Abstract
Aims: Adenosine administration is needed for the achievement of maximal hyperaemia fractional flow reserve (FFR) assessment. The objective was to test the accuracy of Pd/Pa ratio registered during submaximal hyperaemia induced by non-ionic contrast medium (contrast FFR [cFFR]) in predicting FFR and comparing it to the performance of resting Pd/Pa in a collaborative registry of 926 patients enrolled in 10 hospitals from four European countries (Italy, Spain, France and Portugal).
Methods and results: Resting Pd/Pa, cFFR and FFR were measured in 1,026 coronary stenoses functionally evaluated using commercially available pressure wires. cFFR was obtained after intracoronary injection of contrast medium, while FFR was measured after administration of adenosine. Resting Pd/Pa and cFFR were significantly higher than FFR (0.93±0.05 vs. 0.87±0.08 vs. 0.84±0.08, p<0.001). A strong correlation and a close agreement at Bland-Altman analysis between cFFR and FFR were observed (r=0.90, p<0.001 and 95% CI of disagreement: from –0.042 to 0.11). ROC curve analysis showed an excellent accuracy (89%) of the cFFR cut-off of ≤0.85 in predicting an FFR value ≤0.80 (AUC 0.95 [95% CI: 0.94-0.96]), significantly better than that observed using resting Pd/Pa (AUC: 0.90, 95% CI: 0.88-0.91; p<0.001). A cFFR/FFR hybrid approach showed a significantly lower number of lesions requiring adenosine than a resting Pd/Pa/FFR hybrid approach (22% vs. 44%, p<0.0001).
Conclusions: cFFR is accurate in predicting the functional significance of coronary stenosis. This could allow limiting the use of adenosine to obtain FFR to a minority of stenoses with considerable savings of time and costs.
Introduction
Fractional flow reserve (FFR) is the ratio of two flows that can be calculated from the ratio of two pressures, provided they are both measured during maximal hyperaemia1. Consequently, the achievement of hyperaemia is the crucial prerequisite to assess FFR correctly. For this purpose, intravenous (i.v.) administration of adenosine is still considered the gold standard2. However, for cost, time and practical reasons, the intracoronary (i.c.) route is frequently preferred3. On the other hand, i.c. adenosine also has some potential drawbacks, including significant bradyarrhythmias which may require the interruption of FFR assessment4,5. Considering that administration of other vasodilator agents2,6 is further limited by their side effects, it is not surprising that adenosine-free pressure-derived indices, such as the instantaneous wave-free ratio (iFR), have been proposed, with, however, conflicting results7,8.
Previous studies have shown that radiographic contrast medium, routinely used during coronary angiography, and also during FFR assessment to check the correct positioning of the pressure wire, leads to coronary hyperaemia9,10, but to a lesser extent than with adenosine6. Thus, we hypothesised that the Pd/Pa ratio measured using an intracoronary pressure-sensitive guidewire following injection of radiographic contrast medium is diagnostically useful and would commonly rule out the need for adenosine. In fact, we recently demonstrated that contrast medium-induced Pd/Pa, also known as contrast FFR (cFFR), is very accurate in predicting FFR, and could represent a valid surrogate for FFR, potentially limiting the use of adenosine to doubtful cases11,12. These studies represented the background for the CONTRAST study, a large multicentre study comparing the ability of cFFR to predict FFR versus resting indices. CONTRAST showed that cFFR is superior to resting Pd/Pa and iFR for predicting FFR, while resting Pd/Pa and iFR provided equivalent diagnostic accuracy13.
We designed the Multi-center Evaluation of the Accuracy of the Contrast MEdium INduced Pd/Pa RaTiO in Predicting FFR (MEMENTO-FFR) Study in order to elucidate further the accuracy of cFFR in predicting FFR in a large real-world series of lesions requiring functional assessment for clinical purposes.
Methods
The Multi-center Evaluation of the Accuracy of the Contrast MEdium INduced Pd/Pa RaTiO in Predicting FFR (MEMENTO-FFR) was an international, multicentre, non-randomised, collaborative, retrospective pooled analysis of the accuracy of cFFR in predicting FFR in patients with coronary artery disease in whom physiological lesion assessment was clinically indicated. Data were obtained from different local registries in 10 centres of four European nations, comprising 380 lesions in Italy (Rome), 177 in Portugal (Amadora and Carnaxide), 141 in France (Paris) and 328 in Spain (Madrid, Barcelona, Santander, Valladolid, San Sebastian, Alicante). Some of these data have been included in previous publications11,12 (Online Appendix).
From December 2011 to July 2015, 962 patients with 1,026 coronary artery stenoses were enrolled.
