Abstract
Fractional flow reserve (FFR) is a useful tool for the evaluation of coronary bifurcation lesions. FFR can guide treatment strategy, simplify the procedure and reduce unnecessary complex interventions. However, the application of FFR to complex bifurcation lesions requires a comprehensive understanding of its roles and potential pitfalls. Furthermore, FFR should be interpreted in the context of complex bifurcation anatomy and physiology rather than as a simple number. Finally, it should be recalled that the ischaemic burden is more important than the presence of ischaemia, and the risk/benefit of a complex intervention should be incorporated into the treatment decision after FFR measurement.
Abbreviations
FFR: fractional flow reserve
LAD: left anterior descending artery
LCX: left circumflex artery
PCI: percutaneous coronary intervention
QCA: quantitative coronary angiography
Introduction
Coronary bifurcation lesions possess unique anatomic and physiologic characteristics. The amount of myocardium supplied by the side branch is variable, the pattern of luminal narrowing is complex and differs between main and side branches, and the coronary flow through the main vessel and side branch changes dynamically during the intervention1. Fractional flow reserve (FFR) estimates the ratio of maximal flow in the presence of coronary artery stenosis to the normal maximal flow2. Clinically, FFR is measured by the ratio of distal coronary pressure to aortic pressure under the condition of pharmacologically induced hyperaemia. An FFR-guided intervention strategy has been shown to improve clinical outcomes over medical treatment or an angiography-guided intervention strategy in patients with coronary artery disease3-5. While FFR-guided bifurcation intervention has been demonstrated to be safe and effective, the application of FFR to bifurcation lesions requires a comprehensive understanding of its roles and potential pitfalls. In this review, we focus on the roles and potential drawbacks of FFR in bifurcation lesions.
FFR for the guidance of revascularisation in coronary bifurcation lesions
The inherent limitations of angiographic evaluation for bifurcation lesions are well known6-9. Although invasive imaging tools such as intravascular ultrasound or optical coherence tomography can provide complementary anatomical information, their diagnostic accuracy in predicting the functional significance of bifurcation lesions has been reported to be relatively low (Figure 1)1,10,11.
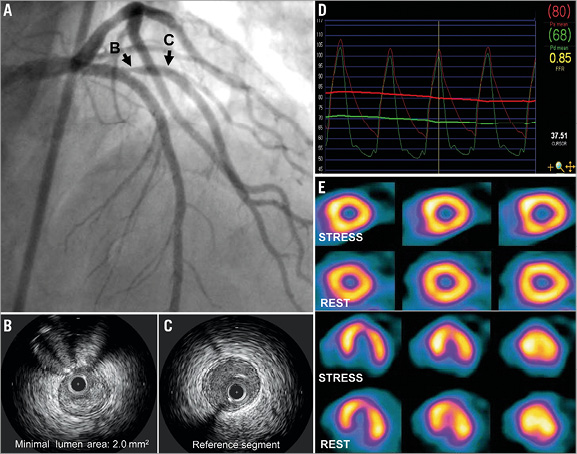
Figure 1. The discrepancy between the anatomical and the functional significance of a side branch. Angiography showed a significant stenosis at the ostium of a large first diagonal branch (A). By intravascular ultrasound, minimal lumen area at the ostium was 2.0 mm2 (B & C). Nonetheless, FFR of a diagonal branch was 0.85 (D) and there was no reversible perfusion decrease in a myocardial perfusion imaging study (E).
A large part of the clinical benefit of FFR-guided revascularisation is the reduction of percutaneous coronary intervention (PCI)-associated complications in vessels that do not require revascularisation. This benefit is likely to be maximal in patients with bifurcation lesions, as PCI for bifurcation lesions is a predictor of periprocedural myocardial infarction12, and stent thrombosis is more frequent after stenting for bifurcation lesions13.
