Abstract
Aims: Fractional flow reserve (FFR), assessed using distal coronary pressure/aortic pressure (Pd)/(Pa) ratio, functionally evaluates coronary stenosis. An assessment method without vasodilators would be helpful. A single intracoronary bolus of saline decreases Pd because of the speculated low-viscosity effect. We hypothesised that saline-induced Pd/Pa ratio (SPR) could functionally evaluate coronary stenosis. This study aimed to test the accuracy and utility of SPR for predicting FFR ≤0.80.
Methods and results: In 137 coronary lesions with over 50% angiographic diameter stenosis, SPR was assessed using an intracoronary bolus of saline (2 mL/s) for five heartbeats (SPR-5) and three heartbeats (SPR-3). FFR was obtained after intravenous adenosine infusion (140 µg/kg/min). There was a strong correlation between FFR and SPR-5 or SPR-3 (R=0.941 and R=0.933, respectively). Receiver operating characteristic (ROC) curve analysis demonstrated good accuracy (86.3%) for SPR-5, with a cut-off of ≤0.84 for predicting FFR ≤0.80 (area under ROC curve 0.96, specificity 94.3, sensitivity 79.9). Thirty-three lesions (24%) were located in the “grey zone” (SPR 0.83-0.88). No complications were observed in 673 SPR measurements.
Conclusions: SPR may accurately predict FFR and can limit adenosine use to one in four lesions. Further studies are needed to confirm the validity of SPR.
Abbreviations
AUC: area under the curve
CI: confidence interval
cFFR: contrast fractional flow reserve
FFR: fractional flow reserve
ICC: intraclass correlation coefficients
iFR: instantaneous wave-free ratio
NPV: negative predictive value
PCI: percutaneous coronary intervention
Pd/Pa: distal coronary pressure/aortic pressure
PPV: positive predictive value
ROC: receiver operating characteristic
SD: standard deviation
SPR: saline-induced Pd/Pa ratio
Introduction
In the last decade, the importance of functional assessment of coronary stenosis by fractional flow reserve (FFR) using distal coronary pressure/aortic pressure (Pd/Pa) ratio, instantaneous wave-free ratio (iFR), and resting Pd/Pa has come to light. Several studies have demonstrated improvement in patient outcomes, allowing more appropriate selection of lesions for percutaneous coronary intervention (PCI)1,2. These assessments have been incorporated into PCI guidelines3,4; nevertheless, these assessments are still underused. To achieve maximal hyperaemia for FFR assessment, intravenous administration or intracoronary high-dose bolus of adenosine has been employed5-7. However, completion of one FFR measurement using intravenous infusion of adenosine requires 4 to 5 min, and intracoronary bolus of adenosine has some potential drawbacks5-8.
Leone et al9 and Johnson et al10 have reported a high accuracy for predicting FFR ≤0.80 using contrast FFR (cFFR). cFFR is based on vasodilation-mediated hyperaemia induced by the high osmolality of contrast medium9-11. However, cFFR has a limitation resulting from the heterogeneity of osmolality among contrast media9,10, and the dose of contrast media itself is limited.
As an alternative to assessments using vasodilators or contrast media, we focused on blood viscosity. A fluid with lower viscosity can flow through arterioles at a higher rate12, resulting in its rapid exit from the arterioles to the venous system and decreased Pd. The blood flow through small vessels is inversely proportional to whole-blood viscosity12, which is affected by volume (haematocrit)13, deformation14 and aggregation of red blood cells15, and plasma viscosity16. The viscosities of whole blood at 37°C and saline are 4.0-4.5 and 1.012 mPa·s, respectively12-16. We selected saline as a low-viscosity fluid and hypothesised that we could substitute saline-induced Pd/Pa ratio (SPR) for FFR. This study was conducted to test the accuracy and utility of SPR for predicting FFR ≤0.80.