The identification of the stenosis which required functional assessment was left to the operator’s discretion. Clinical exclusion criteria were recent myocardial infarction, severe valvular heart disease, acute heart failure, or advanced renal failure such that an additional dose of up to 20 mL of contrast would pose, in the opinion of the operator, unwarranted risk. The study was approved by the local ethics committees and conformed to the Declaration of Helsinki. Informed consent was obtained after explanation of the protocol and potential risks. Diagnostic coronary angiography was performed using the radial or femoral approach. The choice of non-ionic radiographic contrast medium and modality of intracoronary injection were left to local practice (Online Appendix).
PRESSURE MEASUREMENTS
A 0.014-inch pressure monitoring guidewire (Certus™ or Aeris™ PressureWire™; St. Jude Medical, St. Paul, MN, USA; PrimeWire™ or Verrata® wires; Volcano Corporation, Rancho Cordova, CA, USA) was calibrated and introduced into the guiding catheter. The pressure transducer was advanced just outside the tip of the guiding catheter, and the pressure measured by the sensor was then equalised to that of the guiding catheter. The femoral or brachial vein was used for systemic administration of adenosine. An FFR value of ≤0.80 was considered the significant ischaemic threshold.
STUDY PROTOCOL
The study consisted of three sequential steps separated by at least 30 seconds until the return of Pd/Pa ratio to baseline value:
1.Resting Pd/Pa assessment: an initial period of at least one minute provided a stable assessment of resting physiology for calculation of resting Pd/Pa.
2.cFFR assessment: a single injection of radiographic contrast medium was performed according to standard local practice (Online Appendix). cFFR was calculated as the lowest ratio of distal coronary pressure divided by aortic pressure obtained after injection of radiographic contrast medium, in the first 10 seconds after injection. Reproducibility of cFFR was tested in a subgroup of lesions repeating the injection of contrast medium 30 seconds after the first one (Online Appendix). After acquisition of the valid cFFR value, a flushing of the guiding catheter with saline was performed in order to avoid pressure damping due to contrast medium viscosity, to restore resting conditions and then to assess FFR correctly.
3.FFR assessment: maximal hyperaemia was induced by i.c. or i.v. adenosine administration, according to local practice (Online Appendix). The valid FFR value was considered the lowest Pd/Pa value during stable hyperaemia when i.v. adenosine was used and the lowest Pd/Pa value in the first 10 seconds after injection in case of i.c. adenosine.
Patient symptoms, development of complete AVB or any other complication, were carefully recorded. The clinical data of enrolled patients were collected in dedicated electronic databases at the time of the interventional procedure and merged in a single central database when the MEMENTO-FFR study was conceived by the authors.
STATISTICAL ANALYSIS
Categorical variables were expressed as percentages and analysed by Fisher’s exact test. Continuous variables were expressed as mean±SD and/or median (interquartile range) and compared using the paired t-test or the non-parametric Wilcoxon test, as appropriate. The relationship between cFFR and FFR was quantified with a coefficient of determination. The accuracy of cFFR in predicting FFR was assessed by measuring the area under the curve (AUC) by receiver operating characteristic (ROC) curve analysis. Correlation and agreement by Bland-Altman analysis with FFR, calculation of the optimal cut-off at Youden index in predicting an FFR ≤0.80 and its accuracy using a McNemar test between metrics, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) were obtained. All these measures were obtained for resting Pd/Pa too. Comparison of ROC curves for resting Pd/Pa and cFFR was performed using the DeLong method. Reproducibility of cFFR was tested by coefficient of determination in a lesion subset (Online Appendix).
Finally, as in previous reports11,13,14, we maximised the diagnostic accuracy by identifying two cut-offs for both resting Pd/Pa and cFFR below and above which use of adenosine could be avoided with at least 95% safety, limiting adenosine for FFR assessment to intermediate values (the so-called “hybrid approach”). We decided to identify the lower cut-off as the lowest value of cFFR or resting Pd/Pa with a 95% specificity for an FFR ≤0.80, while the upper cut-off was identified as the lowest value with a 95% sensitivity for an FFR ≤0.80. Accuracy, PPV, NPV and number of lesions requiring adenosine for both resting Pd/Pa/FFR and cFFR/FFR hybrid approaches were calculated and compared using a chi-square test with Yates’ correction.
Results
PATIENT CHARACTERISTICS AND SAFETY OF THE PROCEDURE
Patient characteristics are summarised in Table 1. The majority of patients had stable coronary artery disease with intermediate coronary stenosis. FFR was evaluated inducing hyperaemia using i.v. adenosine in most of the cases, while cFFR was obtained using iomeprol and an automatic injection in the majority of patients (Table 1, Online Appendix).
