Bifurcation lesions are present in 15 to 20% of the patients undergoing percutaneous coronary interventions (PCI)1,2 and are associated with increased rates of in-stent restenosis3 and stent thrombosis4.
The current consensus in the treatment of bifurcation lesions is to use the provisional single stent approach as the default strategy5. This consensus is based on large randomised trials, comparing single- with two-stent techniques, such as the Nordic6, CACTUS7 and BBC-18 trials (Table 1). Of these trials, Nordic and CACTUS showed similar clinical outcomes with single stenting when compared with a two-stent strategy. However, in these two trials, procedure duration was longer and x-ray dose higher in the two-stent group thus favouring the use of the provisional single-stent technique. In BBC-1, there was a difference in MACE rates seen favouring the single-stent group (15.2% versus 8.0%). However, this difference was mainly driven by periprocedural myocardial infarctions (MI), of which the clinical implications are still under debate. It could be concluded that, based on these trials, the single-stent technique is not by definition more effective, but safer if compared with the two-stent technique using conventional stents. This justifies the current preference for the single-stent approach.
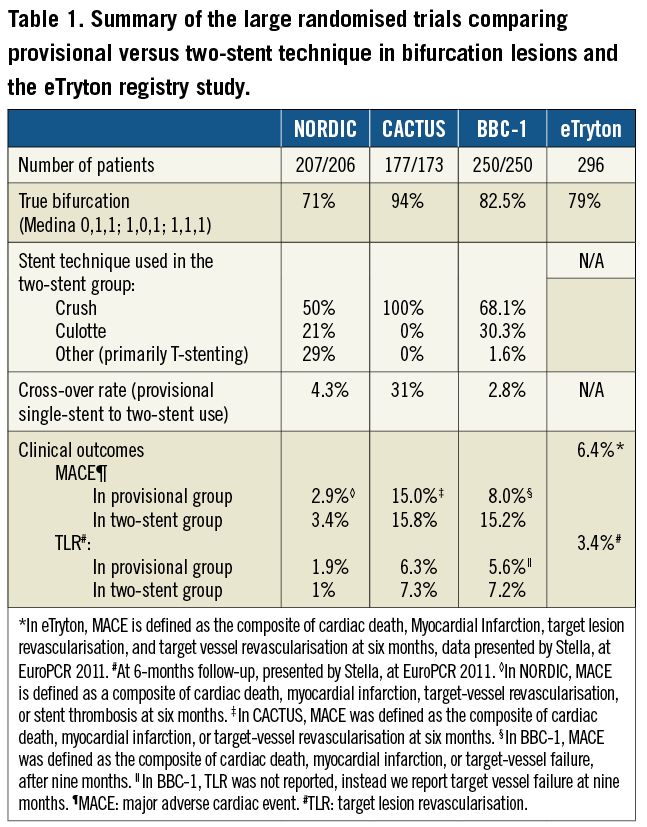
Nevertheless, there are some limitations concerning these trials which should be taken into account when interpreting these data:
– First, not all lesions in these trials were “true bifurcations” (i.e., Medina score 0,1,1; 1,0,1; or 1,1,1), with true bifurcation rates varying between 71% (Nordic) and 92% (CACTUS), resulting in randomisation of bifurcation lesions that had a high likelihood of having an acceptable result with a single stent (provisional) technique.
– Second, the rates of crush technique used in these trials are quite high (50% in Nordic up to 100% in CACTUS) resulting in a great number of stent struts at the level of the side branch, with a considerable number being non-apposed9. These non-apposed side branch (NASB) struts have delayed neointimal coverage, to the same degree as incompletely apposed stent struts6. Therefore, one should be cautious when generalising these trials for all two stent techniques.
– Third, double-stent techniques are more complex to perform than single-stent techniques, and therefore the success of two-stent techniques are highly operator dependent, with excellent results for the experienced, dedicated operators11, while others might achieve poorer results.
– Fourth, another important issue is the crossover rates from single- to two-stent strategies in these trials, which occurred in 2.8%8 up to 31%7,11, due to significant residual stenosis, closure or significant flow-limiting dissection in the SB. With a provisional single-stent approach, the available two stent bail-out techniques are restricted to either culotte or T-stenting. These techniques have limitations. In the case of T-stenting, there is an inherent risk of protrusion into the MB or gap/non-coverage at the side branch ostium. Culotte has the disadvantage of a double layer of drug-eluting stent (DES) struts in the proximal MB, which could increase the risk of (late and very late) stent thrombosis due to excessive drug deliver12.
In our opinion, it could be concluded that the current consensus of provisional stenting in bifurcation lesions is based on sub-optimally designed trials. We are not making a case against the use of provisional single-stent strategies in bifurcations, because in some types of bifurcations a provisional single-stent approach will be sufficient, especially in non-true bifurcations (i.e., lesions without side branch involvement) or very short ostial side branch lesions. However, in some cases a double stent approach should be seriously considered:
1) In complex, true bifurcations (i.e., Medina 1,1,1, Figure 1), especially when there is extensive side branch disease.