Methods
PATIENT POPULATION
Among patients undergoing cardiac catheterisation, those who underwent FFR assessment were enrolled. The inclusion criterion was a stenotic coronary lesion with over 50% angiographic diameter stenosis on visual estimation. Exclusion criteria were: 1) ostial stenosis in both the left and right coronary arteries, 2) tandem lesions, 3) acute myocardial infarction within the preceding two weeks, 4) severe valvular heart disease, 5) decompensated congestive heart failure, 6) extreme hypotension (systolic blood pressure <100 mmHg) and extreme bradycardia (<40 bpm). The study was approved by local ethics committees and conformed to the Declaration of Helsinki on human research. The study was registered with the UMIN clinical trials registry (UMIN000021357). All patients provided written informed consent after the protocol and potential risks were explained.
CORONARY ANGIOGRAPHY
Coronary angiography was performed using a 4 Fr, 5 Fr diagnostic, or 6 Fr guiding catheter. We intravenously administered 100 IU/kg of heparin prior to coronary angiography. We used a non-ionic contrast medium (Iopamiron®; Bracco, Milan, Italy). Three experienced cardiologists visually assessed the severity of coronary stenosis.
PRESSURE MEASUREMENTS
After calibration and equalisation of a 0.014-inch pressure guidewire (Certus™ and Aeris™; St. Jude Medical/Abbott, St. Paul, MN, USA), we administered intracoronary nitrates and advanced the wire distally.
The study consisted of two sequential steps:
1. SPR assessment: we administered an intracoronary bolus of saline at room temperature at 2 mL/second through the catheter using a power injector system (ACIST®; ACIST Medical Systems, Eden Prairie, MN, USA). SPR was calculated as Pd/Pa ratio after intracoronary saline injection. We defined the Pd/Pa value at the inflection point between rapid increase and plateau as the SPR value. To set the optimal duration of saline injection, we injected saline for five heartbeats (SPR-5) and three heartbeats (SPR-3).
2. FFR assessment: after intravenous infusion of adenosine (140 µg/kg/min), FFR was assessed during peak hyperaemia. To test the relationship between the saline effect and arteriolar diameter, we added an intracoronary bolus of saline for five heartbeats during FFR recording (FFR+saline).
To test reproducibility, we sequentially repeated every saline injection twice. Haemodynamic parameters were continuously recorded periprocedurally. We observed the patients’ symptoms and complications. Clinical features, coronary risk factors, left ventricular function, and medications were recorded. All patients continued their medications before and during examinations.
STATISTICAL ANALYSIS
Categorical variables were expressed as percentages and analysed using Fisher’s exact test. Continuous variables were expressed as means±SDs (standard deviations) and compared using the t-test, paired t-test, or parametric Wilcoxon test, as appropriate. We quantified the relationship between SPRs and FFR using the coefficient of determination (R or R2). The validity of lesion-level analysis according to the assumption of independence was evaluated using intraclass correlation coefficients (ICCs) of one-way random effects models for the main variables, SPRs and FFR. We analysed the agreement between SPR and FFR using Bland-Altman plots and 95% limits of agreement. We examined the performance of SPR for predicting FFR ≤0.80 using sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy, with 95% confidence intervals (CIs). The receiver operating characteristic (ROC) curve was used to measure the accuracy via area under the curve (AUC) and to identify the optimal SPR cut-off for predicting FFR ≤0.80. All statistical analyses were performed using MedCalc (MedCalc Software, Mariakerke, Belgium) and SPSS, Version 23.0 (IBM Japan, Ltd., Tokyo, Japan). FFR ≤0.80 was considered as an indication for PCI. A p-value <0.05 was considered significant.
To limit the use of adenosine to achieve at least 95% safety, we defined the equivocal SPR values as the “grey zone”, identifying the lower cut-off as the lowest SPR value with 95% specificity for FFR ≤0.80 and the upper cut-off as the lowest SPR value with 95% sensitivity for FFR ≤0.80. As in the previous studies9,10, we maximised the diagnostic accuracy using these cut-off values, limiting the use of adenosine for FFR assessment to the grey zone (hybrid approach).
In verifying the main objective of this study that “FFR ≤0.80 can be predicted with SPR”, the AUC calculated by ROC analysis was assumed to be 0.95, and a 95% CI of ±0.05 was required as the accuracy of the AUC. In the above setting, as a result of the power calculation, the required sample size was 105 lesions. After that, 137 lesions were taken as the final sample size, considering the occurrence of missing values and prediction error.
