Abstract
Provisional side branch (SB) stenting is the recommended treatment strategy in the vast majority of bifurcation lesions. Over the past 10 years, advances in fundamental knowledge have led to a better understanding and to improvements of this technical approach. This strategy has reached maturity, and long-term clinical results are now comparable to those of non-bifurcation lesions. This paper describes in detail simple rules and tips and tricks which may help physicians in daily practice to use provisional side branch (SB) stenting as the gold standard treatment for the majority of bifurcation lesions.
Background
Bifurcation lesion treatment remains technically challenging (Moving image 1). Despite the introduction of drug-eluting stents (DES) which have allowed a significant reduction in the risk of restenosis and repeat interventions1,2, the use of complex techniques with DES has not solved the problem of SB restenosis. Randomised studies have shown that the implementation of complex techniques with two stents does not improve the efficacy and safety of SB treatment3,4. A two-stent approach may be required as a primary option in the most complex bifurcation lesions, in rare instances of difficult SB access, or in long SB lesions5. Therefore, provisional SB stenting is the recommended approach in the vast majority of bifurcation lesions6,7.
The three diameters
A knowledge of the fundamental aspects of bifurcations is essential to understand fully the technical approach used for the provisional SB stenting strategy.
Ramifications of the coronary tree follow the natural law of minimum energy cost in providing the underlying myocardium with the amount of blood required8. As a consequence, there are three segments in a bifurcation, each of which has its own diameter. There is a constant relation between these three segments governed by Murray’s law9,10, which was simplified by Finet11. The proximal main branch (MB) is consequently larger than the distal MB (Figure 1).
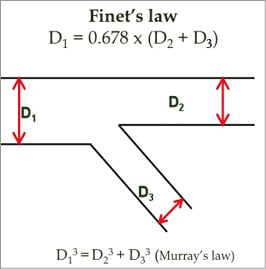
Figure 1. The branching law of bifurcation.
Technical aspects
Provisional SB stenting is an A technique (A for across the side branch) according to the MADS (Main, Across, Distal, Side) classification adopted by the European Bifurcation Club (EBC) in 200712. More than a technique, it is a philosophy of treatment, designed to meet the main objectives of bifurcation lesion treatment, focusing on the MB whilst ensuring patency of the SB. With this approach, a single stent can be used in 80 to 90% of cases with excellent clinical outcome13.
ONE OR TWO WIRES?
The systematic wiring of the two distal branches at the beginning of the procedure provides several advantages. It is a good marker of the SB origin in the event of SB occlusion14. It can also be used to re-open the SB by pushing a small balloon between the stent and the wall of the vessel, as described by Burzotta15. Furthermore, the SB wire modifies favourably the angle between the MB and SB which may facilitate wire exchange as well as balloon and stent advancement if necessary. Moreover, in the TULIP multicentre study16, use of only one wire when starting the procedure was a predictor of SB treatment failure and repeat intervention at six months.
It is very important to shape the distal tip of the MB wire in order subsequently to re-cross the distal strut of the MB stent by means of a gentle pullback technique. The wire tip should be modified manually in accordance with the angle between MB and SB and the MB. To avoid wire wrap it is recommended that the most difficult lesion should be wired first.
PREDILATATION
Predilatation of the MB is left to the discretion of the operator according to the type of lesion (Moving image 2). Kissing balloon predilatation is not recommended because of the risk of extensive dissection on a “non-stented” vessel.
Predilatation of the SB remains a subject of controversy. Our opinion is that it is preferable not to predilate the SB because the occurrence of dissection inherent in the enlargement of the SB lumen may increase the likelihood that access to the SB may also be possible through a proximal strut or through the dissection, leading to a suboptimal result after kissing balloon inflation (KBI). This is based on the fact that access through a distal strut is the only possibility for projecting struts in the SB ostium.
We recommend that SB predilatation should be performed when SB access is difficult or in cases of severe and calcified SB lesions. When SB predilatation is carried out, it is very important to use non-compliant (NC) balloons and carefully assess the angiographic result before MB stenting, and be ready to switch to another strategy (crush technique, culotte or T-stenting) in case of SB dissection.
