Abstract
Aims: The need of adenosine administration for the achievement of maximal hyperaemia limits the widespread application of fractional flow reserve (FFR) in the real world. We hypothesised that Pd/Pa ratio registered during submaximal reactive hyperaemia induced by conventional non-ionic radiographic contrast medium (contrast medium induced Pd/Pa ratio: CMR) can be sufficient for the assessment of physiological severity of stenosis in the vast majority of cases. The aim of the present study was to test the accuracy of CMR in comparison to FFR.
Methods and results: Eighty patients with 104 intermediate coronary stenoses were prospectively and consecutively enrolled. CMR was obtained after intracoronary injection of 6 ml of radiographic contrast medium, while FFR was measured after administration of adenosine. Despite the fact that CMR values were significantly higher than FFR values (0.88 [IR 0.80-0.92] vs. 0.87 [IR 0.83-0.94], p<0.001), a strong correlation between CMR and FFR values was observed (r=0.94, p<0.001) with a close agreement at Bland-Altman analysis (95% CI of disagreement: -0.029 to 0.072). ROC curve analysis showed an excellent accuracy of CMR cut-off of ≤0.83 in predicting FFR value ≤0.80 (AUC 0.97 [95% CI: 0.91-0.99, specificity 96.1, sensitivity 85.7]). Moreover, no FFR value ≤0.80 corresponded to a CMR ≥0.88.
Conclusions: CMR is accurate in predicting the functional significance of coronary stenosis. This could allow limiting the use of adenosine to obtain FFR to doubtful cases. In particular, we suggest considering a CMR value ≤0.83 to be significant, a CMR value ≥0.88 as not significant, and inducing maximal hyperaemia using adenosine for FFR assessment when CMR is between 0.84 and 0.87.
Introduction
In the last decade, the development of fractional flow reserve (FFR) has provided a major shift in the assessment of coronary stenosis severity in the cardiac catheterisation laboratory. Supported by several clinical studies1-5, invasive coronary physiology has been shown to improve patient outcomes, providing a more appropriate selection of lesions which may benefit from percutaneous coronary interventions (PCI). This has led to the incorporation of FFR into coronary revascularisation guidelines, which currently recommend its clinical use based on a fixed 0.80 cut-off6-8.
Maximal hyperaemia is the crucial prerequisite to assess FFR correctly and for this purpose intravenous (i.v.) administration of adenosine is still considered the gold standard9,10. Despite compelling evidence and recommendations from guidelines, in the real world the use of FFR is far from being frequent7. The need for administering adenosine has been highlighted as one of the reasons for this underutilisation11. In fact, in addition to its cost, some patients present contraindications to adenosine infusion and, more generally, most of them find it uncomfortable. To circumvent, at least partially, these limitations, a large number of interventional cardiologists prefer the intracoronary (i.c.) route. In this regard, we recently demonstrated in the NASCI study that i.c. administration of a high-dose bolus of adenosine is safe and cost-effective compared to i.v. infusion12. However, even using this route of administration, the potential drawbacks of adenosine, such as chest pain, dyspnoea and, in particular, sinus bradycardia up to atrioventricular block (AVB), may require the interruption of FFR assessment12,13. On the other hand, administration of other potentially valuable vasodilator agents, such as sodium nitroprusside or papaverine, is again limited by their side effects on arterial blood pressure and cardiac rhythm14-18. For these reasons, adenosine-free pressure-derived indices, such as the instantaneous wave-free ratio (iFR), are currently under study19-22. However, the usefulness of these new tools is still debated, and indeed presents several limitations.
Non-ionic radiographic contrast medium, routinely used during coronary angiography, has been demonstrated to induce hyperaemia23-25, although inferior as compared to adenosine16. Thus, it is conceivable that the Pd/Pa ratio registered by pressure wire during submaximal reactive hyperaemia induced by i.c. injection of conventional non-ionic contrast medium can be sufficient for the assessment of the physiological severity of stenosis in a large number of cases, avoiding the drawbacks of adenosine injection. We called this novel index contrast medium induced Pd/Pa ratio (CMR) to avoid confusion about FFR that needs, by definition, maximal hyperaemia9. The aim of the “Rapida iniezione di mezzo di contrasto vs nitroprussiato o adenosine nelle stenosi coronariche intermedie” Rapid injection of contrast medium vs. nitroprusside or adenosine in intermediate coronary stenoses (RINASCI) study was to test the accuracy of CMR in predicting FFR in a series of consecutively and prospectively enrolled patients with intermediate coronary artery stenosis.