Results
BASELINE CHARACTERISTICS
From August 2015 to June 2017, we enrolled 137 (105 patients) of 152 lesions assessed by FFR, according to the inclusion and exclusion criteria. The characteristics of the study population are listed in Table 1. The target arteries were the left anterior descending (55.7%), right coronary (26.3%), and left circumflex (18.2%) arteries. Multivessel disease was found in 33 (31%) cases. SPR-5 and FFR measurements were completed in 137 lesions and SPR-3 in 112. As a result of calculating the ICC for SPR-5 and FFR in cases using data of multiple lesions, correlation within the case was found to be low (SPR-5: ICC=0.186 [95% CI: -0.205, 0.527], p=0.173; FFR: ICC=0.055 [95% CI: -0.328, 0.425], p=0.391). The validity of analysing the lesion level under the assumption of independence was proved.
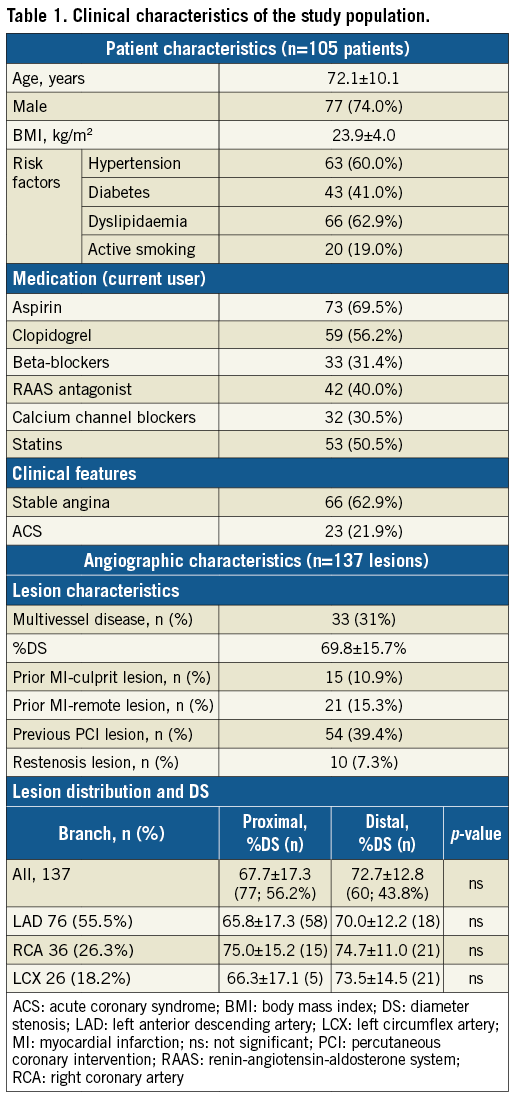
CORRELATION BETWEEN SPRs AND FFR, AND ACCURACY OF SPR FOR PREDICTING FFR
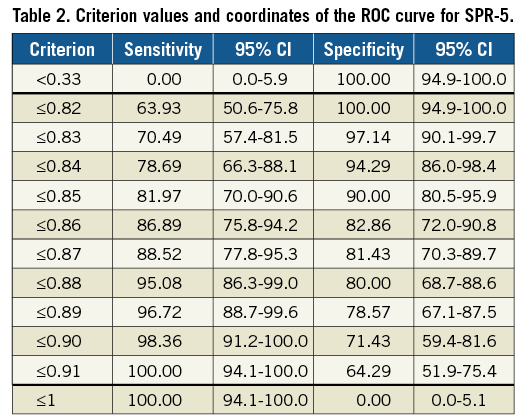
The mean value of resting Pd/Pa was 0.91±0.11 (Figure 1). The mean values of SPR-5 and SPR-3 were 0.85±0.12 and 0.86±0.12, respectively (p<0.001). The mean value of FFR was 0.80±0.13 (p<0.0001 vs. SPR-5 and SPR-3). There were strong correlations between SPR-5 or SPR-3 and FFR (R=0.941, p<0.001, and R=0.933, p<0.001, respectively) (Figure 2A, Figure 2B). We found a strong correlation between SPR-5 and SPR-3 (R=0.987, p<0.0001) and a close agreement on Bland-Altman analysis (bias: 0.01±0.005, 95% CI of disagreement: –0.03-0.05) (Figure 2C). ROC curve analysis using SPR-5 and FFR values is shown in Figure 3. The SPR-5 cut-off value for predicting FFR ≤0.80 was 0.84. The AUC was 0.96 (95% CI: 0.90-0.99, specificity 94.3, sensitivity 79.9). PPV was 92.3% and NPV was 82.3%. The diagnostic accuracy was 86.3%.