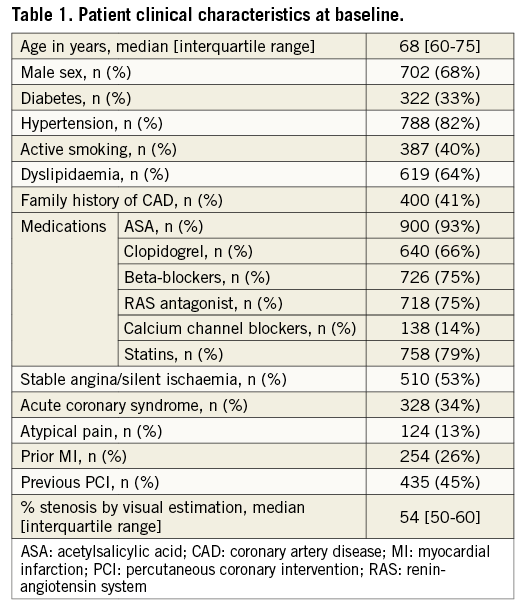
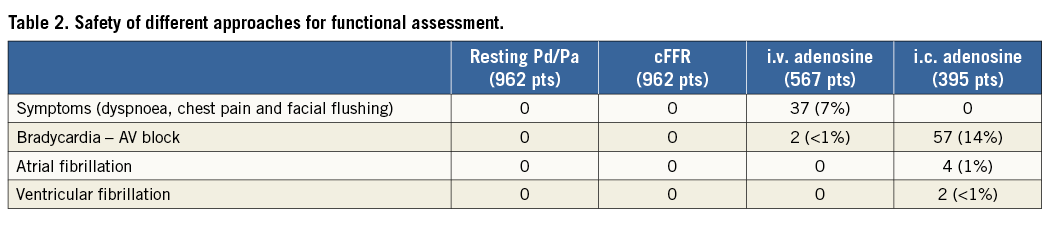
As expected, resting Pd/Pa and cFFR were not associated with any symptom, while administration of i.c. adenosine for assessing FFR was associated with 57 cases of bradycardia or complete AVB not requiring atropine or pacing, four cases of atrial fibrillation (two cases spontaneously resolved in less than five minutes, one case needed electrical cardioversion and one case resolved by i.v. amiodarone), and two cases of ventricular fibrillation needing DC shock. On the other hand, while administration of i.v. adenosine was associated with 37 cases of unpleasant symptoms (dyspnoea, chest pain and facial flushing), there were only two cases of significant bradycardia (Table 2).
cFFR VS. FFR
FFR values were significantly lower than Pd/Pa and cFFR values (Figure 1). Both resting Pd/Pa and cFFR were significantly correlated to FFR (r=0.79, r²=0.62; p<0.001 and r=0.90, r²=0.81; p<0.001, respectively) (Figure 2A, Figure 2B). However, cFFR showed a higher r-coefficient and a lower spread of data with a very strong agreement with FFR by Bland-Altman analysis (Figure 2C, Figure 2D).
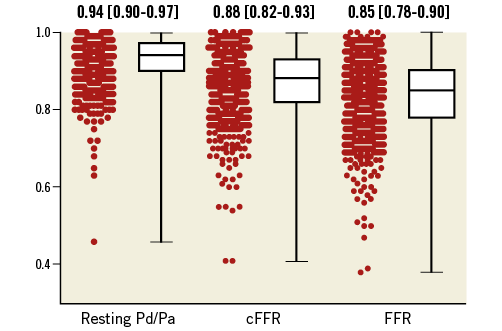
Figure 1. Median values (interquartile ranges) of resting Pd/Pa, contrast fractional flow reserve (cFFR) and fractional flow reserve (FFR).