Before the intervention, the use of FFR is generally recommended to evaluate the functional significance of main branch stenosis or pure side branch stenosis (Medina 0,0,1) (Table 1). During PCI, FFR is a useful tool to decide whether additional interventions are required in the jailed side branches. Following the work by Koo et al, several studies have consistently shown the limitations of angiographic % diameter stenosis (%DS) in identifying functionally significant jailed side branches (Table 2, Figure 2A)9,14-17. These results imply that FFR can simplify bifurcation PCI by restricting additional treatment of jailed side branches to those without functional significance. However, the operator needs to balance the risk and benefit of FFR measurement for jailed side branches. FFR measurement is most effective when measured in a large side branch with a short ostial lesion.
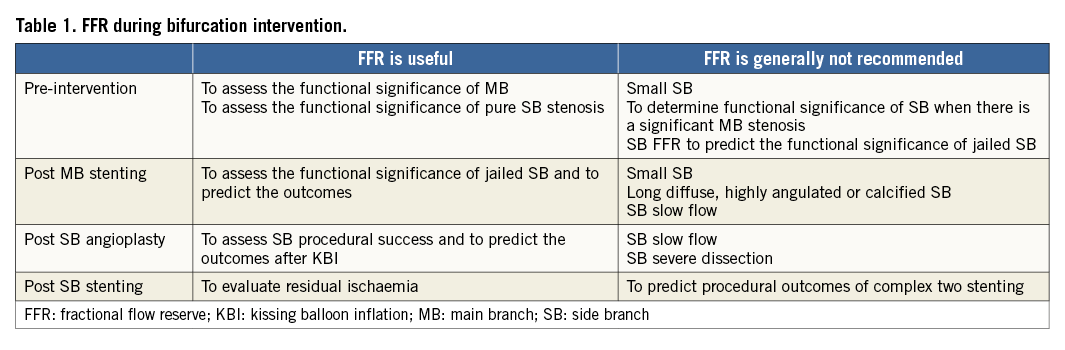
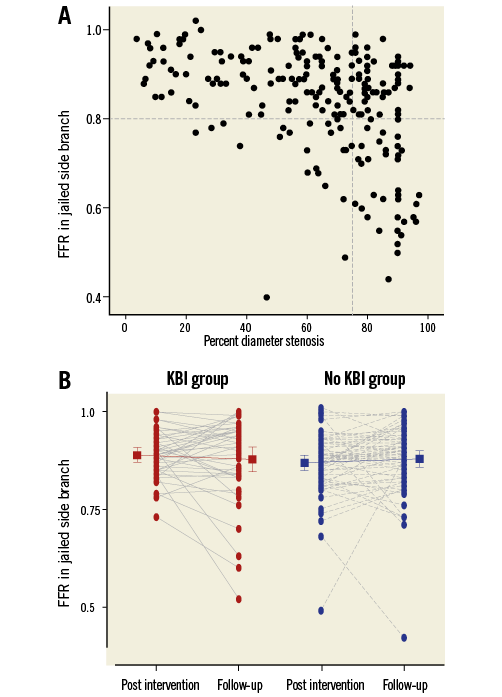
Figure 2. FFR and angiographic percent diameter stenosis in jailed side branches. A) The data of 242 jailed side branch lesions were pooled from the Seoul National University Hospital (SNUH) side branch FFR registry, the Nordic-Baltic Bifurcation III substudy and Bellenger et al14,16,18. Angiographic % diameter stenosis showed a modest correlation with FFR (r=–0.423, p<0.001). Using receiver-operating curve analysis, the AUC of % diameter stenosis to predict FFR <0.80 was 0.729 (95% CI: 0.656-0.801, p<0.001). B) Among the 242 jailed side branch lesions, 113 lesions underwent serial FFR measurement at six to eight-month follow-up9,16. Side branch FFR was maintained regardless of final KBI or not (0.89±0.06 to 0.88±0.11 in the final KBI group [p=0.406] and 0.87±0.08 to 0.88±0.09 in the no KBI group [p=0.332]). FFR: fractional flow reserve; KBI: kissing balloon inflation
FFR is also useful to assess the procedural success and to predict functional and clinical outcomes after side branch intervention (Table 1). Through serial FFR measurements, Koo et al showed that side branch FFR was not changed significantly during follow-up (0.86±0.06 to 0.84±0.01, p=0.4 in a kissing balloon group and 0.87±0.06 to 0.89±0.07, p=0.1 in a non-kissing balloon group, respectively) (Table 2)9. The Nordic-Baltic Bifurcation III trial substudy showed similar findings16. Therefore, immediate post-intervention side branch FFR appears to be a useful index to predict the functional outcomes of the jailed side branches during follow-up (Table 1, Figure 2B). However, functional and angiographic late loss is also dependent on the degree of injury from the intervention. After two-stenting, FFR can be helpful to detect the residual ischaemia. However, it should be noted that a high side branch FFR does not always guarantee procedural success and favourable clinical outcomes1,18.