Methods
The RINASCI study was a prospective study designed to test the accuracy of CMR in predicting a positive FFR, in order to elaborate a possible flow chart to limit the use of adenosine to doubtful cases.
From December 2011 to April 2013, 80 consecutive patients (104 lesions) undergoing diagnostic cardiac catheterisation for suspected coronary artery disease (CAD) showing angiographically intermediate lesions (diameter stenosis 30% to 80% at visual estimation) in at least one coronary artery branch were consecutively and prospectively enrolled. Lesions localised on left and right coronary ostia were excluded. Clinical exclusion criteria were recent myocardial infarction (within seven days) or prior myocardial infarction in the territory supplied by the target vessel, severe valvular heart disease, acutely decompensated chronic heart failure, or advanced renal failure (estimated glomerular filtration rate <30 ml/min). Clinical features, cardiovascular risk factors, and left ventricular function were obtained. Cardiovascular medications were not withheld before the study. The study was approved by the local ethics committee and conformed to the Declaration of Helsinki on human research, and informed consent was obtained after complete explanation of the protocol and potential risks. Diagnostic coronary angiography was performed in all cases through the radial approach. Non-ionic radiographic contrast medium was used for all patients (Iomeron; Bracco, Milan, Italy). At least two different projections differing by more than 30° were recorded for each assessed lesion. Coronary stenoses were visually assessed by two independent expert reviewers.
PRESSURE MEASUREMENTS
After i.v. administration of heparin 100 IU/kg, a 0.014 inch pressure monitoring guidewire (PressureWire®; Radi Medical Systems, Uppsala, Sweden) was calibrated and introduced into the guiding catheter. The pressure transducer was advanced just outside the tip of a 6 Fr guiding catheter, and the pressure measured by the sensor was then equalised to that of the guiding catheter. The wire was then advanced distally to the target coronary stenosis. Special attention was paid to avoid arterial pressure wave damping, unselective catheterisation of coronary ostia and variation in the position of the pressure wire. CMR was calculated as the ratio of distal coronary pressure divided by aortic pressure obtained after achievement of submaximal hyperaemia with radiographic contrast medium. FFR was calculated as the ratio of distal coronary pressure divided by aortic pressure obtained after achievement of maximal hyperaemia. The femoral or brachial vein was used for systemic administration of adenosine. An FFR value of ≤0.80 was considered the significant ischaemic threshold.
STUDY PROTOCOL
After checking the correct position of both the guiding catheter and the pressure wire, 0.2 mg of i.c. isosorbide dinitrate were administered. The study consisted of two sequential steps separated by at least 30 seconds until the return of Pd/Pa ratio to baseline value:
1. CMR assessment: a single injection of 6 ml of radiographic contrast medium iomeprol (Iomeron; Bracco) at a flow of 4 ml/sec and at a pressure of 300 psi was performed using a power injector system (MEDRAD Avanta®; Bayer HealthCare, Warrendale, PA, USA) and the minimal CMR value obtained was recorded (in general within the first 10 seconds). Each injection of contrast medium was duplicated to test reproducibility of CMR. After any injection of contrast medium a flushing of the guiding catheter with saline was performed to avoid pressure damping due to contrast medium viscosity.
2. FFR assessment: maximal hyperaemia was induced by i.c. or i.v. adenosine administration, according to our recently proposed protocol9: in brief, we performed incremental boli of i.c. adenosine from 60 mcg to 300 mcg and up to a maximum dose of 600 mcg, if tolerated. Conversely, if the FFR value was between 0.83 and 0.81 or the patient developed a clinically relevant AVB, FFR was measured using i.v. adenosine (140 mcg/kg/min). Sodium nitroprusside was restricted to patients with absolute contraindication to adenosine.
The order of the two sequential steps was inverted after the first 50 patients to exclude an additive effect of contrast medium on maximal hyperaemia with adenosine.
Heart rate, aortic pressure, and distal coronary pressure were continuously recorded throughout all the phases of the study. Patients’ symptoms (namely an angina-like sensation, dyspnoea, or flushing), development of complete AVB, or any other complication were carefully recorded. Clinical data of the enrolled patients were collected in a dedicated electronic database at the time of the interventional procedure.