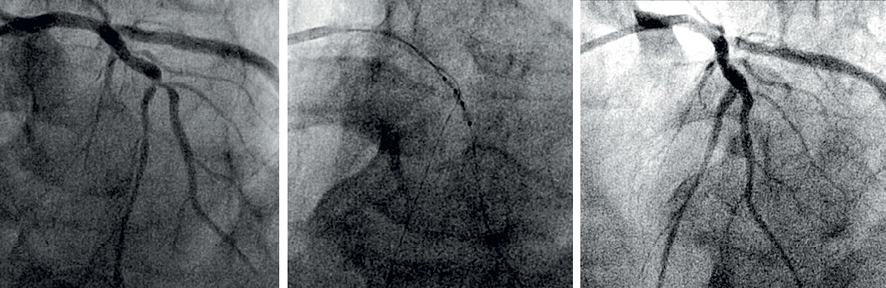
Figure 1. Treatment of a Medina 1,1,1 lesion with the Tryton stent. The left panel shows a significant stenosis of the LAD, proximal and distal of a large diagonal branch, with involvement of this branch (i.e., Medina 1,1,1). The middle panel shows positioning of the Tyrton Side Branch Stent. The right panel shows the final result after placement of a Tryton Side Branch Stent in the diagonal and a Xience Prime in the LAD.
2) In bifurcation lesions with a large side branch (>2.5 mm), as this indicates a large area of distribution, even in cases of non-true bifurcations, where the operator wants to ensure not losing the side branch (Figure 2).
3) If the operator foresees problems in re-crossing the stent struts into the side branch (depending on lesion angle, main branch stent type, etc.).
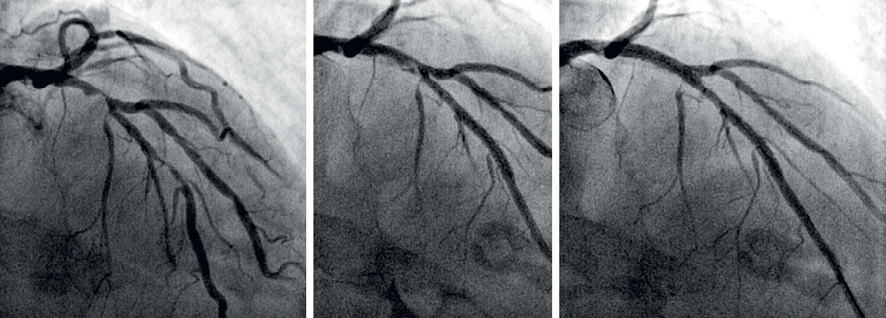
Figure 2. Treatment of a Medina 1,1,0 lesion with the Tryton stent. The left panel shows a significant stenosis of the proximal LAD, without involvement of the side branch (D1), but with some involvement distal to the side branch (i.e., Medina 1,1,0). The middle panel shows “snow-ploughing” after pre-dilatation of the LAD. The operator decided to protect the large diagonal side branch with the placement of a Tryton bifurcation stent. The right panel shows the final result after placement of a Xience Prime in the LAD.
Dedicated bifurcation devices
Regardless of the chosen strategy, bifurcation lesions still prove to have poorer results than non-bifurcation lesions. Therefore, different dedicated bifurcation devices are being developed with the potential of improving clinical outcomes after PCI of bifurcation lesions. These dedicated devices could be classified using the MADS classification. The MADS classification provides us with a simple, easy way to describe the different techniques used in bifurcation treatment (M stands for Main proximal branch first; A for main Across side first; D for Distal first; and S for Side branch first). Some of the newly developed devices provide easy access to the side branch, without the obligation to use a second stent, thus facilitating the provisional single stent approach. These stents are cla ssified according to the MADS classification as either “A” (the Nile Croco® and Nile Pax® devices of Minvasys, Gennevilliers, France) or as “M” (the Axxess™ self-expanding stent of Biosensors Int., Morges, Switzerland).
We will discuss here some of these dedicated devices, but limit ourselves to the devices which, rather than facilitating a two-stent approach mandate a two-stent approach, and could not be used as a bail-out strategy for provisional single-stenting. Most of these devices are classified as “S” in the MADS classification, mimicking culotte or T-stent techniques.
The Sideguard® stent (Cappella Medical Devices Ltd., Galway, Republic of Ireland) is a self-expanding trumpet shaped nitinol stent. Deployment of the stent is accomplished using a special balloon release sheath system. The device has five radiopaque markers that facilitate its visibility during and after the implantation using standard fluoroscopy: two distal and three proximal (the last also aids in accurate positioning of the Sideguard stent at the ostium). The stent consists of three zones:
1) the cup, which is designed to have complete wall apposition around the side branch ostium with minimum stress and shape deformation,
2) a transition zone, and
3) the anchor zone, which anchors the stent in the side branch distally.