MAIN BRANCH STENTING
The stent platform selection is very important for bifurcation lesion treatment. Due to the differences in platform design, maximal stent expansion and strut opening capacity may vary among the currently available workhorse stents17. The assessment of stents in bench tests or computer simulation has been essential in improving the comprehension of bifurcation stenting18-20.
Stent selection should be made according to the maximal expansion ability of the stent, in order to allow stent apposition both on the MB wall and the SB ostium (Moving image 3). The maximal opening diameter of the MV at the SB ostium is also an important criterion for large bifurcations such as the left main, and we recommend that stents with an open-cell design should be used rather than stents with closed cells17.
The choice of stent diameter for MB stenting is also crucial (Moving image 4). If the stent diameter is selected according to the proximal MB reference diameter, it may increase the risk of SB occlusion by carina shifting. Therefore, the stent diameter should be selected according to the distal MB reference (Figure 2). The drawback is the inadequate proximal MB stent apposition which can be easily corrected by the proximal optimisation technique (POT) and/or KBI.
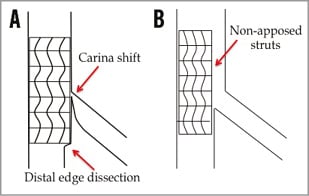
Figure 2. Importance of main branch stent diameter for bifurcation lesion treatment. A) Diameter according to proximal MV segment. B) Diameter according to distal MV segment.
PROXIMAL OPTIMISATION TECHNIQUE
We initially described POT at the EBC meeting in 2008 in order to correct the proximal MB stent malapposition observed when selecting a stent according to the distal MB diameter (Moving image 4). By simply using POT, workhorse stents can be adapted to the fractal anatomy of bifurcation lesions, especially in bifurcation lesions with a large SB where there is a greater difference between the proximal and distal MB diameters.
POT is carried out by inflating a short NC balloon with two markers in the MB stent proximal to the carina. The balloon size should be selected according to the proximal MB reference. When the proximal MB is diseased, the reference can be easily calculated by using the Finet formula or the Huo chart11,21. Balloon positioning is crucial and may influence the final result. The distal balloon marker should be positioned in front of the carina whilst the proximal part is still in the stent in order to avoid geographical miss (Figure 3). Inflation is performed at a pressure giving the appropriate diameter. As a result, the original anatomical configuration of the bifurcation is restored (Figure 3).
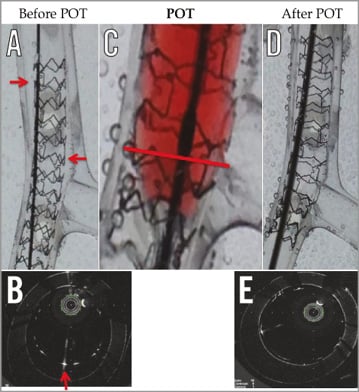
Figure 3. Main branch stent on a silicone fractal bench into water bath. Non-apposed in the proximal MB (red arrow in A and B with OFDI). Positioning of the POT balloon in C, with distal part of the distal marker in front of the carina (red line). Final result in D and E, after POT, with apposed strut and cell enlargement in the proximal segment.
Bench testing, computer simulations and in vivo application have shown other potential benefits of POT. POT induces a constant increase in cell size area and modifies the orientation of the SB ostium. This facilitates access towards the SB and the distal stent crossing close to the carina by reducing the number of possibilities to cross through the MB stent (Figure 4). As a consequence, POT is particularly helpful in instances of strut wire re-crossing failure, and also facilitates the balloon crossing. By apposing the stent strut to the proximal MV wall, POT prevents the wire from crossing into the SB between the arterial wall and the stent, which would result in crushing the MV stent with the SB balloon inflation (Figure 3 and Figure 4).