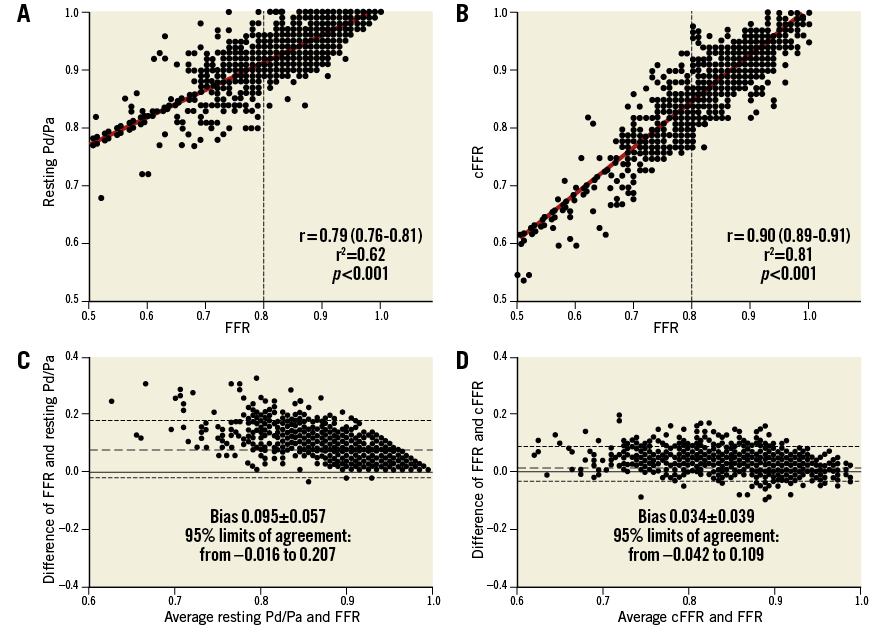
Figure 2. FFR comparisons. A) & B) Correlation between resting Pd/Pa or contrast fractional flow reserve (cFFR) and fractional flow reserve (FFR) values. C) & D) Bland-Altman plots for the agreement between resting Pd/Pa or contrast fractional flow reserve (cFFR) and fractional flow reserve (FFR).
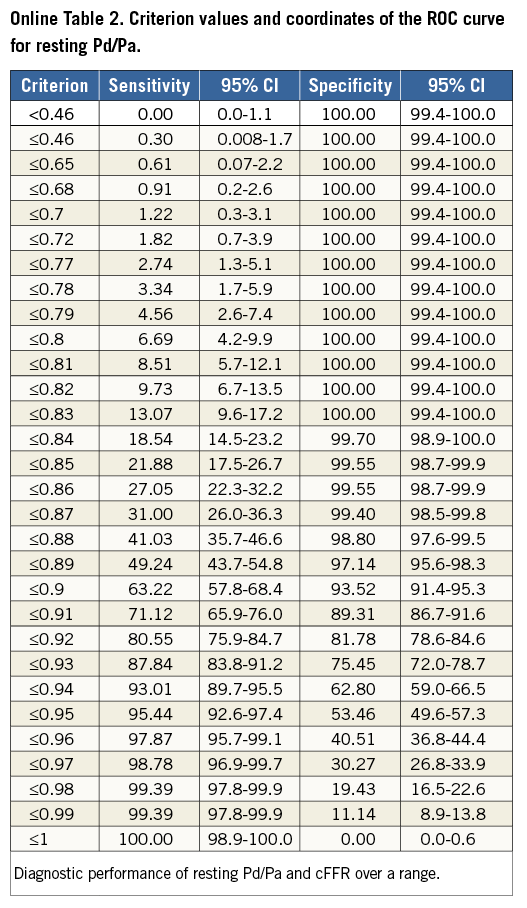
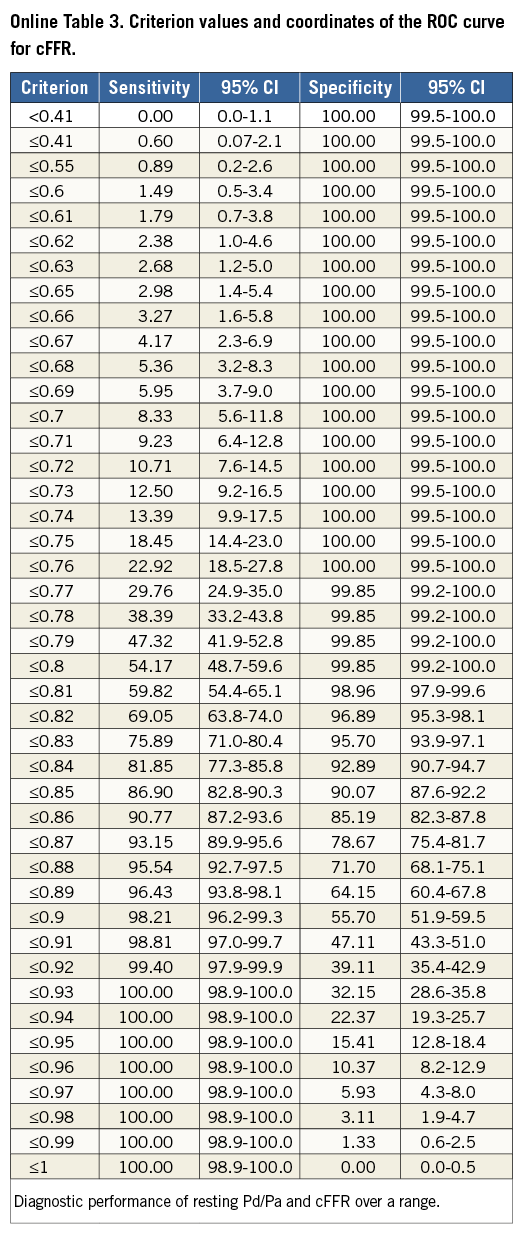
Using ROC curve analysis, cFFR strongly predicts FFR with an AUC of 0.95 (95% CI: 0.94-0.96), significantly better than resting Pd/Pa, AUC 0.90 (95% CI: 0.88-0.91) (p<0.001). Moreover, for cFFR, the single cut-off of ≤0.85 had the best combination of sensitivity (87%) and specificity (90%) by the Youden index with a PPV of 82% and an NPV of 93%. More importantly, with this cut-off cFFR had an accuracy of 89% in identifying a correct FFR. The best cut-off for resting Pd/Pa was ≤0.93, which showed a similar sensitivity (87%) and an NPV (92%) but a lower specificity (76%) and PPV (65%) and, more importantly, a significantly lower accuracy (80%, p<0.0001) in identifying a correct FFR as compared to cFFR ≤0.85 (Figure 3).
