpleasant side effects was reported in the iFR arm, as well as a significant 10% saving in procedural time.
Today, FFR and iFR are the most frequently used intracoronary haemodynamic parameters, based on evidence, availability and simplicity. However, unlike FFR, a number of key physiological properties of iFR limit it from being confounded by inter-patient variations in microvascular function, hMVR or hyperaemic flow velocity. Firstly, iFR is measured under basal conditions, thereby avoiding the need for a hyperaemic stimulus that is itself variable between patients. Secondly, resting coronary flow remains stable at ~20 cm/s across almost the entire range of stenosis severities, up to ~90% stenosis, where even resting flow profiles are impaired3,20.
In an analogy to the FFR-CFR comparison, a normal iFR may result in an abnormal FFR when hMVR is low and, similarly, an abnormal iFR may result in a normal FFR when hMVR is high. As is illustrated in the present report, the use of FFR in this diagnostic workup is debatable, as an abnormal FFR (<0.80) may coincide with a low hMVR, resulting in a normal coronary flow reserve (>2.0) and a normal iFR. Such a lesion is, by definition, non-flow-limiting, and coronary revascularisation in this setting may not be beneficial to the patient. This rationale suggests that measurement of flow may be an important factor in improving the accuracy of the FFR measures which are altered by microvascular disease8. However, only modest gains in flow-based technology have occurred over the past 15 years, largely attributable to the simplicity and relative robustness of coronary pressure measurements in clinical practice and patient outcome data demonstrating beneficial effects of coronary pressure-based revascularisation decision making. In order for true coronary flow-based clinical decision making to evolve, it is important to develop flow-based technologies further in order to: i) make these measurements applicable in daily clinical practice; and ii) regain interest from clinicians to apply them in their daily practice. Regarding the latter, studies such as those from Young-Woo Seo presented in this issue of the journal play an important role, since they remind us of the complexity of ischaemic heart disease and the great potential of multimodality physiological assessment to optimise diagnosis.
Conflict of interest statement
J. Davies is co-developer of IP which is licensed to Volcano Philips by Imperial College London. He receives consultancy and research funding from Philips Volcano. C. Cook is on the speaker’s bureau for Philips Volcano. J. Piek is a consultant for Philips Volcano and Abbott Vascular.