Statistical analysis
Normality was assessed by the D’Agostino-Pearson test. Categorical variables were expressed as percentages and analysed by Fisher’s exact test. Continuous variables were expressed as mean±SD and/or median (interquartile range) and compared using the paired t-test or the nonparametric Wilcoxon test, as appropriate. Considering that all analyses were performed comparing one variable to a standard reference, no corrections for multiple comparisons were made.
The relationship between CMR and FFR was quantified with a coefficient of determination (r and r2). Agreement between the two methods was assessed by Bland-Altman plots and 95% limits of agreement. The performance of CMR in predicting a positive FFR (≤0.80) was assessed using sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy, together with their 95% confidence intervals (CIs). The receiver operating characteristic (ROC) curve27 was used to measure the accuracy of the test (area under the ROC curve: AUC) and identify the CMR optimal cut-off corresponding to FFR ≤0.80 (Youden index).
The reproducibility of FFR and CMR was tested by a coefficient of determination. The primary aim of the present study was to test the accuracy of CMR in predicting a positive FFR; however, in order to be sure to have enrolled a sufficient number of lesions and considering that contrast medium induces a submaximal hyperaemia while adenosine induces a maximal hyperaemia, sample size was calculated assuming a mean FFR value of 0.87±0.07, as in the NASCI study12, and hypothesising a difference of 0.03±0.05 between CMR and FFR as the superiority threshold of FFR over CMR. According to this calculation, at least 102 lesions were required to have the 80% power to identify a significant difference between the two different approaches.
Results
PATIENTS’ CHARACTERISTICS AND SAFETY OF THE PROCEDURE
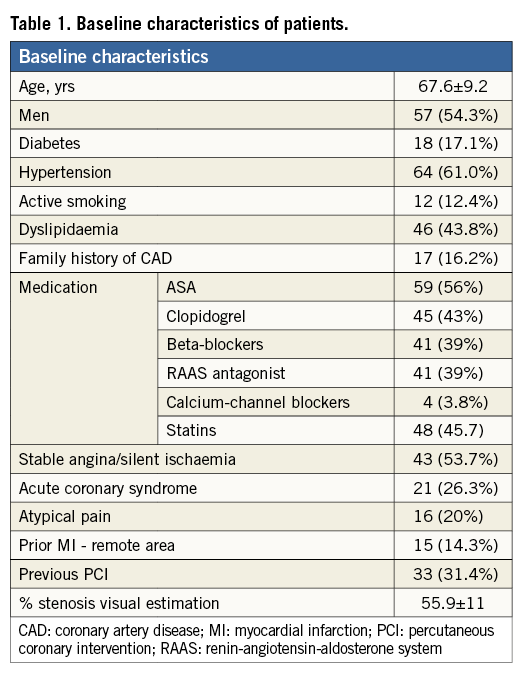
Patients’ characteristics are summarised in Table 1. The majority of patients had stable coronary artery disease. Fewer than one third of patients had a previous PCI. The average angiographic percentage stenosis was 55.9±11, and the target vessels were left anterior descending (65%), circumflex (21%), and right coronary artery (14%).
Intracoronary injection of contrast medium for CMR assessment was feasible without any symptoms in all cases. In contrast, in 13 lesions, i.c. adenosine protocol for FFR assessment was not completed because of development of complete AVB >5 s (12.5%), which was transient and spontaneously reversible in each case, thus never requiring atropine administration or temporary pacemaker implantation. In addition, 10 patients undergoing i.v. administration of adenosine complained of mild dyspnoea, chest pain and facial flushing. Collectively, a final FFR value was acquired in 74 (71%) lesions using 600 mcg of i.c. adenosine, while in the remaining cases i.v. adenosine was needed. Intracoronary administration of sodium nitroprusside, for absolute contraindication to adenosine, was not necessary in any case.
