Abstract
Aims: We aimed to investigate the impact of concordance or discordance of fractional flow reserve (FFR) and coronary flow reserve (CFR) on coronary flow profiles and microvascular resistance after percutaneous coronary intervention (PCI), and the prognostic impact of the periprocedural physiological indices.
Methods and results: A total of 249 de novo physiologically significant coronary lesions from 231 patients who underwent FFR, CFR, and index of microcirculatory resistance (IMR) examinations before and after PCI were included. Baseline characteristics and physiological indices were compared between the concordant (FFR ≤0.80 and CFR <2.0, n=114) and discordant (FFR ≤0.80 and CFR ≥2.0, n=135) groups. Follow-up data were collected to determine predictors of cardiac events. Shortening of the mean transit time, CFR improvement, and decrease in the hyperaemic IMR were all significantly greater in the concordant territories. Cox proportional hazards analysis showed that a lower pre-PCI CFR was an independent predictor of adverse events at a median follow-up of 26.5 months, whereas neither the pre- nor post-PCI FFR was predictive of events. Event-free survival was significantly worse in patients with a lower pre-PCI CFR.
Conclusions: FFR/CFR concordantly abnormal territories provide a favourable benefit as assessed by coronary physiological indices after elective PCI. The pre-PCI CFR may predict adverse cardiac events.
Abbreviations
CABG: coronary artery bypass grafting
CFR: coronary flow reserve
FFR: fractional flow reserve
IMR: index of microcirculatory resistance
PCI: percutaneous coronary intervention
Tmn: mean transit time
Introduction
Coronary flow reserve (CFR) has been identified as a measure of coronary artery dysfunction that integrates the haemodynamic effects of epicardial coronary stenosis, diffuse atherosclerosis, and microvascular dysfunction on myocardial perfusion1,2 and carries an excellent prognostic value3,4. Current guidelines recommend a fractional flow reserve (FFR) cut-off value of 0.80 for revascularisation decision making5 irrespective of the CFR value. However, the clinical implications of the difference between FFR/CFR concordantly abnormal territories (FFR ≤0.80 and CFR <2.0) and FFR/CFR discordant territories (FFR ≤0.80 and CFR ≥2.0) for percutaneous coronary intervention (PCI) decision making remain unclear. Although the potential aim of PCI is to increase the coronary blood flow by targeting epicardial coronary stenosis, an increase in the hyperaemic coronary flow after PCI may not be determined solely by modifying the epicardial stenosis6. We hypothesised that epicardial stenosis with ischaemic FFR and preserved CFR may not exhibit favourable changes in the coronary flow profiles and that pre-PCI CFR may carry prognostic information. To test this hypothesis, we compared changes in physiological indices, including FFR, CFR, and the index of microcirculatory resistance (IMR), before and after successful PCI between territories with concordantly abnormal FFR/CFR and those with an ischaemic FFR and preserved CFR to elucidate the impact of PCI on coronary flow profiles. Furthermore, we assessed whether pre-PCI physiological indices predicted event-free survival after PCI.
Methods
STUDY POPULATION
The institutional database of cardiac catheterisation at Tsuchiura Kyodo General Hospital was searched for the period between January 2013 and September 2016 to identify patients treated with elective PCI who underwent FFR, CFR, mean transit time (Tmn), and IMR measurements before and after PCI. Patients were eligible for the analysis if they satisfied the following criteria: physiological assessment by pressure temperature sensor-tipped wire for a de novo single coronary lesion at the proximal or mid segment exhibiting intermediate to obstructive stenosis (estimated as 30-90% diameter stenosis on an angiogram by visual estimation). A total of 349 patients with 382 lesions were identified for the analysis. We excluded patients with left main disease, a history of coronary artery bypass grafting surgery (CABG), lesions requiring balloon angioplasty prior to pressure wire crossing, tandem lesions, and lesions with insufficient physiological data acquisition. Patients with a severely impaired systolic ejection fraction (<35%), culprit lesions of acute coronary syndrome, and lesions with FFR values >0.80 were also excluded. All patients received antiplatelet treatment with aspirin (200 mg/d) and clopidogrel (75 mg/d; loading dose, 300 mg) ≥24 hours before cardiac catheterisation. Of the 260 lesions from the 242 patients, 11 lesions fulfilled the definition of type 4a myocardial infarction7 in the present cohort and were excluded from the final analysis, since significant microvascular injury in these cases would result in impaired physiological profiles. Therefore, the final data set included 249 lesions from 231 patients. Baseline patient characteristics and follow-up data were collected by reviewing the medical charts and by telephone interviews. The study protocol was approved by the institutional review board, and all patients provided written informed consent for institutional database registration and future clinical research prior to catheterisation.