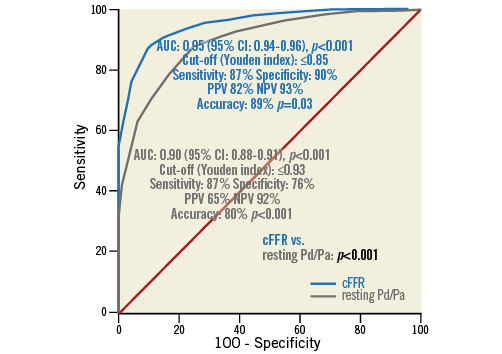
Figure 3. Receiver operating characteristic curve calculated using the threshold cut-off for fractional flow reserve (FFR) of ≤0.80. Contrast fractional flow reserve (cFFR) strongly predicts FFR (area under the curve [AUC] 0.95), significantly better than resting Pd/Pa (AUC 0.90). A cut-off of 0.85 of cFFR, obtained using the Youden index, had the best combination of sensitivity (87%) and specificity (90%) and an 89% accuracy in predicting a positive FFR, significantly better than resting Pd/Pa at the cut-off of 0.93.
While FFR was ≤0.80 in 349 cases (34%), resting Pd/Pa and cFFR were ≤0.80 in 25 (2.4%) and 192 cases (19%), respectively.
Regarding the hybrid approach, both a resting Pd/Pa/FFR and a cFFR/FFR hybrid approach showed an equivalent excellent accuracy (96%) (Figure 4A, Figure 4B). However, a cFFR/FFR hybrid approach resulted in a significantly lower number of lesions requiring adenosine (22% vs. 44%, p<0.0001).
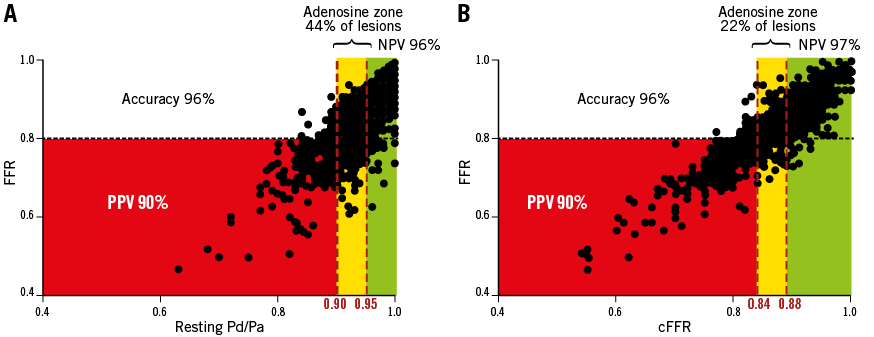
Figure 4. Hybrid revascularisation strategy with resting Pd/Pa or cFFR and fractional flow reserve. Both a resting Pd/Pa/FFR (A) and a cFFR/FFR (B) hybrid approach showed an equivalent excellent accuracy (96%). However, a cFFR/FFR-based hybrid approach showed a significantly lower number of lesions requiring adenosine (22% vs. 44%, p<0.0001).