The delivery system is composed of an exterior sheath, which retains the device and an interior tube, which supports the device eliminating device movement during deployment. Inflation of the system results in splitting of the exterior sheath. The delivery system also has a radiopaque marker band that facilitates placement of the stent at the side branch ostium. The device was studied clinically in a First-in-Man (FIM) study, the Sideguard-I (SG-1) study, presented at TCT 200713. Technical success was achieved in 16 (80%) patients. Target lesion revascularisation rate at six months follow-up was 12.5%, without cases of stent thrombosis. A second generation Sideguard was developed, with a mixed open and closed cell design with a new mid-distal open cell acting as a built-in anchoring system preventing the stent from migrating after deployment. The FIM study of this second generation Sideguard (SG-2) showed a technical success rate of 97%. Clinical results of the SG-1 and SG-2 combined showed MACE rates of 10.8% at 6-months14. An IVUS substudy of SG-1 showed an increase in SB stent area from 3.9±1.2 to 4.6±1.1 mm² (p=0.04) whereas no change in lumen area was observed (3.9±1.3 vs. 4.0±1.3 mm², p=0.77), suggesting that chronic stent expansion due to the self-expanding properties of the nitinol alloy compensates for the intimal hyperplasia within this bare metal stent15. More clinical studies as well as, eventually, a randomised trial, are needed to fully evaluate the performance of this device compared to a two-stent strategy with two conventional stents.
The other dedicated bifurcation device mandating a two-stent approach that we would like to discuss is the Tryton Side Branch Stent System™. The Tryton bifurcation stent is a side-branch first approach (S in MADS) and, in combination with a work-horse main-branch stent, it provides an alternative to the classical culotte technique16. What are the advantages of this device over classic culotte? The device is tapered, obeying Murray’s law17, and allows for better apposition in the proximal main branch. Due to the paucity of struts at the proximal portion and the carina itself re-crossing is much easier. At the same time, coverage and scaffolding of the side branch ostium is superior to provisional strategy. As demonstrated by OCT imaging, apposition at the carina is better, the number of overlapping struts is minimised and, most importantly, the number of struts in front of the side branch, which by definition are non-apposed, is decreased (Figure 3). Clinical results of a FIM trial of 30 patients16,18 and a two-centre registry19 were published previously. In the current issue of this journal, results are published of the eTryton registry, including 300 patients. All these publications consistently display TLR rates of 3-4% (at 6-9 months). Stent thrombosis rates at 6-9 months follow-up range from 0 to 0.3%. Currently, a large randomised trial in more than 700 patients is running where the Tryton Side Branch Stent, in combination with a regular DES in the main branch, is compared with a DES in the main branch with additional balloon angioplasty of the side branch. In this trial, only patients with a true bifurcation (i.e., Medina 0,1,1; 1,0,1; 1,1,1) are included as well as with a significant (>2.5 mm) side branch. This trial will get us closer to the answer concerning whether routinely a two-stent approach in true bifurcations with a dedicated device offers benefits over a single-stent approach. One limitation of this study is that patients with extensive side branch disease (>5 mm lesion length) are excluded, while this particular lesion characteristic could potentially benefit the most of a routine, multi-stent approach.
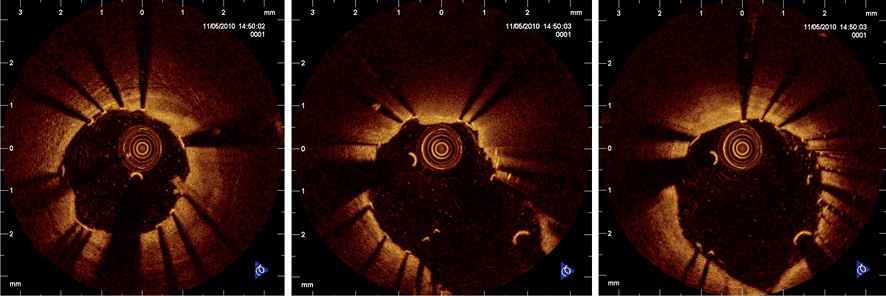
Figure 3. Optical coherence tomography after acute implantation of the Tryton Side Branch Stent at the level of the carina. Left panel: Strut apposition of Xience Prime everolimus eluting stent in the distal main vessel. Middle panel: Carina of the bifurcation of the left anterior descending (LAD) artery and the first diagonal branch (D1) showing a well-apposed stent struts and only some struts in front of side branch and minimal strut overlap. Right panel: Only a minimal number of overlapping struts and good apposition in the proximal main branch.
Although these results are very promising already, further improvements could be achieved by coating these dedicated side branch devices with a drug, so that the advantage of optimal ostial scaffolding of the side branch will not be neutralised by in-stent restenosis of these bare metal devices.
Conclusion
Caution should be taken in extrapolating results of previous large randomised trials comparing single- with two-stent techniques in bifurcation lesions to routine clinical practice. Current insights in bifurcation treatment, in particular regarding the importance of side branch involvement, does, in our opinion, not justify a routine provisional strategy in all bifurcation lesions. In true or complex bifurcation cases, a routine two-stent approach should be considered. New dedicated bifurcation devices show facilitation of the procedure and improvement of outcomes of the two-stent strategy.
Conflict of interest statement
P. Stella is member of the steering committee of the Tryton IDE trial. J. Wykrzykowska receives consultancy fees from Tryton Medical. M. Grundeken receives minor travel fees from Tryton Medical.