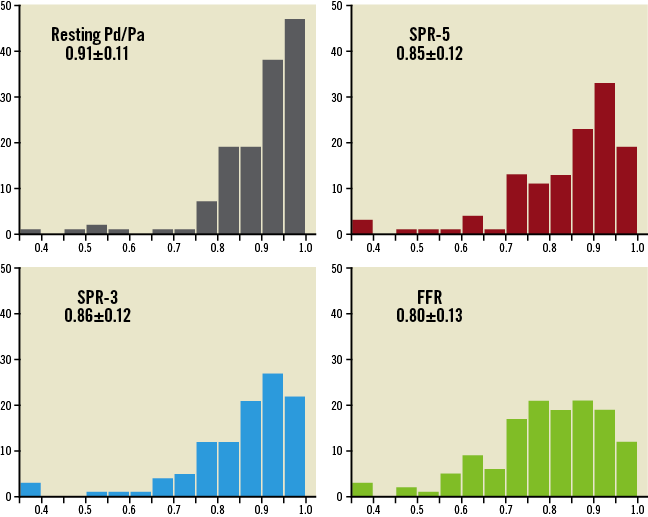
Figure 1. Distribution of pressure measurements in all patients.
Figure 2. Relationship between SPR and FFR values. A) SPR-5. B) SPR-3. Correlations were similar and good. C) Bland-Altman plot demonstrated close agreement between SPR-5 and SPR-3 (0.01±0.005, 95% CI of disagreement: –0.03-0.05). CI: confidence interval; FFR: fractional flow reserve; SPR-5, SPR-3: saline-induced Pd/Pa ratio for five and three heartbeats, respectively
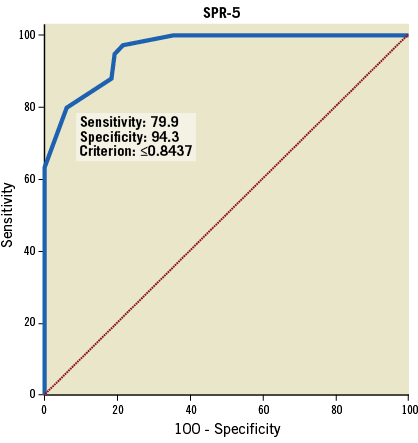
Figure 3. Receiver operating characteristic curve analysis. AUC demonstrated good accuracy of an SPR-5 cut-off of ≤0.84 for predicting FFR ≤0.80 (AUC 0.96 [95% CI: 0.90-0.99, specificity 93.0, sensitivity 79.2]). AUC: area under the curve; CI: confidence interval; SPR-5: saline-induced Pd/Pa ratio for five heartbeats
The grey zone included SPR-5 values in the range 0.83-0.88 (Table 2) (33 lesions [24%]). The hybrid approach using SPR-5 and FFR showed excellent accuracy (96%) for predicting FFR ≤0.80.
A representative case is shown in Figure 4. In SPR-5 and SPR-3 (Figure 4A, Figure 4B), resting Pa was 98 mmHg in SPR-5 and 97 mmHg in SPR-3 (red line). Three heartbeats after starting saline injection, the Pd value began to decrease rapidly from 84 to 76 mmHg in SPR-5 and from 83 to 78 mmHg in SPR-3, before reaching a plateau. Subsequently, it gradually returned to baseline (green line). The Pd/Pa value showed a rapid decrease and subsequent increase, followed by a plateau and gradual return to baseline (yellow line). SPR-5 was 0.78 and SPR-3 was 0.79 (arrows). In FFR+saline (Figure 4C), the Pd/Pa value directly returned to baseline.