CARDIAC CATHETERISATION
Each patient initially underwent standard selective coronary angiography to assess the coronary anatomy via the radial artery using a 6 Fr system. Coronary angiograms were analysed quantitatively using the CMS-MEDIS system (Medis medical imaging systems, Leiden, the Netherlands) to measure the lesion length, minimum lumen diameter, reference lumen diameter, and percent diameter stenosis at the target lesion. All patients underwent coronary stent implantation (drug-eluting stent, 94%; bare metal stent, 6%; no bioresorbable vascular scaffolds) with predilatation. The type of stent was selected at the operator’s discretion. To avoid aggressive stent expansion, online quantitative coronary angiography was used to help determine the proper stent size. Successful PCI was defined as <20% residual stenosis with Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow. After the angiographic endpoint was achieved, intravascular ultrasound examination was performed to confirm optimal stent deployment, and additional PCI was performed in cases with suboptimal results.
INTRACORONARY PHYSIOLOGICAL INDICES
Before and after PCI, the FFR, mean Tmn, CFR, and IMR values were determined using the RadiAnalyzer™ Xpress instrument with the coronary PressureWire™ Certus™ (both St. Jude Medical, St. Paul, MN, USA) as described previously8-10. The post-PCI physiological assessment was performed approximately 10 minutes after completion of PCI. After administration of nitroglycerine, a pressure monitoring guidewire was advanced distal to a stenosis. Hyperaemia was induced by intravenous infusion of adenosine (140 μg/kg/min through a central vein). The FFR was calculated by dividing the mean distal pressure (Pd) by the mean aortic pressure (Pa) during stable hyperaemia. For the IMR measurements, hyperaemic thermodilution curves were obtained (three times each using a 3 ml saline bolus injection) and the mean hyperaemic Tmn were documented. IMR was calculated as the product of the mean Pd and the Tmn during stable hyperaemia10. CFR was calculated as the mean basal Tmn divided by the mean hyperaemic Tmn. In the presence of significant epicardial stenosis and/or collateral flow, accurate determination of the IMR has been reported to require measurement of the coronary wedge pressure11. In the present study, both corrected pre-PCI IMR values using wedge pressure during balloon predilatation and uncorrected pre-PCI IMR values were analysed. Since the inverse value of the mean hyperaemic Tmn has been validated to correlate with the absolute coronary blood flow6,9 and the Tmn can be used as a surrogate of the coronary flow velocity, a shorter Tmn suggests a higher coronary flow velocity with a greater hyperaemic coronary flow. A positive value calculated by subtracting the post-PCI Tmn from the pre-PCI Tmn might be interpreted as a shortening of the Tmn, suggesting improved coronary flow profiles after PCI and an increase in the hyperaemic coronary flow. Changes in the physiological indices were also studied and compared between territories with CFR <2.0 and CFR ≥2.0.
