Abstract
Although the guidelines recommend the provisional one-stent technique as a default technique for bifurcation coronary lesions, there are cases of bifurcations with large side branches (SB), difficult access and with ostial and diffuse disease extending more than 5 mm into the SB, where a two-stent strategy might be the best treatment option. Due to the inherent advantages and disadvantages of each two-stent technique, an appropriate technique should be selected according to each patient’s clinical condition, bifurcation morphology and the operator’s experience. Good long-term prognosis is most likely ensured by successful performance of each procedural step during the initial stenting.
Introduction
Consensus from the first 10 years of the European Bifurcation Club meetings recommended the provisional stenting technique as the preferred technique for bifurcation stenting1. This recommendation is based not only on multiple randomised trials and registries on the one-stent versus the two-stent technique in coronary bifurcation lesions but also on the practical approach of the KISSS principle (keep it simple, swift and safe). However, the consensus also stated that, in case of bifurcations with large side branches (SB) with ostial disease extending more than 5 mm from the carina, a two-stent strategy can be utilised. Nonetheless, dilemmas exist and controversies as to when complex bifurcation stenting should be used are most likely to persist. This paper, therefore, covers the potential indications for two-stent techniques in the drug-eluting stent (DES) era and the advantages and disadvantages of various two-stent techniques in this setting.
Current indications for a two-stent technique
A meta-analysis of previous randomised studies demonstrated that a provisional one-stent approach was comparable to a two-stent approach in terms of mortality, repeat revascularisation, and quality of life2,3. On the other hand, a one-stent technique was superior to a two-stent technique in terms of the risk of periprocedural myocardial infarction4-6. However, the two-stent approach in provisional or planned situations is still a viable option for a minority of patients who have complex true bifurcations. In such lesions, operators are afraid of acute complications, such as haemodynamic compromise, large periprocedural myocardial infarction, or patients’ subjective symptoms during the procedure. A two-stent approach is attempted for bifurcations where SB have large diameters (>2.5 mm), severe stenosis extending beyond the ostium (>10-20 mm), and/or an unfavourable angle for re-crossing after MB stenting7,8. A narrow angle between the MB and the SB may also be a potential predictor of SB compromise with increased risk of carina shift9.
In randomised studies comparing one- versus two-stent techniques, a two-stent technique was finally performed in around 4%-31%, even for patients assigned to a one-stent approach10-12. However, most of the available literature comparing one- versus two-stent techniques is burdened by a design dilemma. The populations in most of the published studies favour the provisional technique, because of inclusion of non-true bifurcations, and the inclusion of bifurcations with an SB diameter below 2.5 mm. Some of the more recently presented larger randomised studies might clarify the question in the near future. The recently presented randomised Nordic-Baltic IV trial (TCT 2013) showed a trend towards improved midterm outcome when using a two-stent technique compared to provisional stenting in bifurcations with large SBs (≥2.75 mm) having more than 50% diameter stenosis in the SB. This trend was similarly supported by the DKCRUSH-II trial and by a subgroup analysis of the Tryton IDE study (EuroPCR 2014). The EBC II trial on the provisional technique vs. the culotte two-stent technique in bifurcation lesions (SBs ≥2.50 mm and more than 50% SB diameter stenosis) may provide further information on the role of two-stent techniques in this subset of bifurcations. Until then, a two-stent technique may be considered “up-front” for bifurcations with large SB and with reference diameters ≥2.75 mm and significant disease extending into the SB7.
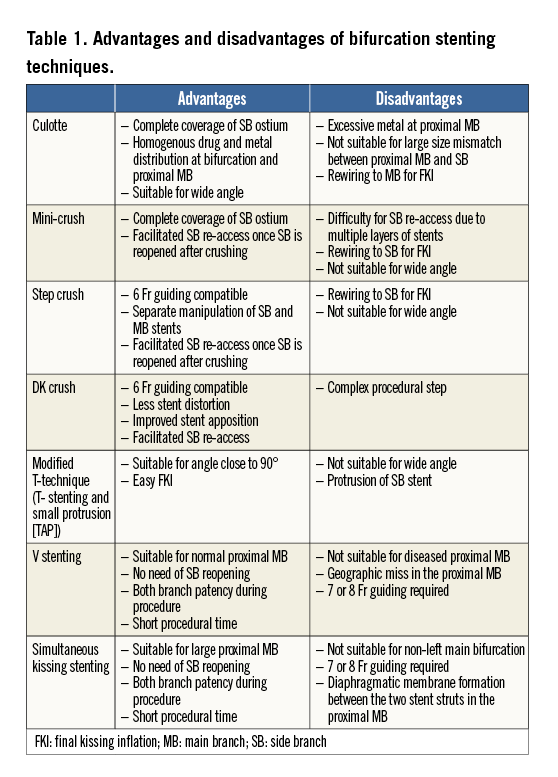
Advantages and disadvantages of various two-stent techniques
Current two-stent techniques using DES comprise the culotte technique, the crush technique, variants of the crush technique, the T technique, and the V or simultaneous kissing stent (SKS) technique. Classic crush is now not often performed, but variants of the crush technique, such as mini-crush, step crush, and DK (double kissing) crush techniques are preferred instead. The potential advantages and disadvantages are summarised in Table 1. Because of a lack of studies on the comparative outcomes of diverse two-stent techniques, selection of each bifurcation stenting technique should be dependent on the clinical manifestation, bifurcation morphology, and the operator’s preference13. A careful angiographic evaluation is required to identify disease severity, vessel size, and the angle of both branches. The technical details have been well described previously7,14.