CMR VS. FFR
Median resting Pd/Pa value was 0.94 (IR 0.77-1.00). Resting Pd/Pa was significantly correlated to FFR (r=0.60, r2=0.36; p<0.001). CMR and FFR showed good reproducibility (p<0.001 with r=0.98 and p=0.001 with r=0.97, respectively). Median value of CMR was significantly higher than that of FFR (0.88 [IR 0.80-0.92] vs. 0.87 [IR 0.83-0.94], respectively, p<0.001) (Figure 1). However, we observed a strong correlation between CMR and FFR (r=0.94, r2=0.88; p<0.001; Figure 2), with a close agreement between the two indices at Bland-Altman analysis (0.02±0.02, 95% CI of disagreement: -0.03 to 0.07) (Figure 3).
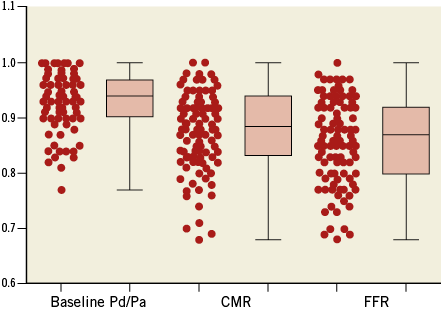
Figure 1. Values of resting Pd/Pa, contrast medium induced Pd/Pa ratio (CMR) and fractional flow reserve (FFR).
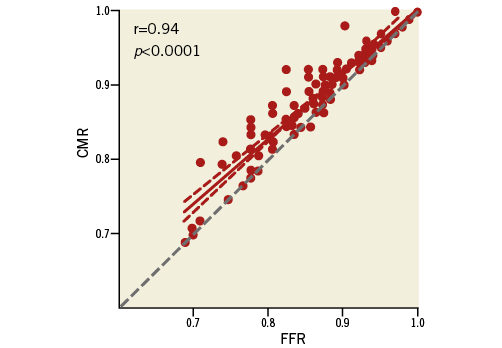
Figure 2. Correlation between contrast medium induced Pd/Pa ratio (CMR) and fractional flow reserve (FFR) values.
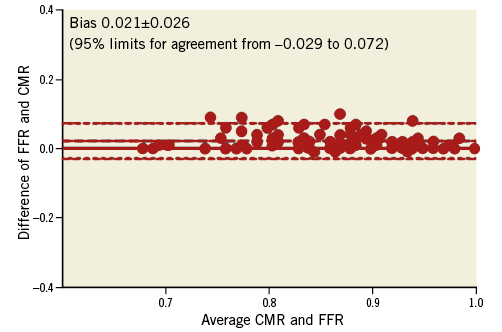
Figure 3. The Bland-Altman plot demonstrated a good agreement between contrast medium induced Pd/Pa ratio (CMR) and fractional flow reserve (FFR) across the entire range of stenosis severity (0.02±0.02, 95% CI of disagreement: -0.03 to 0.07).
ROC curve analysis showed an excellent accuracy of the CMR cut-off of ≤0.83 in predicting an FFR value ≤0.80 (AUC 0.98 [95% CI: 0.93-0.99, specificity 97.4, sensitivity 85.7]) (Figure 4). Moreover, no FFR value ≤0.80 corresponded to a CMR value ≥0.88; more particularly, using this cut-off value to classify lesions, we observed an accuracy of 85%, a specificity of 78.9%, and a negative and positive predictive value of 100% and 63%, respectively. Finally, 18 lesions were localised in the “grey zone” between 0.84 and 0.87 of CMR values; in this lesion subset, the correlation between CMR and FFR was not significant (r=0.38, p=0.12), suggesting that, between 0.84 and 0.87 of CMR values, the need of adenosine administration for FFR assessment cannot be circumvented.
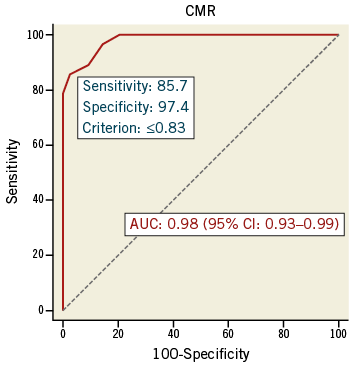
Figure 4. A receiver operating characteristic curve was calculated using the threshold cut-off for fractional flow reserve (FFR) of ≤0.80. The receiver operating characteristic was found to have an area under the curve (AUC) of 0.98 (95% CI: 0.93-0.99), suggesting high accuracy of contrast medium induced Pd/Pa ratio (CMR) in predicting positive FFR.