STATISTICAL ANALYSIS
Patient demographics are presented as n (%) where appropriate. Categorical data are expressed as absolute frequencies and percentages and were compared using the χ2 or Fisher’s exact test as appropriate. The data were analysed on a per-patient and per-lesion basis. Continuous variables are expressed as the mean±standard deviation for normally distributed variables or as the median (25th-75th percentiles) for non-normally distributed variables and were compared using the Student’s t-test or the Mann-Whitney U test, respectively. Receiver operating characteristic curves were analysed to assess the best cut-off values of the pre-PCI physiological indices for predictions based on the Cox proportional hazards regression analyses. The pre- and post-PCI physiological variables were analysed separately, and all significant variables were tested to identify predictors of adverse events during the follow-up period. Hazard ratios with corresponding 95% confidence intervals are reported. All variables associated with adverse events at the p<0.10 level in the univariate analysis were tested in a stepwise multivariable Cox regression analysis. Differences in combined adverse events according to the pre-PCI CFR value were analysed using the Kaplan-Meier method. Event-free survival curves were compared using the Mantel-Cox test. P<0.05 indicated statistical significance. The statistical analyses were performed using SPSS, Version 23.0 (IBM Corp., Armonk, NY, USA) and R version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
PATIENT CHARACTERISTICS, ANGIOGRAPHIC DATA, AND PHYSIOLOGICAL INDICES
The baseline patient characteristics are summarised in Table 1. A significant, albeit modest, relationship was found between the pre-PCI FFR and CFR (r=0.41; p<0.01) (Figure 1A). Figure 1B shows the distribution of the FFR values of the concordant and discordant groups. The concordant group comprised 114 territories (FFR 0.66 [0.57-0.74], CFR 1.36 [1.12-1.73]), and 135 territories were included in the discordant group (FFR 0.75 [0.69-0.78], CFR 3.00 [2.36-3.76]). The FFR and CFR were both significantly lower (p<0.01 for both comparisons) in the concordant group than those in the discordant group, and the IMR was significantly greater (p<0.01) in