The use of fractional flow reserve (FFR) to determine the physiological severity of coronary stenosis is well established and is routine practice for main vessel coronary artery stenosis. Percutaneous coronary intervention (PCI) that requires stent deployment across a side branch (SB) can result in deleterious distortion of bifurcation anatomy, even in SBs that were angiographically normal prior to PCI. This may result in the creation of a significant stenosis or occlusion of the SB, primarily due to carina shift from the main vessel (MV) into the SB.
In the current issue of EuroIntervention, Omori et al report the use of a deflated semi-compliant balloon extending from the left anterior descending (LAD) artery into a large SB over a coronary pressure wire and subsequent stent deployment in the LAD1.
The jailed balloon technique was demonstrated to secure the lumen of the jailed SB with pressure wire Pd/Pa measurements changing from 0.34 immediately after stent deployment to 0.60 after balloon removal from the SB. Consequently, following re-crossing and kissing balloon inflation, the FFR in the SB was 0.84. This novel jailed balloon technique with pressure wire might have two advantages: 1) to secure the lumen of the jailed SB; 2) to provide a means for haemodynamic assessment of the SB to assist decision making regarding whether SB intervention is necessary.
This technique should be reserved for vessels where there is high risk of SB occlusion after MV stenting, which can be assessed by plaque burden, SB take-off angle, SB ostium involvement, etc. In addition, it remains unclear whether pressure wire-directed SB PCI yields improved clinical outcomes compared to angiography-alone directed SB PCI2. The possible disadvantages of this technique include: 1) distortion of the MV stent when removing the jailed balloon; 2) decoiling of the pressure wire on removal from the jailed segment of the vessel; 3) pressure wire, in particular the pressure transducer segment, being caught in the MV stent struts on removal3.
For general adoption of this novel technique more data are required to elucidate these issues but, if proven to be efficacious, it has the potential to impact significantly on the treatment of high-risk SB vessels.
Regardless of provisional or systematic double-stent strategy, in cases requiring SB interventions after main branch stenting, kissing balloon inflation (KBI) is widely performed in daily practice. KBI has two main purposes: 1) expanding the SB ostium adequately, 2) correcting the carina position (ideally the middle of the MB and SB). In order to perform KBI effectively and safely, the use of appropriately sized non-compliant balloons for both branches is recommended4, avoiding unexpected balloon underexpansion or overexpansion, which may result in suboptimal KBI results (inadequate SB ostium expansion, coronary dissection, etc.). Although the efficacy of KBI has been reported5, there are concerns regarding ellipsoid stent deformation and mother vessel (MoV) overexpansion. In this regard, especially for cases with less vessel size discrepancy between proximal and distal to the bifurcation, KBI with slightly undersized balloons, modified KBI (SB dilatation, followed by KBI with low pressure in the SB), or mini-KBI (minimal protrusion of SB balloon towards the MoV) could be considered6,7.
In order to overcome these limitations of KBI, Al-Saadon et al reported the efficacy of a dedicated bifurcation balloon (DBB) tested in a swine coronary bifurcation in comparison with conventional KBI.
The DBB is a unique device comprising three components of differently sized balloons (MoV: 3.5 mm, MB: 3.0 mm, and SB: 2.5 mm), which seems theoretically reasonable to prevent the concerns regarding conventional KBI (Figure 1)8. However, unfortunately the study was conducted in only one bifurcation lesion for each technique without any quantitative evaluations (visual evaluation alone) and, for its utilisation in real-world patients, the deliverability of the DBB could be a main concern. During bifurcation PCI, we frequently encounter difficulties in delivering the balloon towards a jailed SB due to the presence of MB stent struts, disease at the proximal SB, or the SB angulation. From this point of view, the friction during DBB delivery may be much higher, not only because of the larger profile of the DBB but also becaue of the fact that the operator has to advance two balloons towards the MB and SB simultaneously. Moreover, this limitation may also result in unfavourable positions of each balloon. Furthermore, considering the difficulty of adequately visualising the bifurcation by 2D angiography, geographic miss of this complex shaped DBB should also be taken into account. Therefore, the development of a marker on the catheter indicating the position of balloons to be placed at each branch ostium is required. In order to introduce this unique device into clinical practice, an improved device profile and assessment in various types of bifurcation lesion with different sizes and angles are required.
