Introduction
In this chapter of Tools and Techniques the percutaneous treatment of bifurcations lesions is discussed using a step-wise approach. The following is an overview of its management with highlights on specific technical issues. The complete, unabridged e-version with images is available at www.eurointervention.org.
The presence of low wall shear stress areas in both branches of a coronary bifurcation, opposite the carina, account for the frequency of coronary bifurcation lesions1 encountered in daily practice. While interventional cardiologists have attempted to treat these lesions since the early days of balloon angioplasty, the technical strategies that should be implemented are still the subject of substantial debate. We aim to describe in detail the strategy of provisional side branch (SB) stenting which has become the gold standard technique in the vast majority of coronary bifurcations.
Background
The coronary tree is an object of fractal geometry. It branches off into assymetrical bifurcations according to Murray’s law which defines the diameter relationship between the main vessel and the two distal branches2. This law may be simply expressed by Finet’s formula3 as follows: main proximal diameter = (main distal diameter + SB diameter) X 0,678. Therefore, the main vessel has two different diameters, and this must be taken into account in order to achieve an optimal result.
The Medina classification (Figure 1) serves as a description tool for bifurcation lesions. It indicates the location of significant stenosis (>50%) in the coronary bifurcation. It cannot be used to describe the angles, the calcifications and the length of the lesions.
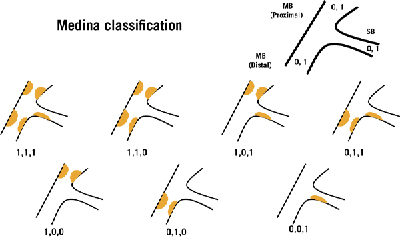
Figure 1. Medina classification of bifurcation lesions: before the first coma, 1 or 0 depending on the presence or not of > 50% stenosis in the proximal main vessel, between the two comas the same for distal main vessel, after the second coma the same for side branch (from A.Medina).
Among numerous treatment techniques summarised in the MADS classification (Figure 2), Provisional SB stenting is the gold standard strategy for non-left main bifurcation treatment4. Indeed, six of seven randomised trials comparing this strategy with dual-stent techniques have shown that the implantation of two stents is not associated with any benefits, regardless of the lesion type.
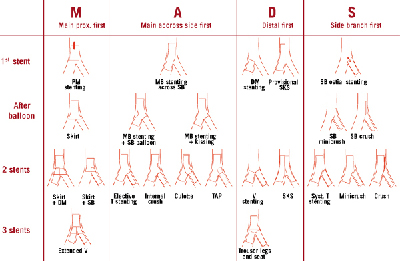
Figure 2. MADS classification of techniques (straight techniques).
Stenting a coronary bifurcation step-by-step (Figures 3 and 4)
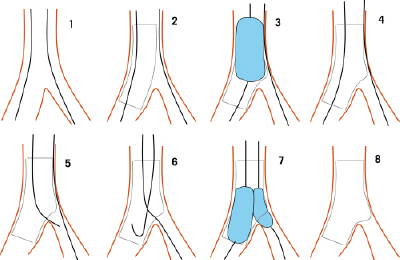
Figure 3. Schematic drawing of each step of the provisional approach: 1. Both branches wired starting with the most difficult one. 2.Main branch stenting (stent sized according to MB distal reference). 3. Proximal optimisation technique (POT). 4. Stent apposition, SB partial scaffolding. 5. Main branch wire through the most distal strut. 6. Jailed wire removed and pushed in distal MB with a loop. 7. Kissing balloon inflation. 8. Final result (if not satisfactory, T stenting, TAP, inverted crush or culotte stenting can be performed).