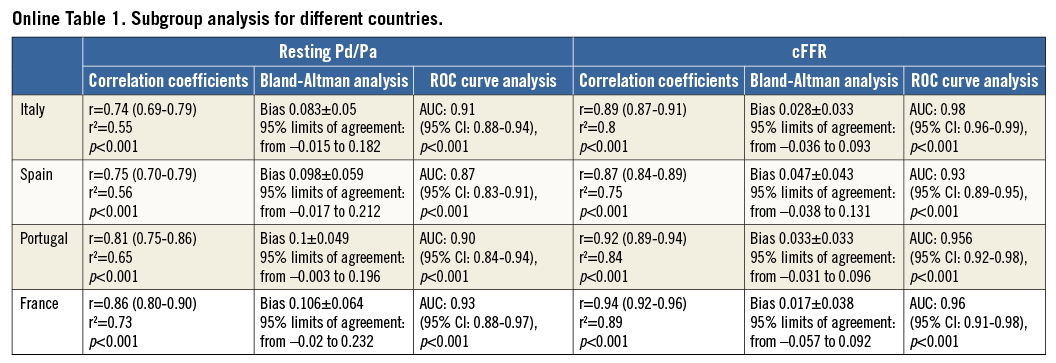
Subgroup analysis showed lack of difference for the type or the amount of contrast medium used, for its modality of administration and for the country of origin (Online Appendix, Online Figure 1, Online Table 1, Online Table 2, Online Table 3).
Discussion
The results of the MEMENTO-FFR study confirm that cFFR, calculated as Pd/Pa after the induction of submaximal hyperaemia using an i.c. injection of standard radiographic contrast medium, accurately predicts FFR, significantly better than resting Pd/Pa. This could allow limiting the use of adenosine to obtain FFR to a minority of doubtful cases.
The crucial prerequisite to assess FFR correctly is the achievement of maximal hyperaemia and for this purpose, given its favourable risk/efficacy profile, i.v. adenosine is still the gold standard1,15 and i.c. administration a valuable alternative11. This was also confirmed in our study in which the occurrence of symptoms and of significant side effects was relatively low, despite being potentially disturbing. Nevertheless, FFR is still underused in clinical practice and some authors have suggested further simplifying functional assessment by using resting gradient-derived measures7,16,17. In particular, Sen et al proposed the instantaneous wave-free ratio (iFR) as a novel adenosine-free index of stenosis severity7. The notion of iFR is based on the hypothesis that there is a diastolic “wave-free” period when microvascular resistance is already constant and minimal and consequently does not need a further vasodilation. However, this hypothesis was challenged by Berry et al who showed in the VERIFY study that assessment of iFR during infusion of adenosine gave significantly lower values than iFR in resting conditions and a much higher accuracy in predicting FFR18. Moreover, the VERIFY, RESOLVE and CONTRAST studies showed that iFR is not significantly more accurate in predicting FFR than resting Pd/Pa7,8,18. Overall, these studies consistently showed that non-hyperaemic indices have an accuracy of around 80% in predicting FFR. This was also confirmed in our study in which resting Pd/Pa exhibited an 80% accuracy. This implies that, if we take FFR as the gold standard, which is obtained (by definition) during maximal hyperaemia, we must induce a certain degree of hyperaemia to reach an acceptable level of accuracy. However, the burning questions are how to induce a sufficient hyperaemia and what is the amount of hyperaemia that we can give up without losing accuracy significantly.
Much of our knowledge in coronary physiology stems from the original studies of K. Lance Gould. It is worth noting that he used contrast medium to induce hyperaemia and describe the pressure/flow/resistance relations in the presence of coronary stenosis9. In the following years, the development of FFR gave interventional cardiologists a realistic and practical tool to assess the functional significance of coronary artery stenosis in clinical scenarios19. In the early days of the history of FFR, contrast medium was again proven to induce reactive hyperaemia, probably related to its osmolality10, although significantly less than adenosine6. For this reason, contrast medium was abandoned and eliminated from the list of recommended vasodilators1. Nevertheless, in clinical practice it is likely that submaximal hyperaemia induced by contrast medium could be sufficient to evaluate the vast majority of stenoses without losing accuracy significantly. This working hypothesis was tested in the RINASCI study11. Indeed, we demonstrated that Pd/Pa registered after the injection of a standard dose of contrast medium was very accurate in predicting FFR and that the use of this approach could reduce the use of adenosine to one case in five. In the beginning, we preferred to avoid the use of the term FFR, which needs by definition maximal hyperaemia, and we called this index contrast medium-induced Pd/Pa ratio (CMR); nevertheless, in the following studies the more direct term cFFR was preferred. Indeed, the results of the RINASCI study were confirmed by Baptista, Martin-Reyes (abstract P4537 and P6374 at ESC Congress 2014) and Spagnoli et al12-14 and collectively represented the background for the CONTRAST study15. CONTRAST was a large multicentre study comparing ability in predicting FFR by cFFR vs. resting indices (resting Pd/Pa, iFR). The results documented that cFFR was superior to resting Pd/Pa and iFR in predicting FFR while iFR and resting Pd/Pa provided equivalent diagnostic accuracy. With the MEMENTO-FFR study, we intended to corroborate these data independently in the largest real-world population of patients to date, even larger than the CONTRAST study. Notably, our results clearly confirm that cFFR is a reliable surrogate for FFR that can simplify functional assessment of coronary stenosis in clinical practice. We observed an accuracy of 89% for the single cut-off of cFFR ≤0.85, very similar to that observed in the CONTRAST study. In practice, this means that, without the use of adenosine, the operator has in cFFR a simple and always available tool to evaluate the functional significance of coronary stenosis that is accurate in nine cases out of ten, much better than that which we can obtain using resting Pd/Pa (and probably iFR)13. Nevertheless, when the operator does not intend to renounce the highest possible accuracy, but at the same time he wants to minimise the use of adenosine, a cFFR/FFR hybrid approach exhibits an accuracy of >95% while the need for FFR is limited to about one case in five. This is half the number of lesions that would have needed FFR using a hybrid approach based on iFR or Pd/Pa8,13. In simple terms, this means that cFFR should be the preferred approach in clinical practice, and the use of resting indices cannot be justified since diagnostic accuracy is lower and adenosine would be used more often.