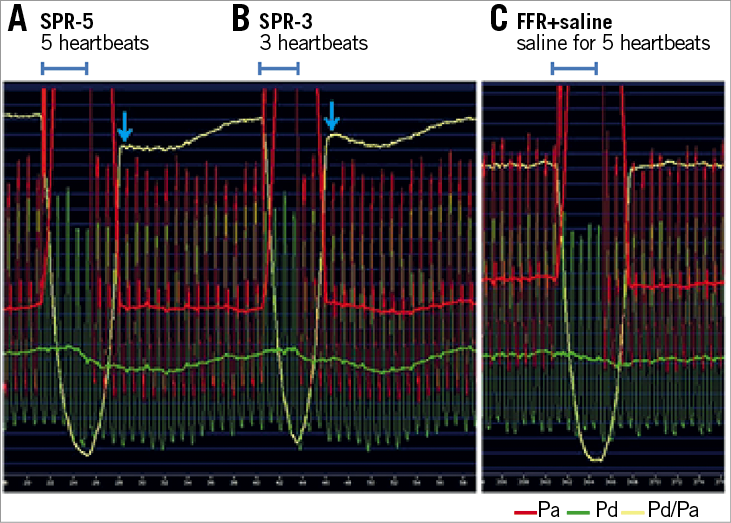
Figure 4. Pd/Pa records from a 76-year-old woman with stable angina. A) SPR-5 was 0.73 (arrow). B) SPR-3 was 0.79 (arrow). C) Additional intracoronary saline injection during FFR assessment (FFR+saline) did not affect the FFR value. FFR: fractional flow reserve; SPR-5, SPR-3: saline-induced Pd/Pa ratio for five heartbeats and three heartbeats, respectively
FFR and FFR+saline were strongly correlated (R=0.989, p<0.0001) (Figure 5), with close agreement between the two indices on Bland-Altman analysis (0.001±0.004, 95% CI of disagreement: –0.04-0.04). There was a greater difference between SPR-5 and FFR (SPR-FFR) in lesions with higher resting Pd/Pa than in lesions with lower resting Pd/Pa (Figure 6).
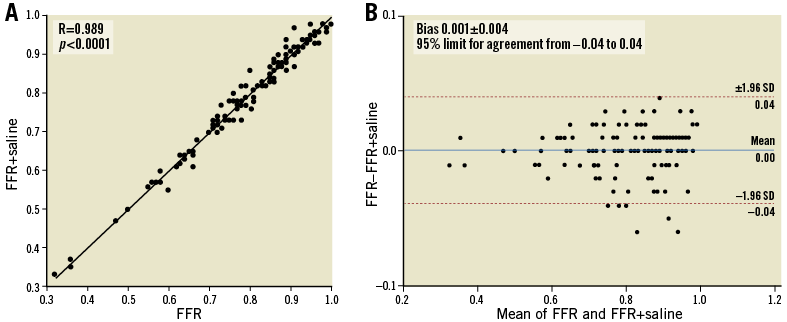
Figure 5. Relationship between FFR and FFR+saline. A) Excellent correlation between FFR and FFR+saline was observed. B) Bland-Altman plot demonstrated a close agreement between FFR and FFR+saline (0.001±0.004, 95% CI of disagreement: –0.04-0.04), suggesting additional saline injection did not affect FFR values. CI: confidence interval; FFR: fractional flow reserve; FFR+saline: additional saline injection during FFR recording
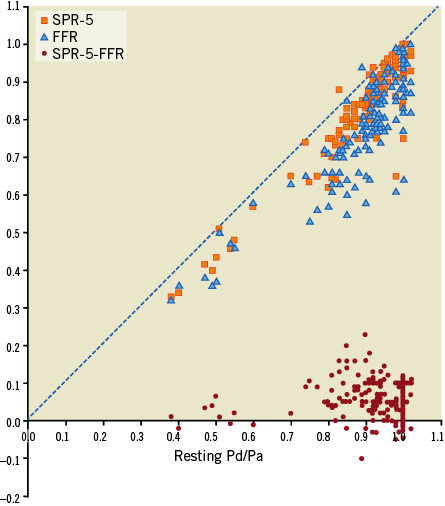
Figure 6. Relationship between resting Pd/Pa and SPR-5, FFR and (SPR-5 - FFR). SPR-5 - FFR values are obviously larger in the lesions with higher resting Pd/Pa than in the lesions with lower resting Pd/Pa. FFR: fractional flow reserve; SPR-5: saline-induced Pd/Pa ratio for five heartbeats; SPR-5 - FFR: difference between SPR-5 and FFR
INFLUENCE OF CATHETER SIZE ON SPR AND REPRODUCIBILITY OF SALINE INJECTION
We used 4 Fr and 5 Fr diagnostic catheters in 78 and 11 lesions, respectively, and 6 Fr guiding catheters in 48 lesions. SPR-5 and FFR were strongly correlated in the 4 and 5 Fr diagnostic catheter group (n=89, R=0.908). There was also a strong correlation in the 6 Fr guiding catheter group (R=0.952). The ICCs showed absolute agreement between the first and second SPR measurements at a high level (ICC=0.996 [95% CI: 0.994, 0.998], p<0.0001).