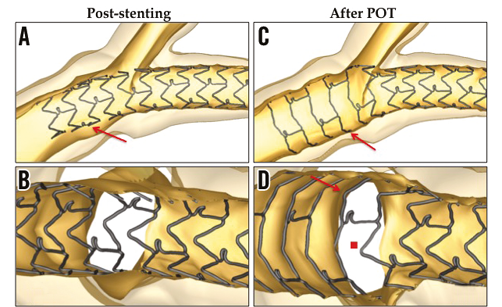
Figure 4. Computer simulation of left main stenting (P. Mortier) showing proximal non-apposed struts in A (red arrow) and ostial SB strut obstruction in B after MB stenting, and role of POT on apposition and cell enlargement (red arrow) in C and D, facilitating distal strut re-crossing (red point).
The drawback of POT is the stent crown overstretching, different among various DES20, which may induce variable gaps between struts, and could impair the vessel wall scaffolding and drug elution. This is why the choice of the platform is very important.
KISSING BALLOON INFLATION
Even though a randomised study showed no clinical evidence22 supporting the systematic use of KBI, it has been shown to improve the acute angiographic and physiological result in the SB22,23 and reduces the angiographic SB restenosis rate and inducible ischaemia at follow-up22,24. Several steps are necessary to carry out KBI appropriately.
REWIRING THE SB AND WIRE EXCHANGE
Both in vitro bench tests18,25 and in vivo OCT imaging26 have shown that wiring the MB stent through the cell closer to the carina provides better ostial SB scaffolding than entering the proximal strut after KBI. To increase the chance of a “distal re-cross”, POT and pullback wiring technique with the appropriately pre-shaped MB wire are advised (Moving image 5). When the tip of the wire is engaged within the stent strut, careful steering allows crossing into the SB. In case of difficulty in advancing the wire into the SB, a repeat POT, wire reshaping, the use of a hydrophilic polymer-coated or a stiffer wire with improved torque, or even a microcatheter may help to overcome the technical issues27.
After SB wire crossing, the SB jailed wire is withdrawn (right hand) proximal to the stent while the guiding catheter is closely controlled (left hand) in order to avoid deep intubation, which might cause proximal dissection or longitudinal stent compression.
Once released, the previously SB jailed wire is advanced into the MB, possibly with a loop to avoid potential advancement outside the stent.
BALLOON TYPE AND DIAMETER (Moving image 6)
Balloon selection is also very important. The diameter must match that of the two distal branches. The MB balloon must be sufficiently short (or the stent long enough) to avoid inflation proximal to the MB stent, and the SB balloon should be short in order to avoid damaging the SB. In cases where POT has not been performed, KBI may optimise the proximal segment of the MB.
The use of NC balloons for KBI allows improved stent expansion in the MB whilst reducing the risk of dissection in the SB28. This decreases the need for SB stenting.
In case of difficulty in SB balloon crossing, a new POT may be helpful. The other options are to use a smaller semi-compliant balloon, and as a last resort to try to re-cross through a different strut. Anchoring balloon technique using the stented MB distal to the carina can also be useful.
SEQUENCE AND DURATION OF INFLATION
The aim of KBI is to create some ostial scaffolding with the MB stent and correct the proximal MB stent malapposition. The appropriate sequence of inflation to achieve these results and minimise the proximal MB stent deformation is currently a subject of discussion. The benefit of sequential inflation, in improving ostial scaffolding and stent expansion, was initially described by Kinoshita (EBC 2009). Mickley and Larson (EBC 2013) have also shown that sequences and number of inflations may influence SB opening and ostial SB scaffolding (Figure 5). Mortier recently proposed a sequential inflation beginning with the SB29. After POT and rewiring, it consists of inflating the SB at 12 atm first, then the MB at 12 atm while deflating the SB at 4 atm. This reduces the final elliptical deformation and optimises SB access compared to simultaneous KBI. Based on these results, a two-step inflation, beginning with the SB, is recommended.