We think that cFFR could help in promoting a physiology-based approach to the treatment of intermediate coronary artery stenosis. Indeed, cFFR, despite the impossibility of performing a pullback evaluation for the shortness of the contrast medium-induced hyperaemia, could allow a rapid assessment of all major coronary branches, especially in multivessel disease, limiting standard FFR with adenosine infusion to a minority of doubtful lesions (according to the proposed algorithm in Figure 5). Moreover, cFFR-guided PCI could be easier in comparison to FFR-guided PCI, not requiring additional adenosine and using the same amount of contrast medium needed to visualise the coronary tree during PCI. This could allow replicating the favourable results of the FAME 1 study using a quicker solution, similar to the evaluation using resting iFR in the ongoing SYNTAX II study20,21. On the other hand, we should be aware that, while FFR has a well-known prognostic effect22, similar data about cFFR are still lacking. Consequently, although this information is going to be collected, in the meantime operators have to be cautious in drawing conclusions about the midterm and long-term prognosis associated with cFFR values.
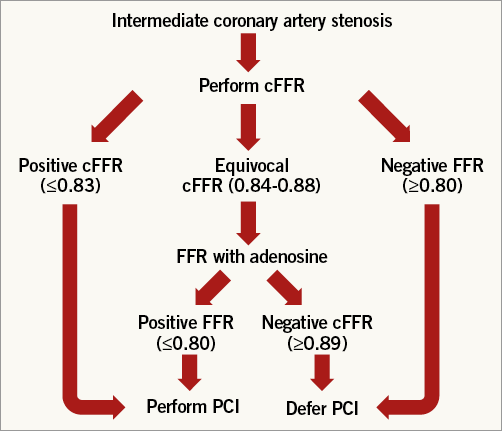
Figure 5. A simple algorithm to limit adenosine administration only to doubtful cases. We consider a cFFR value ≤0.83 significant (consequently we suggest performing PCI), a cFFR value ≥0.89 not significant (consequently we suggest deferring PCI) and inducing maximal hyperaemia using adenosine for FFR assessment when cFFR is between 0.84 and 0.88. After that, PCI would be performed when FFR is ≤0.80 and deferred when FFR is >0.80.
We acknowledge that MEMENTO-FFR has some limitations. First, this is a collaborative pooled analysis and consequently different local protocols were used in assessing FFR and, more importantly, cFFR. However, considering the lack of impact of different contrast media and the modality of administration, this potential weakness further strengthens the wide applicability of cFFR to clinical practice. Second, we did not record raw data and pressure tracings in a dedicated database. This is due to the real-world nature of our study and made it impossible to calculate offline iFR in order to compare cFFR to iFR on a large sample. However, taking into account that the RESOLVE and CONTRAST studies8,13 showed that iFR is not significantly more accurate than resting Pd/Pa in predicting FFR, we can reasonably infer that the inclusion of iFR assessment would not have changed the results of the MEMENTO-FFR study significantly.
| Impact on daily practice cFFR is remarkably accurate in predicting the functional significance of coronary stenosis with FFR as the gold standard. cFFR is also superior to resting Pd/Pa both using a single cut-off and using a hybrid approach. The use of cFFR may allow limiting the use of adenosine only to doubtful cases with meaningful savings in time and costs. |
Conflict of interest statement
A.M. Leone has received speaking honoraria from St. Jude Medical. S. Baptista has received investigation grants from St. Jude Medical. N. Amabile has received consulting honoraria from St. Jude Medical. L. Raposo has received investigation grants from St. Jude Medical and speaker fees from St. Jude Medical and Volcano Corp. The other authors have no conflicts of interest to declare.
SUPPLEMENTARY DATA
Online Appendix. Details of local practices
Centre by centre local practice for contrast medium injection, induction of hyperaemia and basal Pd/Pa, cFFR and FFR assessment.