COMPLICATIONS
In 673 SPR assessments, no complications were observed. In contrast, during FFR assessments, nearly 20% of patients complained of chest discomfort and one experienced severe hypotension.
Discussion
SPR assessment requires only a single intracoronary saline bolus. The results of this study demonstrated high accuracy of SPR for predicting the functional significance of coronary stenosis assessed by FFR in lesions excluding tandem stenosis. We found an excellent agreement between SPR-5 and SPR-3, a lower mean value and a slightly better correlation with FFR for SPR-5 than for SPR-3. The interval before returning to baseline in both Pd and Pd/Pa values was 10%-20% longer for SPR-5 than for SPR-3. These differences might be due to more heartbeats of saline streaming through the arterioles and complete replacement of blood with saline in SPR-5. Hence, SPR-5 is more appropriate for assessment.
MECHANISM OF SPR
The potential mechanisms of increase in coronary flow induced by intracoronary saline administration still remain unclear. De Bruyne et al demonstrated increases of epicardial coronary flow velocity by continuous intracoronary saline infusion (~20 mL/minute) in patients free of stenosis17. They proposed mechanisms of hyperaemia induced by continuous saline infusion, such as temperature of saline, decreased local arterial oxygen content, myocardial ischaemia, or endothelial paracrine pathways. In their study, the decrease in Pd value began 20 seconds after starting the saline infusion. This implies that hyperaemia appeared within ~20 seconds from starting saline infusion in non-stenotic coronary arteries. In our study, saline injection (2 mL/sec) in a coronary artery with a stenotic lesion caused the Pd value to decrease within only three to four heartbeats (Figure 4). Saline mainly streams through the epicardial coronary artery during this initial period of three to four heartbeats after starting saline injection, and subsequently begins to stream through the arterioles. Therefore, Pd decreases seem to appear too soon and are too rapid to be explained by hyperaemia.
From these findings, we speculate that the low viscosity effect is the most probable mechanism of SPR. When saline begins to stream through the arterioles (second period), the viscosity begins to decrease rapidly in the arterioles and the Pd value immediately begins to decrease rapidly. When saline continues to stream through the arterioles (third period), viscosity stays at the minimum and the Pd value plateaus. When saline is gradually replaced with blood again (fourth period), viscosity increases gradually and the Pd value gradually returns to baseline. During the third and fourth periods, the Pd/Pa value plateaus and is followed by a gradual return to baseline. As an additional mechanism, it is possible that hyperaemia induced by saline injection appears in the mid to late phase of the process, earlier than reported in the study by De Bruyne et al because saline was injected at a higher flow rate in our study. The appearance of reactive vasodilation in the third period might be one of the reasons for the gradual return of Pd value to baseline.
Temporary decreases in Pd and Pd/Pa were seen during the third period in 13 SPR assessments (eight SPR-5s and five SPR-3s), especially when repeating saline injections within a short interval (Figure 4A, Figure 4B). Most accompanied a temporary decrease in systemic blood pressure. De Bruyne et al demonstrated no effect of intracoronary saline infusion (~20 mL/min) on left ventricular function in patients without coronary stenosis18. However, we speculate that, in patients with coronary stenosis, temporary myocardial ischaemia enhanced by intracoronary saline injection followed by a short interval may depress ventricular function, resulting in temporary decreases of Pa and Pd values. Therefore, the inflection point is considered adequate as an SPR value to avoid this.