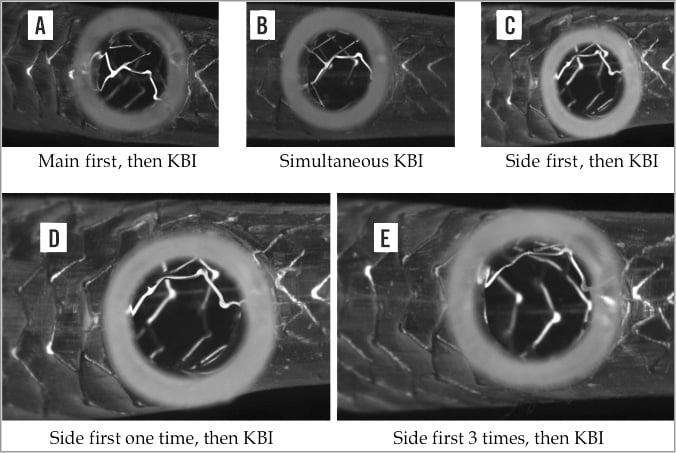
Figure 5. Silicone fractal bench focusing on the ostial side branch after KBI. Differences in side branch opening and scaffolding depending on the sequence of KBI in A, B and C, for the same stent and same strut re-crossing. Difference also depending on time duration in D and E.
The elliptical deformation, which has been associated with a greater amount of thrombus in an OCT study30, can also be corrected after KBI by a final POT as described by Foin31.
Concerning the deflation time, bench tests suggest that both balloons should be deflated simultaneously18,25.
A recent study has also demonstrated that prolonged inflation duration to 60 s results in better stent expansion32. Therefore, three inflations of 20 s may be recommended.
When and how to treat the side branch?
Stenting of the SB is clearly indicated in instances of major SB dissections or compromised SB flow after KBI7. The problem of residual stenosis is still a subject of controversy, because angiographic assessment of the SB ostium is not easy. The degree of SB angiographic stenosis is overestimated as assessed by FFR33. Therefore, we should not overtreat the SB with stents, and FFR could be helpful in this setting, but this also depends on the SB lesion length and size.
The advantage of the provisional strategy is that any technique can be applied after MB stenting and SB opening: T-stenting, TAP or culotte. The choice is left to the operator, but technique selection will depend mainly on the bifurcation angulation. Of course final KBI using NC balloons is always recommended after any two-stent technique.
Conclusion
Provisional SB stenting is the recommended treatment strategy in the vast majority of bifurcation lesions. Over the past 10 years, advances in fundamental knowledge have led to a better understanding and to improvements of this technical approach (Moving image 7). This strategy has reached maturity, and long-term clinical results are now comparable to those of non-bifurcation lesions.
Conflict of interest statement
O. Darremont is an advisory board member for Abbott Vascular. T. Lefèvre is an advisory board member for Abbott Vascular and Boston Scientific and has received minor fees from Terumo, Asahi and Biosensors. R. Albiero has received minor fees from Abbott Vascular. The other authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Baseline angiography of Medina 1,1,1 LAD/diagonal bifurcation lesion.
Moving image 2. MB predilatation with 3.0×15 mm NC balloon.
Moving image 3. MB stenting with a 3.0×18 mm DES.
Moving image 4. POT with 3.5×8 mm NC balloon.
Moving image 5. Re-crossing distal strut by pullback technique of the MB wire.
Moving image 6. KBI with 3.0×15 mm NC balloon in the MB and 2.5×15 mm NC balloon in the SB.
Moving image 7. Final result.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Baseline angiography of Medina 1,1,1 LAD/diagonal bifurcation lesion.
Moving image 2. MB predilatation with 3.0×15 mm NC balloon.
Moving image 3. MB stenting with a 3.0×18 mm DES.
Moving image 4. POT with 3.5×8 mm NC balloon.
Moving image 5. Re-crossing distal strut by pullback technique of the MB wire.
Moving image 6. KBI with 3.0×15 mm NC balloon in the MB and 2.5×15 mm NC balloon in the SB.
Moving image 7. Final result.