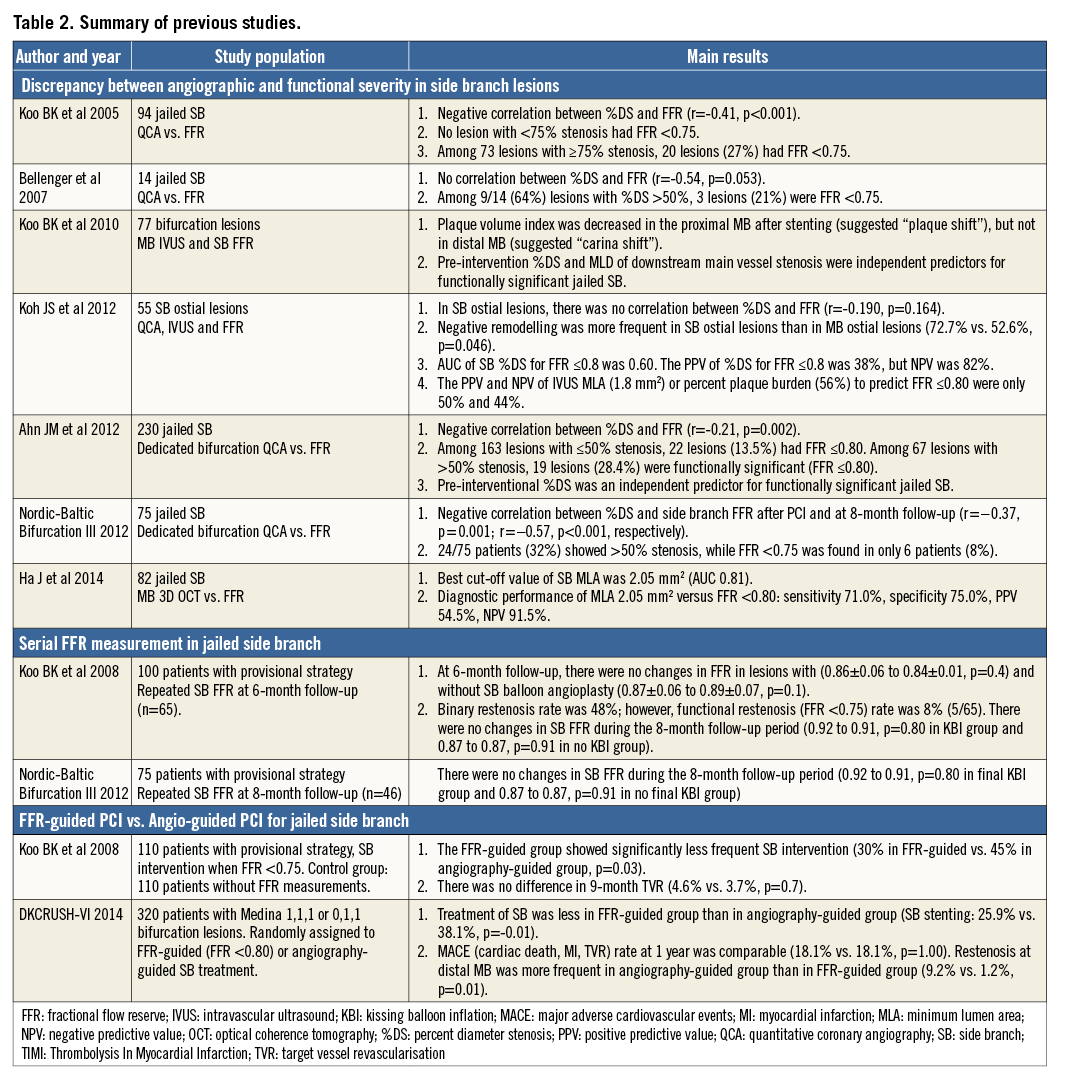
Clinical outcomes of FFR-guided side branch intervention strategy
A previous study comparing clinical outcomes between patients undergoing side branch intervention with and without FFR-guided revascularisation9 showed that there was no difference in nine-month clinical outcomes between the two groups. However, the FFR-guided group received fewer side branch interventions (30% in the FFR-guided vs. 45% in the angiography-guided group, p=0.03). The recent DKCRUSH-VI study randomly assigned patients with Medina 1,1,1/0,1,1 bifurcation lesions into an FFR-guided side branch treatment group (n=160) versus an angiography-guided side branch treatment group (n=160) (Table 2)19. The angiography-guided group received more side branch intervention (angioplasty: 56.3% vs. 63.1%, p=0.07; stenting: 25.9% vs. 38.1%, p=0.01) without any difference in major adverse cardiac events at one year (18.1% vs. 18.1%, p=1.00). Interestingly, the restenosis rate at the distal main vessel was higher in the angiography-guided group (9.2% vs. 1.2%, p=0.01) (Table 2). These study results demonstrated the benefit (less unnecessary side branch intervention) and limitation (no benefit in clinical outcomes) of FFR-guided side branch intervention when used in general bifurcation lesions.
Theoretical and practical limitations of FFR in bifurcation lesions
LOW FFR VS. CLINICAL RELEVANCE
It is well established that myocardial ischaemic burden is clinically more important than the simple presence of ischaemia20,21. As side branch territory is smaller than main branch territory, not all side branches with low FFR will cause clinically relevant ischaemia. The different clinical, electrocardiographic, and physiologic relevances between main and side branches were