Optimal treatment of coronary bifurcation lesions by percutaneous coronary intervention (PCI) has been investigated and debated intensely. In this issue of EuroIntervention, Milasinovic et al provide an easy to follow step-by-step manual for bifurcation stenting by the provisional side branch (SB) stenting technique, with careful remarks on selection of two-stent techniques for appropriate cases1. The strategies follow the European Bifurcation Club (EBC) consensus and focus on feasibility and keeping resource utilisation to a minimum.
Also in this issue, in an effort to make bifurcation stenting even easier, Tang and colleagues present the first preclinical results with a prototype of the prewire channel stent (APT Medical Inc., Xiangxian, China)2.
This dedicated bifurcation stent allows preloading of the SB wire through stent cells that the operator expects to align in front of the side branch ostium. Therefore, when subsequently implanted, the stent is already rewired and there is no need for wire exchange. In theory, and in the presented series of implantations in pigs, the stent was easily delivered and had apparently rotated so that the cell for recrossing was in front of the SB ostium, although this was not confirmed. The flexible stent design with multiple wire crossing points is an advantage over other dedicated bifurcation stents for main vessel implantation with a fixed position of the opening to the SB. However, the need for the stent to rotate into position and the need to ensure that the SB wire cell is located just proximal to the carina are major limitations, and inability to position in diseased bifurcations may not be detected in the coronary arteries of healthy pigs. In the often highly irregular lumen of an atherosclerotic and maybe even tortuous coronary artery, rotation of the stent just in front of the SB ostium based on tracking by the SB wire may be very difficult. Therefore, before first-in-man implantations, it would be advisable to evaluate the deliverability either in pigs with extensive atherosclerosis or in coronary bifurcation phantoms with lumen resembling coronary atherosclerosis of varying extents.
The importance of appropriate bifurcation phantoms and a standardised set-up for evaluation of stents and implantation techniques is emphasised in the EBC consensus document by Ormiston and colleagues on “bench testing and bifurcations”3, also featured in this issue.
From simple bifurcated silicone tubes to future 3D bio printing of coronary arteries with human-like tissue maintained in bioreactor perfusion systems, the authors indicate the pros and cons, and provide key specifications to follow during design. Development of human-like coronary phantoms is urgent. The high costs and low access to atherosclerotic pigs makes it important for both independent researchers and companies to have a preclinical testing platform that is as close to the human coronaries as possible. Stents or stent techniques that perform acceptably in regular tubes could show disproportional weakness in irregular lumen models with human-like elasticity. Evaluation of the mechanical properties of bioresorbable scaffolds and the feasibility of various two-stent techniques may be such examples. Low-cost human-like transparent phantoms would facilitate training and direct evaluation of stent techniques, e.g., by OCT, thereby making such capacity available to sites with fellows in training and to groups with an interest in improving their bifurcation implantation techniques and for “entry-level” research.
Use of phantoms in modelling and computation of flow and shear stress are important applications covered by the document. Validation and comparison of the wide spectrum of computation methods in standardised, well characterised phantoms are obvious tasks to come, but present best-in-class methodology may already provide crucial information on influence of anatomy, pathoanatomy, stent design and implantation techniques on local flow disturbance and shear stress patterns. As there are no standardised specifications from the FDA and ISO on testing and measurement specific to bifurcations, the consensus paper suggests relevant tests and endpoints. Description of local flow patterns around apposed and jailing struts may be added as future requirements in such evaluations.
Optimal position of the wire recrossing into the SB has been the focus of numerous bench studies and registries. Okamura et al confirm that distal cell rewiring is of importance to reduce incomplete stent apposition (ISA) in the bifurcation core segment4.
The novel information relevant for operators is that the negative consequence of proximal rewiring is more pronounced with narrow angle “parallel” bifurcations than with larger angle “perpendicular” bifurcations. As the SB ostium is oval-shaped and longer in narrow angle bifurcations, a proximal rewiring position and subsequent kissing balloon dilatation may push more struts in front of the ostium towards the main vessel lumen compared to bifurcations with larger angles. If the dilatation after proximal rewiring is performed as kissing with exact simultaneous deflation of the balloons, the struts may be positioned in the middle of the lumen and, if only an SB balloon is inflated, the struts could be pushed to the side opposite the SB ostium, effectively jailing the distal MV. In perpendicular angle bifurcations, the SB balloon may more often be in an almost coaxial position to the SB. The MV stent struts are then to a higher degree pushed towards the edges of the ostium and may therefore be less dependent on the wire position.