Additional intracoronary boluses of saline (FFR+saline) did not affect FFR values (Figure 5), suggesting that the low viscosity effect does not appear under the condition of maximally dilated arterioles.
LIMITATIONS OF CURRENT ASSESSMENT METHODS
Despite the importance of patient outcome demonstrated by the FFR study18, FFR has remained underused because of the need for adenosine and procedural inconvenience5,6. Additionally, the issue of insufficient arteriolar dilation by adenosine remains unsolved. A simpler method that can easily predict FFR ≤0.80 would be useful for the widespread application of FFR. Leone et al demonstrated a high accuracy (89%) of cFFR for predicting FFR ≤0.80 using multiple contrast media9, and Johnson et al also reported the high accuracy (83.5%) of cFFR using eight different contrast media10. However, the heterogeneity among different contrast media was not examined in either study. Furthermore, cFFR requires more additional doses of contrast medium to assess multiple lesions. These disadvantages would limit its widespread application. In contrast, although iFR and resting Pd/Pa are simple methods that do not require agents and have shown patient outcomes in large patient populations1,2, both assessments have an accuracy of around 80% for predicting FFR ≤0.8019.
ACCURACY AND UTILITY OF SPR
We demonstrated high accuracy (86.3%) of SPR-5 for predicting FFR ≤0.80. The grey zone of SPR included 24% of lesions, almost identical to the 22% seen with cFFR (adenosine zone)9. Using SPR, the use of adenosine for FFR assessment is limited to one in four lesions. SPR assessment does not require any vasodilator agent or contrast medium and has advantages, such as its simplicity, low cost, speed, easy repeatability, and safety. Since one SPR measurement requires 6 to 10 mL of saline and only 20 heartbeats, we can repeat measurements sequentially several times if needed. Furthermore, we can use SPR for assessing multiple lesions without being concerned about the dose of contrast medium or the time needed for assessments. More importantly, SPR data are applicable around the world.
Finally, SPR reflects not only the ability of stenotic coronary lesions to supply blood but also the basal condition of arteriolar dilation induced by myocardial ischaemia if the primary mechanism is a low viscosity effect. In contrast, arterioles are maximally dilated by adenosine for FFR assessment. In this study, we demonstrated excellent agreement between FFR and FFR+saline (Figure 5) and obviously larger differences between SPR and FFR values (SPR-FFR) in the lesions with higher resting Pd/Pa than in the lesions with lower resting Pd/Pa (Figure 6). These two findings imply that arterioles distal to the stenotic lesions are dilated proportionally in response to basal myocardial ischaemia. It is possible that combined assessment of SPR and FFR has the potential to characterise the microcirculatory condition in acute coronary syndrome. Furthermore, it is possible that arteriolar dilation induced by adenosine for FFR assessment might be insufficient when SPR-FFR is a small or negative value. We expect the combined assessment of SPR and FFR to be useful to detect these insufficient assessments using adenosine.
Study limitations
We excluded patients with extreme bradycardia because of the possibility of ventricular arrhythmia. Therefore, SPR-3 might be safer for these patients. We also excluded patients with ostial stenosis because it would require much more saline for complete replacement, leading to severe depression of left ventricular function or dangerous arrhythmia. SPR assessment cannot perform pullback evaluation due to the short-term effect of saline. Finally, and most importantly, since the size of our patient population was quite small, further studies are needed to confirm the validity of SPR. We expect that studies with a larger population including tandem lesions could provide useful information in order to understand the basal condition of arterioles induced by the combination of multiple lesions.
Conclusions
SPR is a novel method without any agents based on the speculated low viscosity effect. It is a simple, easy-to-use, safe, and useful method for predicting the functional significance of coronary stenosis assessed by FFR, with high reliability and easy repeatability. Using SPR, we can easily apply the results from previous studies indicating patient outcomes and limit the use of adenosine for FFR assessment to one in four lesions.
| Impact on daily practice To apply the results from previous FFR studies in clinical practice, SPR can easily and accurately predict FFR. SPR needs no vasodilators or contrast medium and requires ≤10 mL of saline and 20 heartbeats. Using SPR, we can limit the need for adenosine for FFR to one in four lesions. |
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing and publication support.
Conflict of interest statement
The authors have no conflicts of interest to declare.