the concordant group. In the total cohort, both the FFR and CFR increased significantly after PCI (p<0.01), although the changes in the FFR and CFR were significantly greater in the concordant group than those in the discordant group (p<0.01 for both comparisons). The post-PCI CFR was significantly lower in the concordant group than that in the discordant group (p<0.01), whereas no significant differences in the post-PCI FFR and IMR were detected (p=0.11 and p=0.17, respectively). These results were consistent regardless of whether the IMR correction was applied or if the values were corrected only when the FFR values showed severe stenosis (FFR ≤0.65). Shortening of the Tmn was significantly greater in the concordant territories (p<0.01).
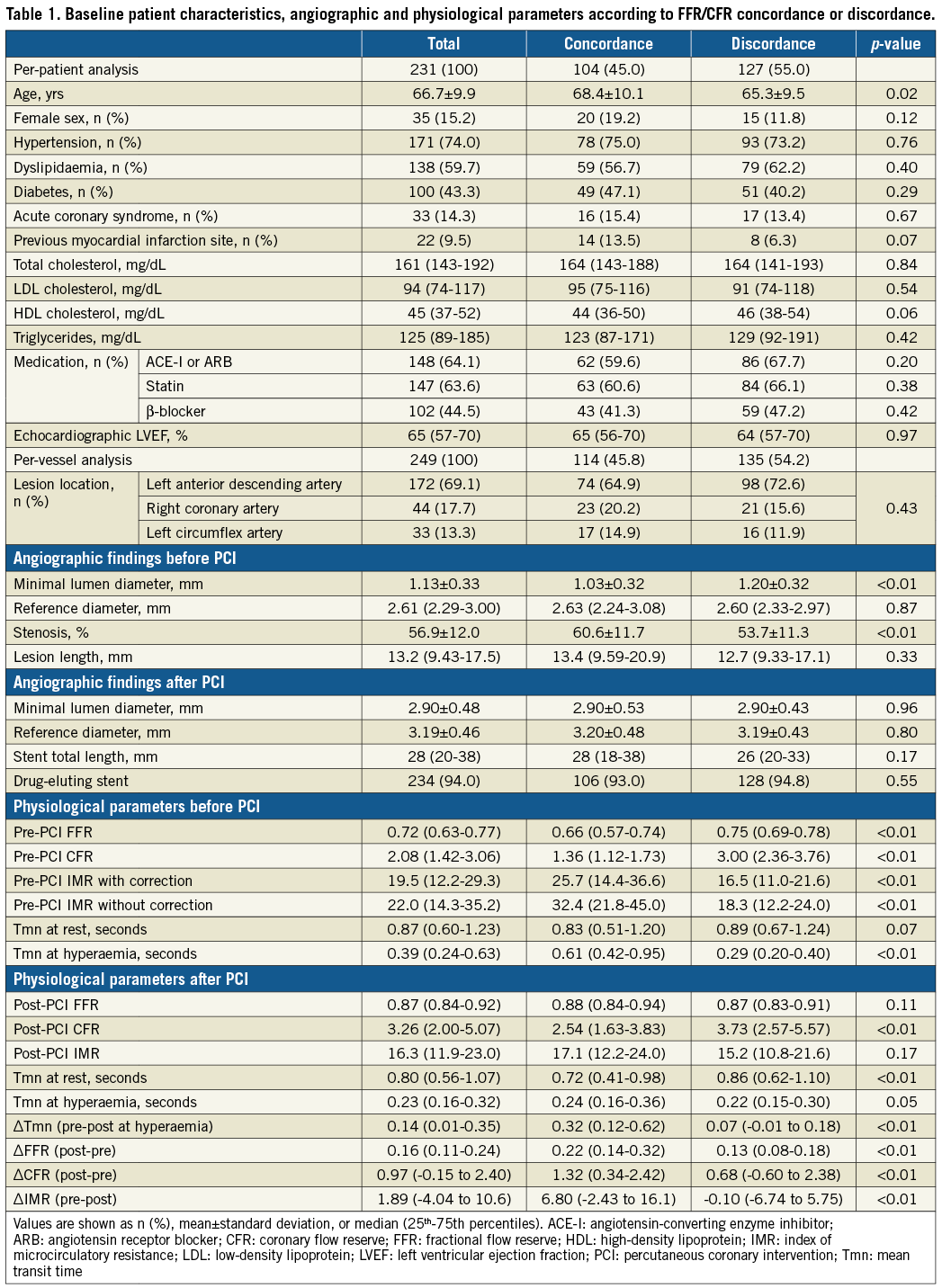
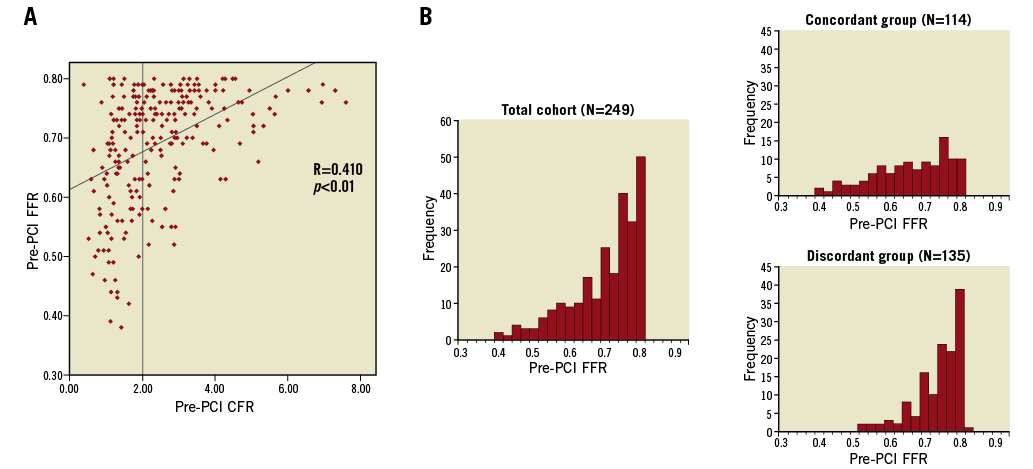
Figure 1. Distribution of lesions. A) Frequency distribution of lesions as a function of the FFR and CFR. A modest correlation was found between the FFR and CFR (r=0.41, p<0.01). B) Lesion-level histograms of the pre-PCI FFR in two groups divided by the CFR value of 2.0.
LONG-TERM FOLLOW-UP AFTER PCI
Four patients were lost at a median follow-up of 26.5 months (interquartile range 9.30-52.4 months). Therefore, the follow-up data were analysed for 245 (98.4%) lesions. The cumulative event rate of adverse events was 19.6% (48/245) (Table 2). No significant differences in coronary anatomy, angiographic findings, and elevation of cTnI after PCI were observed between the patients with and without adverse events. The pre-PCI CFR (p=0.06), post-PCI CFR (p=0.05), and post-PCI Tmn at baseline (p=0.04) tended to be different between lesions in patients with and without adverse events (Table 3). The stepwise multivariate Cox regression analysis showed that a low pre-PCI CFR (hazard ratio [HR] 0.764, 95% confidence interval [CI]: 0.592-0.986, p=0.039) was an independent predictor of adverse events during follow-up (Table 4). Receiver operating characteristic curve analysis showed that the optimal cut-off value of the pre-PCI CFR to predict adverse events was 2.26 (area under the curve 0.586; 95% CI: 0.494-0.679). Event-free survival was significantly worse in patients with a lower pre-PCI CFR (log-rank test χ2=9.011; p=0.003) (Figure 2).