Both in this work and in the step-by-step manual by Milasinovic on bifurcation stenting, a clear description of how final POT was or should be performed would have been helpful. The position of the balloon during final POT may be of the utmost importance so that the bifurcation anatomy ensured by kissing balloon inflation is not distorted. If the wire position is not confirmed by OCT, an unintended proximal rewiring results in a long metallic carina that is subsequently pushed towards the SB if the final POT balloon is positioned distal to the proximal offspring of the bifurcation (Figure 1). Thus, the struts forming the metal carina are again jailing the side branch ostium and there is a risk of some compression of the SB ostium. Particularly in two-stent techniques, this may be detrimental.
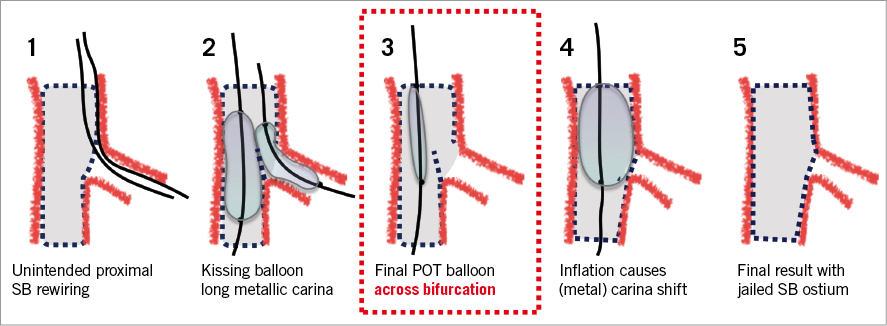
Figure 1. Pitfall in final POT. Bifurcation anatomy is ensured by kissing balloon inflation with simultaneous balloon deflation. A subsequent final POT with the balloon in a distal position across the side branch shifts the (metal) carina towards the side branch ostium.
Okamura et al observed that 3D OCT guidance was more successful (non-randomised) in achieving distal rewiring compared to 2D OCT4. 3D OCT requires suitable equipment, correct settings, optimal vessel clearing and more interaction with the OCT apparatus to enable adequate visualisation of both stent struts and guidewires and in an optimal viewing angle. Evaluation of wire positions by 2D OCT is less fancy but only requires identifying the cell for wire passing and following the cell distally to see if it extends to the carina. It would be interesting to see if 10 minutes of training in 2D OCT evaluation of wire positions would lead to the same diagnostic accuracy as with 3D OCT but at higher feasibility and with shorter analysis time. However, even more importantly, is it possible to ensure distal rewiring by an optimal rewiring technique and angiographic evaluation aided by stent enhancement such as StentBoost (Philips, Amsterdam, the Netherlands) or CLEARstent (Siemens Healthineers, Erlangen, Germany)?
With the evidence and guideline recommendations supporting invasive imaging for guiding left main stenting, which in 80-85% of cases involves the bifurcation, the high angiographic ambiguity in complex bifurcation stenting and growing body of evidence that adequate stent expansion is required and that optimal rewiring is essential for ostial scaffolding, reduction of ISA and to avoid accidental abluminal rewiring, the minimal strategy described by Milasinovic and colleagues may require some future adaptations. The addition of mandatory invasive imaging in complex bifurcation stenting may be a guideline requirement if, e.g., the upcoming ILUMIEN IV trial and the ongoing OCTOBER trial (NCT03171311) show a clinical benefit of routine OCT guiding. For now, the described angiography-based strategies in non-left main bifurcations remain the present standard of care in bifurcation stenting.
Conflict of interest statement
N.R. Holm received institutional research grants from Abbott, Biotronik, Reva Medical, Boston Scientific and speaker’s fees from Abbott, Reva Medical and Terumo. L.N. Andreasen received an institutional research grant from Abbott. E.H. Christiansen received institutional research grants from Abbott and Biotronik, and speaker’s fees from Abbott.