recently demonstrated by one-minute occlusion test22. In this study, occlusion of the diagonal branch resulted in less pain, less ST-segment elevation and fewer QT-segment disturbances than LAD occlusion22. Therefore, to prove the benefit of revascularisation of side branch intervention over medical treatment, clinically significant side branches which supply large myocardial territory should be identified prior to FFR measurement. However, the best method to determine clinically significant side branches still remains unclear. In a BBC/Nordic Bifurcation Study population, a provisional strategy was better than a two-stenting strategy in all subgroups including large side branches (>2.75 mm in diameter or equivalence between main and side branches)23. Recently, a scoring system incorporating a combination of three angiographic parameters (size, number, and location of side branches) was reported to discriminate the clinical relevance of side branches better than vessel size alone22. Further studies are needed to define clinically relevant side branches better in the catheterisation laboratory.
INFLUENCE OF DOWNSTREAM OR UPSTREAM STENOSIS ON FFR
The pressure gradient is dependent on the flow across a stenosis. As blood flow to the side branch is less than that to the main branch, side branch FFR is more easily influenced by the presence of additional upstream and downstream stenoses. Therefore, careful angiographic assessment and pressure pullback tracing under sustained hyperaemia are mandatory to understand the meaning of low FFR in a side branch adequately (Figure 3). By a more complicated interaction of a branching system, the presence of a critical stenosis at one branch can divert flow more to the other branch and influence FFR value (branch steal phenomenon)24.