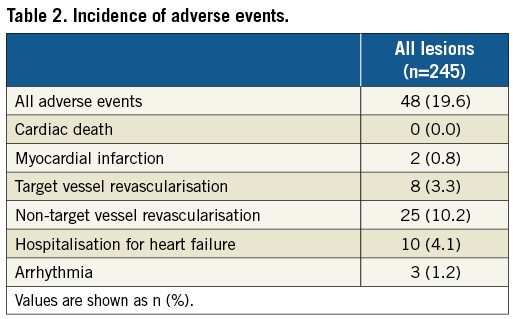
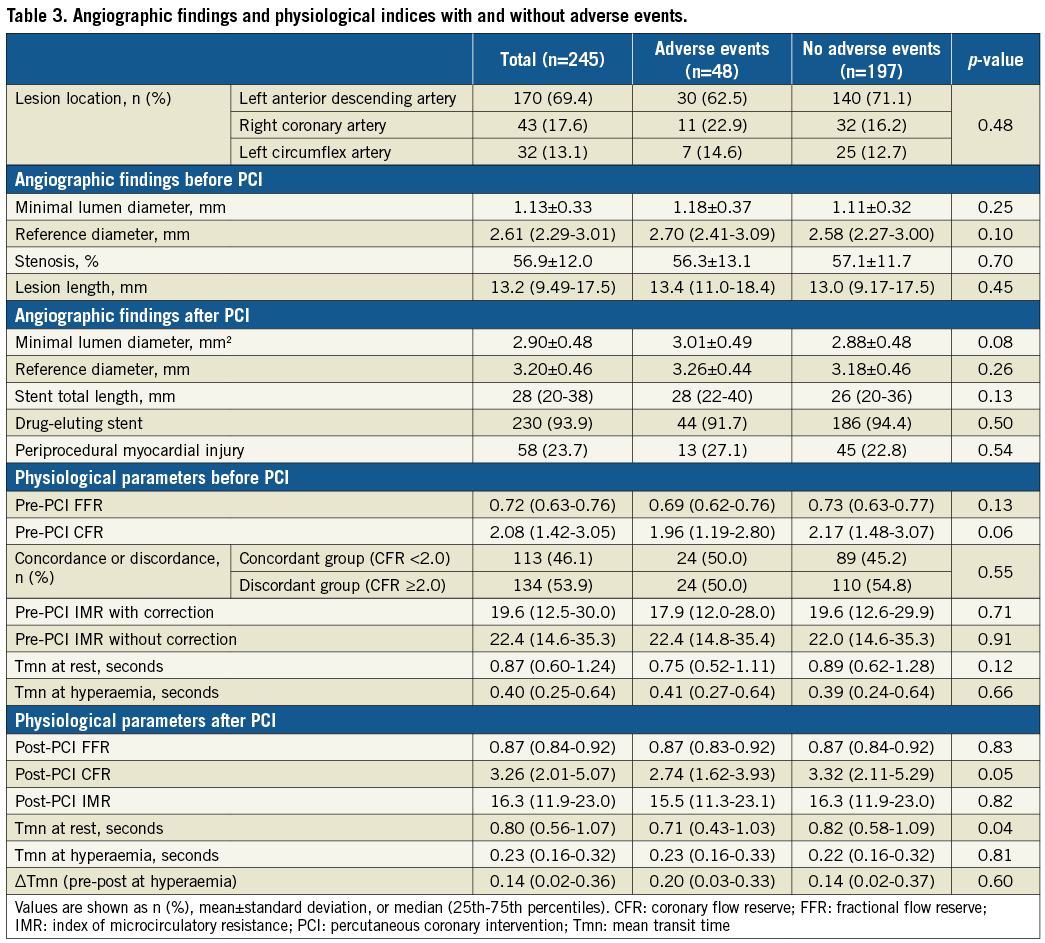
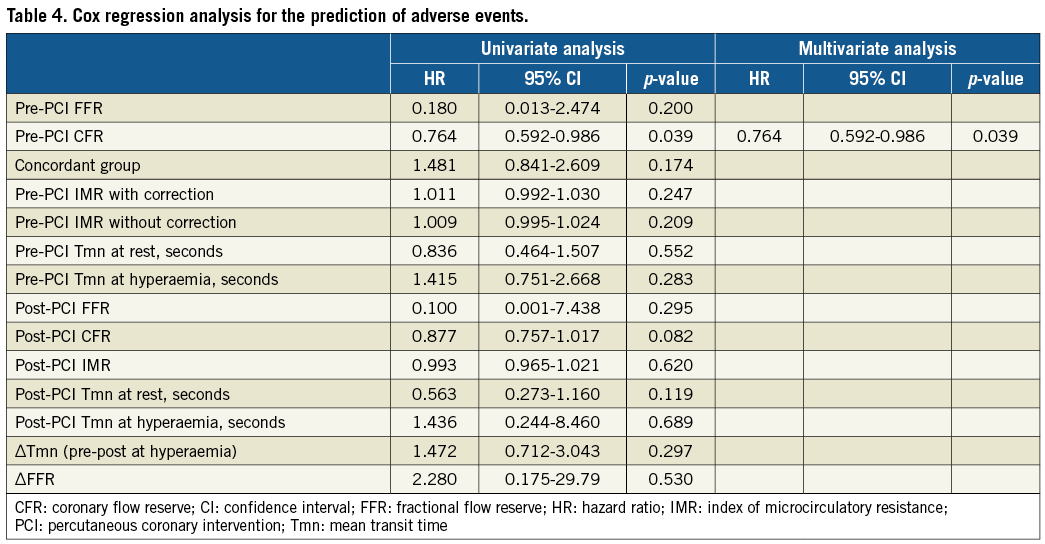
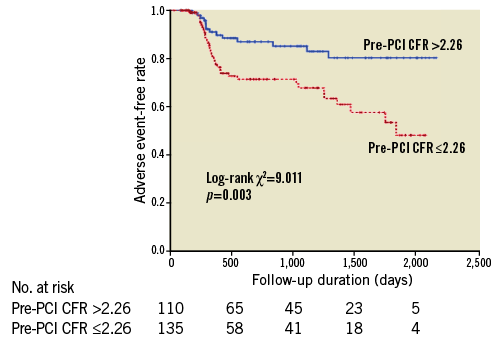
Figure 2. Kaplan-Meier curves according to the CFR cut-off values >2.26 and ≤2.26.
Discussion
The main findings of the present study are as follows. In patients undergoing elective PCI with lesions showing an ischaemic FFR, (1) territories with concordantly abnormal FFR/CFR showed significantly greater shortening of the mean transit time and improvement of the CFR when compared to the territories with a preserved CFR; (2) pre-PCI hyperaemic microvascular resistance was significantly higher in the group with concordantly abnormal FFR and CFR, although no significant difference in the IMR was observed between the two groups after PCI; and (3) a lower pre-PCI CFR was an independent predictor of adverse cardiac events during long-term follow-up after PCI.
DETERMINANTS OF CORONARY FLOW AFTER PCI
This study is the first to demonstrate that FFR/CFR concordance or discordance has an impact on coronary physiological indices after successful elective PCI. Pre-PCI CFR and FFR determinations may incrementally provide functional information. CFR provides important information that represents the effects of various circulatory status and is considered as a marker of the integrity of coronary artery function12,13. In territories with ischaemic FFR and preserved CFR, an FFR below the diagnostic cut-off value may reflect the potential to accommodate high hyperaemic coronary flow and not the presence of significantly flow-limiting stenosis14. Our results suggested that coronary flow improvement assessed by the surrogate marker of flow velocity after PCI for territories with ischaemic FFR and preserved CFR might be less than that in the territories with concordantly abnormal FFR and CFR. This concept might be supported by a study by van de Hoef et al which showed that the long-term outcomes of patients with non-flow-limiting stenosis were favourable after deferral of revascularisation3. FFR/CFR interrogation may clarify the existence of a differentiated pattern of ischaemic heart disease that harbours epicardial and microvascular dysfunction; this pattern may potentially benefit revascularisation decision making for individual lesion levels.
Our results also support those of a recent study suggesting that post-PCI changes in hyperaemic coronary blood flow velocity are associated with the baseline lesion physiological indices15. The lesions with a high pre-PCI IMR tended to decrease after PCI. This phenomenon was in line with the findings in our recent prospective study16, which showed that the magnitude and direction of change in the IMR immediately after PCI significantly correlated with the pre-PCI IMR and that decrease in the IMR was significantly associated with a favourable change in the coronary physiological index represented by Tmn shortening. The documentation of different outcomes by territories with different combinations or measures of these physiological indices has great importance and supports the feasibility of improving the invasive diagnosis of ischaemic coronary heart disease beyond FFR assessment.