Discussion
The results of the RINASCI study demonstrate that contrast medium induced Pd/Pa ratio (CMR), a novel index calculated as Pd/Pa after the induction of submaximal hyperaemia using i.c. injection of standard radiographic contrast medium, is accurate in predicting the functional significance of intermediate coronary artery stenosis assessed by fractional flow reserve (FFR). This could allow limiting the use of adenosine to obtain FFR to a minority of doubtful cases.
FFR is the most accurate methodology for discriminating which lesions are or are not associated with ischaemia in the catheterisation laboratory1-5, and current guidelines recommend its use when evidence of inducible ischaemia at non-invasive stress test is not available6-8. Nevertheless, FFR is still underused in clinical practice7. Basically, this is due to some practical reasons, including the need to position a special wire with inferior handling characteristics, the need to make special connections, a lack of understanding of or belief in the concept, the lack of financial reimbursement, and finally the need for adenosine administration11. To overcome the latter limitation some authors have suggested the use of resting gradient derived measures19,20,26,27. In particular, Davies et al in the ADVISE study proposed the instantaneous wave-free ratio (iFR) as a novel adenosine-free index of stenosis severity22. The concept of iFR is based on the hypothesis that there is a diastolic “wave-free” period when microvascular resistance is already constant and minimal and consequently does not need a further vasodilation. However, any resting gradient is strictly dependent on flow and also iFR may underestimate the stenosis severity in the presence of a low basal flow: this could explain, at least partially, the imperfect correlation between iFR and FFR observed in the ADVISE study programme19,22, supporting the notion that a certain degree of hyperaemia has to be provided to identify functionally significant stenosis correctly.
Radiographic contrast medium, i.c. administered in all coronary angiography and also during FFR assessment to check the correct position of the pressure wire, is a well-known hyperaemic agent16,23,25. This effect, that seems to be principally related to its osmolality, is rapid, short acting and submaximal, and for this reason contrast medium, in general, is considered inferior to adenosine16. Nevertheless, it is conceivable that in most cases a contrast medium dependent submaximal hyperaemia could be sufficient to provide a reliable lesion severity assessment. Accordingly, in the RINASCI study we have found that the Pd/Pa ratio obtained during i.c. injection of contrast medium (which we called CMR) is effective in predicting the functional significance of intermediate coronary stenosis assessed by conventional FFR. Our data are particularly interesting because CMR could help in promoting a physiology-based approach to the treatment of intermediate coronary artery stenosis. Indeed, CMR, despite the impossibility of performing a pullback evaluation for the shortness of the contrast medium induced hyperaemia, could allow a rapid assessment of all major coronary branches limiting standard FFR with adenosine infusion to a minority of doubtful lesions. Moreover, CMR-guided PCI could be easier in comparison to FFR-guided PCI, not requiring additional adenosine and using the same amount of contrast medium needed to visualise the coronary tree during PCI. More importantly, we think that the accuracy of CMR, an index obtained during hyperaemia and consequently similar to FFR, can be considered to be higher than that reported concerning resting gradient derived measures.