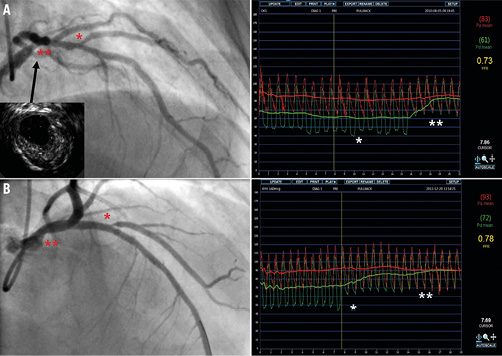
Figure 3. Influence of upstream stenosis on side branch FFR. A) Angiography showed a Medina 0,0,1 lesion and FFR measured at a side branch was 0.73. However, pressure pullback tracing from the diagonal branch to the left main ostium under sustained hyperaemia revealed the pressure step-up at the distal left main (**), but not at the ostium of the diagonal branch (*). This finding suggested that the primary lesion for low FFR was the distal left main lesion which was revealed by intravascular ultrasound. B) FFR measured at a side branch was 0.78, and pressure step-up mainly occurred at the side branch ostium (*), not at the distal left main (**). These two cases show the importance of pressure pullback tracing to determine the relative contribution of proximal main branch and side branch lesions for side branch FFR. FFR: fractional flow reserve
FFR for left main bifurcation
In general, similar principles for using FFR for non-left main bifurcation lesions can be applied to left main bifurcation lesions with a few caveats. First, the left main bifurcation is exposed to the highest blood flow in the human coronary circulation system, and both branches are clinically relevant. Second, as most patients with left main bifurcation lesions have additional stenoses, the influence of downstream stenoses on measured FFR value should always be considered (Figure 4). For instance, when there is a significant downstream stenosis in the proximal LAD in a patient with an intermediate distal left main lesion, FFR measured in a non-diseased left circumflex artery underestimates the severity of a left main lesion due to reduced coronary flow caused by downstream stenosis in the proximal LAD. However, clinically significant FFR change occurs only when the downstream stenosis is located in the proximal portion of the coronary artery and is very severe25,26.
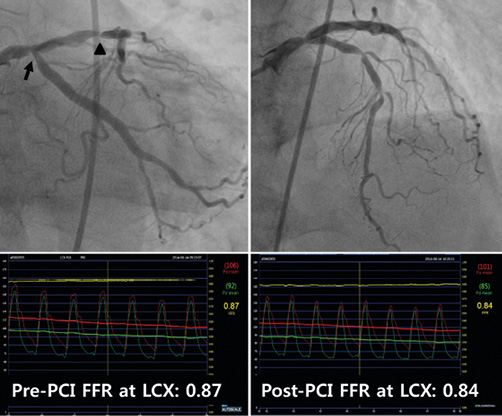
Figure 4. FFR for intermediate left main disease with a downstream stenosis. This patient had intermediate stenoses at the left main coronary artery and at the ostium of LCX and critical stenoses at LAD. Before the intervention of LAD stenoses, FFR measured at distal LCX was 0.87. After stenting of LAD stenoses, FFR at distal LCX decreased to 0.84. FFR: fractional flow reserve; LAD: left anterior descending coronary artery; LCX: left circumflex artery; PCI: percutaneous coronary intervention
Summary
FFR is a useful tool for the evaluation of coronary bifurcation lesions. FFR can guide treatment strategy, simplify the procedure and reduce unnecessary complex interventions. However, the operator should have an adequate understanding of coronary bifurcation physiology and the possible pitfalls of FFR. Finally, it should be remembered that the ischaemic burden is more important than the presence of ischaemia or measured FFR value, and the risks/benefits of complex intervention should be incorporated into the treatment decision after FFR measurement.
Conflict of interest statement
B-K. Koo has received an institutional research grant from St. Jude Medical. N. Curzen has received an unrestricted research grant and speaker/consultancy fees from St. Jude Medical and speaker fees and educational funds from Volcano. The other authors have no conflicts of interest to declare.