EFFECTS OF CORONARY HAEMODYNAMIC INDICES ON THE CLINICAL OUTCOME
Although no significant relationship was found between FFR/CFR concordance/discordance and the occurrence of adverse cardiac events in the present study, the multivariate Cox regression analysis revealed that the pre-PCI CFR was an independent predictor of adverse cardiac events in the FFR-positive lesions. Our results indicated that no physiological indices after PCI or changes in these parameters were associated with event-free survival after PCI and that pre-PCI CFR, but not pre- or post-PCI FFR, may carry prognostic information.
In a recent prospective study, Barbato et al reported that the stenosis severity assessed by FFR was a major and independent predictor of lesion-related outcomes after treatment with medical therapy alone17. Conversely, numerous studies have demonstrated the capacity of CFR to predict future cardiovascular events in a wide range of the subset population3,4,18. These results were in line with our study, which indicated that CFR was a significant predictor of future adverse events, including culprit and non-culprit lesion-related events, heart failure, and other composite adverse events. Taqueti et al reported that the CFR was associated with adverse cardiac outcomes independent of revascularisation4. These authors also reported a significant interaction between the CFR and early revascularisation via CABG; as a result, patients with a low CFR who underwent CABG but not PCI experienced event rates comparable to patients with a preserved CFR independent of revascularisation. CFR may play an important role in diagnosing pathophysiological abnormalities that lead to adverse cardiac events in patients undergoing PCI. Although revascularisation should be considered for severely impaired FFR lesions because their lesion-related outcomes by medical therapy alone may not be favourable17, PCI may not alter the natural history of the total atherosclerotic disease burden of these patients. Compared with FFR, which represents the epicardial focal stenosis severity, CFR includes focal epicardial stenosis, diffuse arterial disease, and microvascular dysfunction, suggesting that CFR may be a better surrogate marker of integrated vascular function. Coronary arterial dysfunction may exist diffusely in addition to local isolated stenosis and microvascular dysfunction, and thus localised mechanical intervention may fail to alter long-term disease outcomes. In the present study, more than half of the events were non-target vessel revascularisation, and lower pre-PCI CFR values were significantly associated with these adverse events. Our results may indicate an association between a lower regional CFR and impaired global cardiovascular function. Our results also strongly support the concept of an ongoing clinical trial (DEFINE-FLOW; NCT02328820). A prospective large clinical study is needed to investigate the efficacy of increases in the CFR relative to the FFR.
Study limitations
This study has several limitations that warrant consideration in the interpretation of the results. First, this study included subjects from a single centre and was retrospective; consequently, selection bias was unavoidable. Second, the decision to perform the FFR measurement was at the discretion of the operator. Third, we measured a validated surrogate of absolute coronary flow (Tmn). Fourth, because the injection of saline can cause submaximal hyperaemia to some extent, thermodilution method-derived CFR values may be different from conventional velocity-derived CFR values. Fifth, there is no solid scientific basis for defining a biomarker threshold to diagnose periprocedural myocardial injury. Sixth, because analysis of non-culprit vessels was not performed, the results might have been biased by a focal, single vessel assessment of flow. Finally, because the extent of post-PCI improvement of coronary physiological indices capable of improving symptoms or producing a prognostic benefit is unknown, the clinical significance and findings of the present study should be considered hypothesis-generating and should be tested in future large, prospective studies.
Conclusions
FFR/CFR concordance or discordance influenced coronary physiological indices after elective PCI for lesions showing an ischaemic FFR. Compared with territories showing an ischaemic FFR and preserved CFR, FFR/CFR concordantly abnormal territories showed a favourable impact on Tmn shortening and CFR improvement after elective PCI. Impairment of the pre-PCI CFR may predict adverse cardiac events after a successful PCI.
| Impact on daily practice Current guidelines recommend an FFR cut-off value of 0.80 for revascularisation decision making in the absence of prior objective evidence of myocardial ischaemia in patients with angina, irrespective of the CFR value. In patients undergoing an elective PCI, territories in the FFR/CFR concordantly abnormal group showed significantly favourable changes in the coronary physiological indices after PCI when compared with those exhibiting an ischaemic FFR and preserved CFR; during long-term follow-up after PCI, event-free survival was significantly worse in the patients with a lower pre-PCI CFR. The documentation of different outcomes by territories with different combinations of physiological indices supports the feasibility of improving the functional diagnosis of ischaemic coronary heart disease beyond FFR assessment. |
Conflict of interest statement
The authors have no conflicts of interest to declare.