– Rome (Italy):
- Modality of injection of contrast medium: automatic injection (Medrad® Avanta™; Bayer HealthCare, Warrendale, PA, USA).
- Type and amount of contrast medium: 6 ml of iomeprol (Iomeron®; Bracco SpA, Milan, Italy).
- Pressure wires: Certus™ or Aeris™ PressureWire; St. Jude Medical, St. Paul, MN, USA; PrimeWire™ or Verrata® wires; Volcano Corporation, Rancho Cordova, CA, USA.
- Drug for hyperaemia: adenosine i.v. (140 mcg/kg/min) 69%, i.c. (600 mcg) 31%.
– Madrid, Barcelona, Santander, Valladolid, San Sebastian, Alicante (Spain):
- Modality of injection of contrast medium: automatic injection (ACIST CVi®; ACIST Europe B.V., Maastricht, The Netherlands).
- Type and amount of contrast medium: 8 ml for left coronary artery and 5 ml for right coronary artery of iomeprol (Iomeron®; Bracco SpA, Milan, Italy).
- Pressure wires: Aeris™ PressureWire; St. Jude Medical, St. Paul, MN, USA.
- Drug for hyperaemia: adenosine i.v. (140 mcg/kg/min) 63%, i.c. (360 mcg for left coronary artery, 90 mcg for right coronary artery) 37%.
– Amadora (Portugal):
- Modality of injection of contrast medium: manual injection.
- Type and amount of contrast medium: 10 ml for left coronary artery and 5 ml for right coronary artery of iopromide (Ultravist®; Bayer, Leverkusen, Germany) (75%), iodixanol (Visipaque®; GE Healthcare, Chalfont St. Giles, United Kingdom) (25%).
- Pressure wires: Certus™ or Aeris™ PressureWire; St. Jude Medical, St. Paul, MN, USA.
- Drug for hyperaemia: adenosine i.v. (140 mcg/kg/min).
– Lisbon-Carnaxide (Portugal):
- Modality of injection of contrast medium: manual injection 60%, automatic injection (ACIST CVi; ACIST Europe B.V., Maastricht, The Netherlands) 40%.
- Type and amount of contrast medium: 10 ml for left coronary artery and 6 ml for right coronary artery of iomeprol (Iomeron®; Bracco SpA, Milan, Italy) (60%) and iodixanol (Visipaque®; GE Healthcare, Chalfont St. Giles, United Kingdom) (40%).
- Pressure wires: Certus™ or Aeris™ PressureWire; St. Jude Medical, St. Paul, MN, USA; PrimeWire™ or Verrata® wires; Volcano Corporation, Rancho Cordova, CA, USA.
- Drug for hyperaemia: adenosine i.v. (140 mcg/kg/min).
– Paris (France):
- Modality of injection of contrast medium: manual injection.
- Type and amount of contrast medium: 10 ml for left coronary artery and 5 ml for right coronary artery of iopromide (Ultravist®; Bayer, Leverkusen, Germany) (75%) and iodixanol (Visipaque®; GE Healthcare, Chalfont St. Giles, United Kingdom) (25%).
- Pressure wires: Aeris™ PressureWire; St. Jude Medical, St. Paul, MN, USA.
- Drug for hyperaemia: adenosine i.v. (140 mcg/kg/min).
Reproducibility of cFFR in 103 lesions (10% of the entire lesion population) showed a very good agreement (r=0.99, p<0.0001) and agreement by Bland-Altman analysis (bias –0.001±0.01, 95% limits of agreement from –0.02 to 0.02).
FFR values were mildly correlated to visual estimation of coronary stenosis (Online Figure 1).
Some of these data have been included in previous publications11,12. More specifically, 104 out of 380 lesions from Rome were included in the RINASCI study11, 138 in 141 lesions from Paris were included in the paper of Spagnoli et al12. Some of the other lesions from the CANICA group and from Portugal were included in abstracts but never published as full papers (oral presentations by Baptista et al and Martin-Reyes et al at the ESC Congress, 2014). Collectively more than 75% of the lesions were not published in full papers.
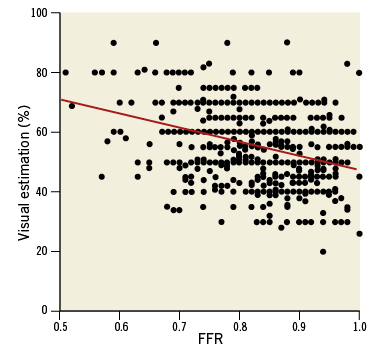
Online Figure 1. Correlation between FFR values and lesion severity by visual estimation. N.B. equal values are superimposed in the present graph.