Culotte stenting is a suitable approach when there is not a large discrepancy in vessel diameter between the MB and SB. Bifurcations with a wide angle between the MB and SB are an inviting target for culotte stenting. To avoid an excess of metal component, minimal overlap of MB and SB stent strut in the proximal MB segment is needed. If expansion of the MB during reopening is too large, the stent strut may be distorted or even ruptured.
The crush technique is the most widely used two-stent technique. In spite of complex procedural steps, this technique can be applied to any true bifurcations requiring a two-stent technique with complete lesion coverage for the ostial SB. Because of some limitations of the classic crush technique, its variants, such as mini-crush, step crush, or DK crush, are preferred15. The variants of crush techniques facilitate final kissing balloon inflation (FKI) with minimal protrusion of the SB stent or SB reopening before MB stenting. Using the step crush technique, in which the SB stent strut is crushed by the MB balloon instead of the stent, separate manipulation of two stents allows procedures using a 6 Fr guiding catheter and precise placement of each stent. In any crush technique, FKI should be performed for complete apposition of the SB stent16. In the randomised Nordic Bifurcation Stent Technique Study, the clinical outcomes were comparable between the culotte and crush technique groups over three years13.
The T-stenting technique is the most frequently used for provisional SB stenting during a one-stent approach to treat a suboptimal result or flow-limiting dissection in the SB. Therefore, the majority of T-stenting is performed with MB stenting first. When provisional stenting is attempted, the provisional T-stenting and small protrusion (TAP) technique was reported to improve outcomes17.
V or SKS can be used for bifurcations with a large proximal MB, such as left main stenosis. If there is no stenosis in the left main, stenosis in the ostia of both the left anterior descending artery and the circumflex artery can be treated with V stenting. SKS is currently not frequently performed due to relatively unfavourable angiographic and clinical outcomes18. Due to the formation of a thin diaphragmatic membrane between the two stent struts in the proximal MB, the risk of restenosis or stent thrombosis may be relatively high compared with other techniques. However, due to the benefits of fast procedural time and no need of strut reopening, SKS can be selectively performed for large left main bifurcation stenosis for patients with haemodynamically unstable presentation.
Due to the diversity in procedural techniques, it is not possible to prove the best stenting technique for the various types of bifurcation lesion. Instead, outcomes have been more dependent on whether each procedure is successfully performed or not. For instance, when an SB wire undermines the MB stent, FKI produces a gap between the SB stent and the vessel wall or results in failed crushing as shown in Figure 1. Such a complication is not infrequently encountered by non-experienced operators. Intravascular ultrasound guidance, the use of a non-compliant balloon, or the use of new-generation DES may also be associated with better clinical outcomes15,19. Therefore, what is important for good outcome is related more to the successful procedure than to the type of two-stent technique.
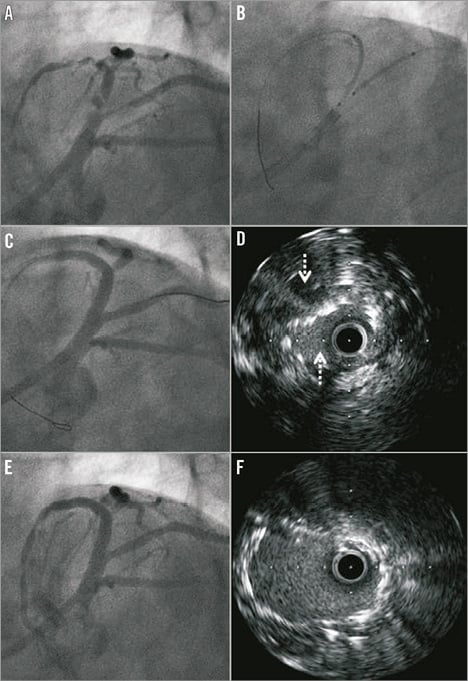
Figure 1. A case of mini-crush technique recognised by misplacement of side branch wire after crushing. Bifurcation stenosis (A) at the proximal left anterior descending artery (LAD) was treated by mini-crush technique (B) using three zotarolimus-eluting Resolute Integrity stents (Medtronic, Minneapolis, MN, USA) comprising a 3.0×38 mm stent in the middle LAD, a 3.5×30 mm in the proximal LAD, and a 3.0×18 mm in the diagonal branch. Diagonal wire misplacement was not recognised by angiography after crushing and final kissing inflation (FKI) was performed (C). Because the diagonal wire undermined the LAD stent in the proximal segment, intravascular ultrasound (IVUS) images showed the barrel shape of two stents (arrows) in the pullback images from the diagonal branch (D). After wire repositioning and repeated FKI, angiography (E) and IVUS (F) showed successful results.
Conclusion
In spite of the consensus that the one-stent technique should be the default strategy for bifurcation coronary lesions, the two-stent technique is still performed in selected patients having significant diffuse SB stenosis. Due to the inherent advantages and disadvantages of each two-stent technique, an appropriate technique should be selected according to each patient’s clinical condition, bifurcation morphology and the operator’s experience. Good prognosis is mostly ensured by successful performance of each procedural step, i.e., FKI with appropriately sized balloons should be used properly during all two-stent techniques. The best two-stent technique might, in most circumstances, be the one with which the individual operator is most familiar and experienced, since the individual long-term result might be more operator-dependent than technique-dependent.
Conflict of interest statement
The authors have no conflicts of interest to declare.

