One of the most likely reasons behind the success of congress sessions on percutaneous interventions (PCI) in bifurcations, always packed with attendees, is that this PCI indication leaves little room to the interventionalists for self-indulgency. While some operators may find relief in not embarking on treating chronic total occlusion on the grounds of alleged unproven benefit, or leave unprotected left main stenoses to the well-accepted alternative of surgical treatment, bifurcation stenoses constitute a too frequent scenario that invariably the interventionalist has to face… along with its unpredictable results.
By far, the most feared complication in bifurcation PCI is side branch occlusion. Adequate triage of this complication, thorough procedure planning and adequate selection of hardware is of critical importance in making the procedure successful and safe. Single stent techniques have been demonstrated to be safer than more complex double stent or dedicated stent approaches, and have been recommended as the technique of choice whenever deemed as appropriate1. Yet, a dubious angiographic result of the side branch covered by the stent often occurs after stent deployment.
If angiographic assessment of bifurcations is always complex, it certainly becomes even more difficult after stent jailing of the side branch. Frequently, visualisation of the side branch ostium is possible from only one angiographic projection, impeding assessment of lumen eccentricity. Stent radiopacity, image filtering and edge enhancement by digital angiography, along with incomplete mixing of blood and contrast medium due to turbulences, contribute to impair its visualisation. Previous work has demonstrated that angiographic estimates of side branch compromise by the stent do not reflect haemodynamic relevance as assessed with pressure guidewires2. It is in this context of uncertainty where the operator has to decide whether the stent should be opened at the side branch ostium by performing kissing balloon dilatation (KBD).
In this issue of EuroIntervention, Kumsars et al report on the results of the Nordic-Baltic Bifurcation Study III FFR substudy3. In that trial, a randomised comparison of two different simple stenting approaches to the treatment of coronary bifurcation stenoses, plain main branch stent implantation with and without final KBD. In this FFR substudy, the authors used pressure guidewire to assess the functional result of each strategy. A difference with prior studies, the operators made no decisions in the index procedures based on FFR evaluation of the side branch after stenting. Long-term functional follow-up with new FFR measurements was performed in around 60% of patients. An FFR cut-off value of 0.75 was chosen to be comparable with prior research on the field2.
The authors found that angiographic assessment of side branch narrowing cannot be used to ascertain its haemodynamic impact. Asubstantial proportion had an associated FFR >0.75 irrespective of its angiographic severity. This supports not only the results of previous work by other authors, but also the everyday observations made by an increasing number of interventional cardiologists using FFR to assess the results of jailed side branches (Figure 1). More importantly, by performing a prospective functional follow-up of the patients included in the study, Kumsars et al investigated to what extent FFR measurements obtained in an acutely pinched side branch ostium are predictive of long -term functional outcome. This is an issue of great importance, since our knowledge concerning the substrate of post-stent ostial narrowing, a combination of stent struts, dissection flaps, displaced carina and traumatised vessels with negative remodelling, challenges the concept of predicting long-term functional outcome on the grounds of acute FFR measurements. The observations collected by the Nordic-Baltic Bifurcation Study III investigators confirm that acute FFR measurements in jailed side branches correlate well with those repeated in the long term. These results confirm previous observations made in the same line, and support the use of FFR as a clinical decision-making tool during bifurcation PCI.