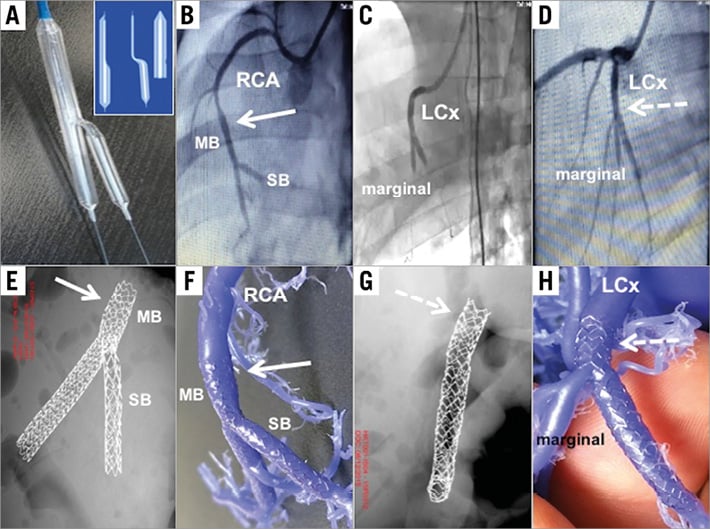
Figure 1. Comparison of bifurcation stenting results: DBB vs. standard KBI. A) The DBB catheter. Inset highlights the three components of the DBB. B) Angiographic image showing potential overexpansion (arrow) of the proximal RCA MB stent after standard KBI. C) The DBB system inflated at the bifurcation of the LCx and marginal branch overexpansion technique. D) Angiographic image showing no overexpansion (dotted arrow) of the proximal LCx MB stent after DBB inflation with marginal SB. E) X-ray image showing potential overexpansion of the proximal RCA MB (arrow) stent post KBI technique in euthanised heart. F) Silicone reconstruction cast of the coronary tree euthanised heart showing potential overexpansion of the proximal MB (arrow). G) X-ray image showing no overexpansion (dotted arrow) of the proximal LCx MB stent after DBB inflation with marginal SB. H) Silicone reconstruction cast showing no overstretching of the proximal LCx (dotted arrow). DBB: dedicated bifurcation balloon; KBI: kissing balloon inflation; LCx: left circumflex artery; MB: main branch; RCA: right coronary artery; SB: side branch
The repeat proximal optimisation technique (rePOT) has also been developed to overcome the limitations of KBI. This technique includes three steps: 1) usual initial POT, 2) SB opening alone instead of KBI, 3) repeat POT, the feasibility of which has been assessed in bench tests with favourable results regarding less MoV overstretch and SB obstruction compared with other bifurcation techniques9. Regarding the technical aspects, rePOT also has the advantage of its simplicity in that operators do not need to manoeuvre two balloons simultaneously. Dérimay et al reported that, irrespective of bifurcation angle (<70° or >70°) or location (left main, or non-left main), 106 consecutive cases treated with rePOT demonstrated favourable OCT results (improving ellipticity of the proximal stent, SB obstruction, and malapposition) and six-month clinical outcomes (only one TLR case)10.
In order to perform rePOT effectively, the position of the balloon for the repeat POT is crucial; however, there are two main concerns: 1) the positional relation between the distal marker and balloon shoulder varies among the different types of balloon currently available, and 2) visualisation of the bifurcation (actual position of the carina) by 2D angiography is frequently insufficient. These factors may result in “re-carina shift” towards the SB ostium. On the other hand, regarding correction of carina shift, KBI would be more reliable. In order to translate these reported favourable OCT results of rePOT into clinical benefits, further investigation with a large randomised cohort comparing with other bifurcation techniques and with long-term follow-up is required.
Bifurcation lesions are not uniform; therefore, in order to achieve optimal results, the strategy for bifurcation PCI should be determined individually, taking into consideration all of the appropriate indications for SB intervention, techniques and devices.
Conflict of interest statement
The authors have no conficts of interest to declare.