Recently, in the ADVISE study, Sen et al aimed at validating the usefulness of iFR in the assessment of coronary stenosis severity22. They reported a good agreement between iFR and FFR, showing a mean difference between the two methods of 0.05±0.19 at Bland-Altman plot analysis and a close correlation between the two indices with an r value of 0.90. In the RINASCI study, we found both a higher agreement at Bland-Altman analysis (0.02±0.02) and a stronger correlation (r=0.94) between CMR and FFR. Moreover, it should be noted that most of the correlation between iFR and FFR values observed in the ADVISE study was localised below 0.60 of FFR, when measures derived from resting gradient approach those obtained after vasodilation. In contrast, in the typical intermediate coronary artery stenosis, which is the most frequent indication to FFR assessment in clinical practice, this correlation was weaker, as clearly confirmed in the ADVISE registry which enrolled patients with clinical indication to FFR assessment22. Of note, in the RINASCI study, in which only patients with intermediate coronary artery stenosis were enrolled (as clearly shown by the mean diameter stenosis and by the lack of FFR values <0.65), we also found a strong correlation in this more clinically relevant context. More importantly, we were able to identify two stringent cut-offs below and above which we can reasonably perform and defer, respectively, PCI. In fact, the CMR cut-off of ≤0.83 allows performing PCI with a 97% specificity (one false positive lesion only) while the CMR cut-off of ≥0.88 allows the 100% safe deferral of PCI (0 false negative lesions). This accuracy seems higher than that shown by Petraco et al in the ADVISE registry23, where the iFR cut-off of <0.86 to perform PCI and >0.93 to defer PCI showed a 92% predictive value for the lower cut-off but a negative predictive value of 91% for the higher cut-off. This means that almost one in 10 positive FFRs could be missed by iFR, different in comparison to our CMR cut-off ≥0.88, which was deliberately chosen to have a 100% negative predictive value. In the RINASCI study, between 0.84 and 0.87 of CMR we identified a narrow grey zone in which the predictive value of CMR was low and FFR assessment during maximal hyperaemia with adenosine is needed. Consequently, we propose a hybrid CMR/FFR approach summarised in a simple algorithm that could allow limiting adenosine administration only to a minority of doubtful cases with CMR between 0.84 and 0.87 (Figure 5). More specifically, applying this algorithm (in which we consider a CMR value ≤0.83 to be significant, a CMR value ≥0.88 as not significant, and inducing maximal hyperaemia using adenosine for FFR assessment when CMR is between 0.84 and 0.87), we would have been able to avoid the use of adenosine in 86 out of 104 lesions (83%) of the present series with a consequent saving of time and costs. This result seems to be better than the one found by Petraco et al in the ADVISE registry in which they showed that less than 60% of lesions would have been adenosine free applying the proposed hybrid iFR/FFR approach.
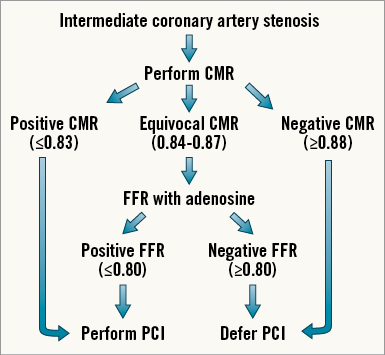
Figure 5. We propose a hybrid CMR/FFR approach summarised in a simple algorithm that could allow limiting adenosine administration only to doubtful cases. We consider a CMR value ≤0.83 to be significant and consequently we suggest performing PCI, a CMR value ≥0.88 as not significant and consequently we suggest deferring PCI, and inducing maximal hyperaemia using adenosine for FFR assessment when CMR is between 0.84 and 0.87. In view of this, PCI would be performed when FFR is ≤0.80 and deferred when FFR is >0.80.
We acknowledge that much more data on CMR (eventually using other contrast media and/or a manual injection) are needed to confirm our results and cut-offs and, more importantly, that clinical data on outcomes are required to corroborate the potential clinical relevance of this new index. However, we are confident that, for its intrinsic similarity to FFR and easiness (not needing new drugs, or software or devices), CMR may be welcome in the interventionalist’s armamentarium and could help in spreading a physiology-based approach to treatment of intermediate coronary artery stenosis. Larger, multicentre prospective studies, specifically testing the efficacy of a hybrid approach (CMR/FFR) on clinical endpoints, are needed to validate the proposed cut-offs and to confirm these promising preliminary data.
Conclusions
CMR, a novel index obtained during submaximal hyperaemia by conventional radiographic contrast medium, is accurate in predicting the functional significance of a coronary stenosis evaluated by FFR. This could allow limiting the use of adenosine to obtain FFR to a minority of doubtful cases. In particular, we suggest considering a CMR value ≤0.83 to be significant, a CMR value ≥0.88 as not significant, and inducing maximal hyperaemia using adenosine for FFR assessment when CMR is between 0.84 and 0.87. Further studies in a larger population and with clinical endpoints are required to confirm the promising findings observed in this early study.
| Impact on daily practice The need for adenosine administration to induce maximal hyperaemia is one of the limiting factors for the widespread application of FFR. The contrast medium induced Pd/Pa ratio (CMR) is a reliable, rapid and easy method to evaluate functional significance of a stenosis. The use of CMR in daily practice could help in spreading a physiology-based approach to treatment of coronary artery stenosis, limiting the use of adenosine to obtain FFR to only equivocal cases. |
Conflict of interest statement
The authors have no conflicts of interest to declare.