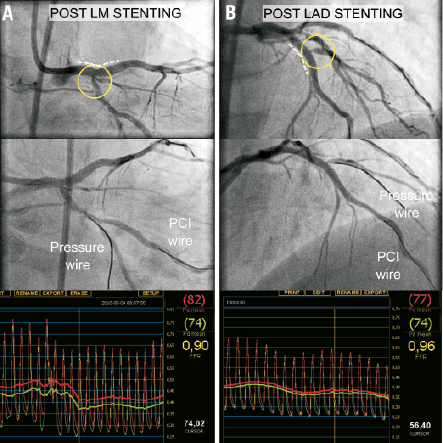
Figure 1. How frequently does side branch compromise occurs in practice? This figure shows the value of fractional flow reserve in the assessment of two jailed side branches during percutaneous revascularisation in the same patient and during the same intervention. Panel A: After implantation of a drug-eluting stent in a left main stenosis (dotted line), an angiographic narrowing (60% DS) became evident in the jailed circumflex branch. An FFR of 0.90 was documented and no further intervention was performed at this level. Panel B: A mid LAD stenosis was then treated at a bifurcation with a diagonal branch. After stent implantation (dotted line) an angiographic stenosis developed at the ostium of the jailed diagonal branch with TIMI III flow. A pressure guidewire was crossed through the stent struts and FFR was measured. On the grounds of the result obtained (FFR 0.96) no additional action was taken regarding the diagonal branch. The patient evolved favourably during hospital stay and remained free of angina at follow-up. Reprinted with permission from reference 5.
The fact that in this study stenosis severity of the jailed side branches was lower than in previous studies2 merits some comments. Although this can be due to selection bias, we should keep in mind the difficulty and variability of objective angiographic assessment for jailed side branches. In addition to the difficulties mentioned earlier, it is virtually impossible to obtain with QCA a>70% diameter stenosis reading in a side branch ostium without introducing manual corrections. Angiographic severity of the jailed side branch is also influenced by the endurance of the operator in getting the best angles. Finally, the obtained FFR measurement in ajailed side branch ostial lesion is influenced not only by the degree of luminal narrowing, but also by lesion length, non-ostial side branch stenosis and main branch stenosis. Surely these factors have influenced the differences in angiographic data between this and other studies, although it is unlikely that this might affect the main conclusions drawn by the authors.
It is also important to analyse the results of these interventions from the standpoint of the conclusions of the Nordic-Baltic Bifurcation Study III. Although in the study the angiographic outcome of the side branch was better in cases treated with KBD (particularly in true bifurcation lesions), no translation to clinical benefits was noted in the long-term. In non-true bifurcation stenoses, KBD had no effect on long-term clinical and angiographic endpoints. These finding are congruent with the functional results reported in the present FFR substudy. Furthermore, like in any stenosis interrogated with pressure guidewires, the prognostic relevance of a jailed side branch with FFR<75% has to be interpreted taking into consideration the amount of myocardium in the distribution territory of that branch, an information not implicit in the obtained FFR measurement that has to be estimated separately by the operator as part of the decision making process.
From the technical point-of-view, one of the lessons learned from this paper is that assessment of side branch pinching after PCI with a pressure guidewire is more tricky that measuring FFR in de novo intermediate coronary stenoses. In 10% of the cases the authors had to abandon FFR measurement in the side branch due to dissection or failure to negotiate the wire. Several tips and tricks should be learned for this indication. As an example, when a microcatheter is used to interchange a conventional wire by the pressure guidewire through the stent struts, it is mandatory to ensure that this new device is not interfering with FFR measurements. Likewise, damage of the pressure sensor is more likely to occur due to the friction of the pressure guidewire against stent struts when crossing to the side branch.
In summary, the results of the Nordic-Baltic Bifurcation Study III FFR substudy constitute good news for the interventional cardiologist. Functional guidance in bifurcation PCI will contribute to simplify many bifurcation PCI procedures, avoiding unneeded interventions on jailed branches with adequate FFR despite their angiographic appearance, and identifying those cases that may deserve further treatment on the grounds of suboptimal functional result. These observations, now in paper, have already influenced the recommendations issued by expert associations like the European Bifurcation Club4. Safety and cost-effectiveness issues have not been explored in this study, but everything seems to indicate that functional guidance in this patient subset might be also beneficial from this perspective. This evidence adds one more argument supporting the adoption of FFR in clinical practice, not only for the interrogation of intermediate coronary stenoses, but also to assess the results of PCI.
Conflict of interest statement
The author has no conflicts of interest to declare.
References