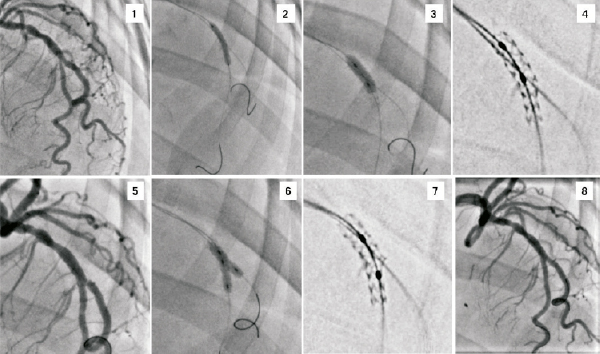
Figure 4. Typical provisional SB stenting strategy. 1. LAD2, LAD3, Dg2; 0,1,0 bifurcation lesion. 2. Direct stenting from PM to DM with a jailed protective wire in the SB, diameter chosen from DM diameter. 3. POT technique with a short balloon on PM, diameter chosen from the PM diameter. 4. “Stentboost” showing the stent with its two diameters. 5. Angiographic results showing a residual stenosis on SB ostium. 6.Kissing balloon inflation with non-compliant short balloons, diameter chosen from DM and SB diameters. 7. “Stentboost” showing the typical aspect after KB, a SB T stenting is possible without gap. 8. Final angiographic result with one stent.
1. Insertion of a wire into each distal branch starting with the most difficult branch in order to avoid wire wrap. Systematic placement of a wire in the SB helps to open the access angle, to keep the SB patent, and serves as a marker in cases of closure. A long shape on the main branch (MB) wire facilitates SB re-wiring during wire exchange after MB stenting.
2. The main vessel may or may not be predilated. It is preferable not to predilate the SB in order to avoid re-crossing both the stent struts and a dissected SB segment after MB stenting. In addition, the absence of SB pre-dilation results in the recrossing access towards the SB being restricted to the stent strut closest to the carina, which allows better metal protrusion into the SB.
3. Stenting of the MB: The diameter of the MB stent implanted across the SB should be selected according to the distal MB diameter in order to decrease the risk of carena shifting. Selection of the MB stent length is also very important in order to leave enough space proximal to the bifurcation to post dilate the proximal part of the MB stent (POT) which is under-deployed.
4. The POT technique (proximal optimisation) is useful in the presence of a large SB diameter. It allows the operator to match the proximal segment of the MB stent with the MB diameter by means of a short balloon with a diameter adapted to the proximal segment.
5. Guidewire exchange is not required in cases where the SB is small and the patient is asymptomatic with normal EKG and normal flow after MB stenting. In other instances, it is performed to allow kissing balloon (KB) inflation which reduces the rate of SB re-stenosis, although its clinical validity has been questioned. The wire positioned in the stented vessel is removed with its tip pointing towards the SB, and subsequently inserted into the SB through the distal cell using a long angulated distal tip.
Then the jailed wire is withdrawn carefully in order to avoid abrupt guiding catheter intubation, and subsequently advanced into the distal MB (a short angulated shape helps to recross the MB stent with a loop).
6. KB inflation is carried out with two short balloons, preferably non-compliant, with a diameter compatible with both distal branches. Although it is preferable to avoid simultaneous inflation, simultaneous deflation is recommended.
7. Further to KB inflation, the decision must be made as to whether the SB should be stented or not.
For SB stenting: chest pain, EKG changes, <3 TIMI flow, unstable dissection, severe residual stenosis, large SB.
Contra SB stenting: short SB stenosis (usually not significant when using functional evaluation by FFR)5. As SB stenting increases the late loss even when DES are used, it should not be performed when a good result has been achieved after balloon inflation.
8. Which dual-stenting technique should be used? Dual-stenting procedures may be carried out using T stenting, TAP (T and protrusion), internal crush or culotte (not adapted to open angles). Final KB inflation is mandatory after dual stenting.
Conclusion
The provisional SB stenting strategy has been associated with many tips and tricks.
However, it can be implemented quite easily provided each phase of the procedure is carried out appropriately.
Acknowledgement
The authors would like to thank Mrs. Catherine Dupic for her assistance in the preparation of this manuscript.
Conflict of interest statement
T. Lefèvre has received minor fees from Abbott, Boston Scientific, Terumo, Biosensors and Cordis. Y. Louvard has no conflict of interest to declare.