Introduction
When you look for the consequences of kissing in websites it is common to find discussions around the possible consequences of casual, light or deep kisses. One informative medical website reports that “...a serious, tongue-tangling kiss triggers a whole spectrum of physiological processes that can boost your immunity and generally spruce up that body you work so hard to keep attractive”. On the other hand, a teenagers’ website states that “...kissing carries some risk, simply because it puts you in close, intimate contact with another person (and all his/her germs)...”.
To date, the value of kissing balloon inflation (KBI) in the setting of double stenting procedures is well accepted. Yet, the decision whether or not to perform KBI during provisional stenting procedures in bifurcated lesions remains simply an unresolved doubt to be lived with. Experience tells us that each time the decision to perform KBI is taken a wide spectrum of consequences is to be expected, ranging from an outstanding angiographic result to nasty side branch (SB) dissections calling for further interventions such as stenting. Whilst in this issue of EuroIntervention readers may find the latest piece of evidence in the field1, we will try to provide a practical overview on what has been recognised so far on KBI in what follows.
How to reduce the occurrence of unplanned kisses
The provisional approach may be practised in different ways. KBI represents the most adopted technique to dilate the SB. After implantation of a stent in the main vessel (MV) across the SB take-off (“crossover” stenting), an appreciable risk of SB compromise exists and may compel operators to perform bail-out SB interventions. Historically, so-called “plaque shift” has been recognised as a possible mechanism for SB compromise. However, we now know that the main cause of SB worsening after MV stent implantation is the so-called “carina shift”, which consists of stent-induced displacement of the flow divider soft tissue into the SB2,3. Such recognition prompted an important refinement in crossover stenting. In particular, the selection of an MV stent with a 1:1 ratio to the distal MV reference diameter is expected to reduce vessel wall distal overstretching and to minimise SB occlusion by carina shift4. When such a selection is made, systematic proximal MV stent post-dilation, using the proximal optimisation technique (POT), should be performed routinely in order to ensure stent strut apposition to the vessel wall5.
Learning to kiss: key lessons from simulations
Historical bench test studies documented that, after crossover stenting, isolated SB post-dilation without simultaneous or subsequent MV dilation is unadvisable. Indeed, it may induce carina shift towards the MV and lumen reduction in the MV distal to the carina6. This phenomenon is known to be accentuated when large balloons are adopted for the SB. On the other hand, KBI has clearly been shown in bench testing to allow appropriate SB treatment as well as MV lumen preservation6. More recently, emphasis has been placed on MV overstretching induced by the overlapping balloons. In particular, an unnatural oval shape is induced by kissing balloons7, so that the selection of short balloons (thus limiting the length of the overstretched area in the proximal MV) and eventual proximal MV reshaping by re-POT may be considered.
Besides such observations, the most confusing finding stemming from simulation studies is related to the fact that the modification induced in tubular stents by KBI is strongly dependent on the SB rewiring site5. In particular, as shown in Figure 1, a completely different DES deformation is induced when KBI is performed after proximal or distal SB rewiring, and SB scaffolding is achieved only when SB rewiring has been performed at the level of the distal SB ostium. Thus, in clinical practice with KBI, meticulous attention should be paid to the previous, critical, step of SB rewiring. In particular, a pullback rewiring technique8 as well as careful monitoring by angio9 or intracoronary imaging10 may be considered in order to enhance the chances of performing KBI in addition to distal SB rewiring.
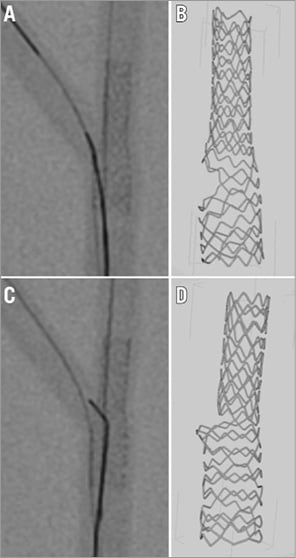
Figure 1. Impact of rewiring site on kissing-induced stent deformation. The results of bench tests performed using a latest-generation DES (Resolute Onyx™ 3×18 mm; Medtronic, Minneapolis, MN, USA) exposed to POT and kissing balloon inflation performed in addition to proximal rewiring or distal side branch rewiring. On the left, the proximal rewiring (A) and distal rewiring (C) phases performed after POT are shown. On the right, the microCT of the final results obtained with kissing balloon inflation after proximal rewiring (B) and distal rewiring (D) are illustrated, showing a completely different aspect.
Finally, it should be emphasised that different metallic platforms of DES respond differently to KBI in terms both of side cell dilation and of SB ostium scaffolding4. This means that the same technical sequence of SB rewiring and kissing may result in significantly different patterns of stent deformation according to the type of DES selected. The possible clinical relevance of these observations has been highlighted by the results of a recent trial which showed, in patients treated by PCI according to the provisional approach, better acute angiographic results in the SB using a latest-generation everolimus-eluting stent as compared with a first-generation sirolimus-eluting stent11.
Kissing everyone may not be advisable!
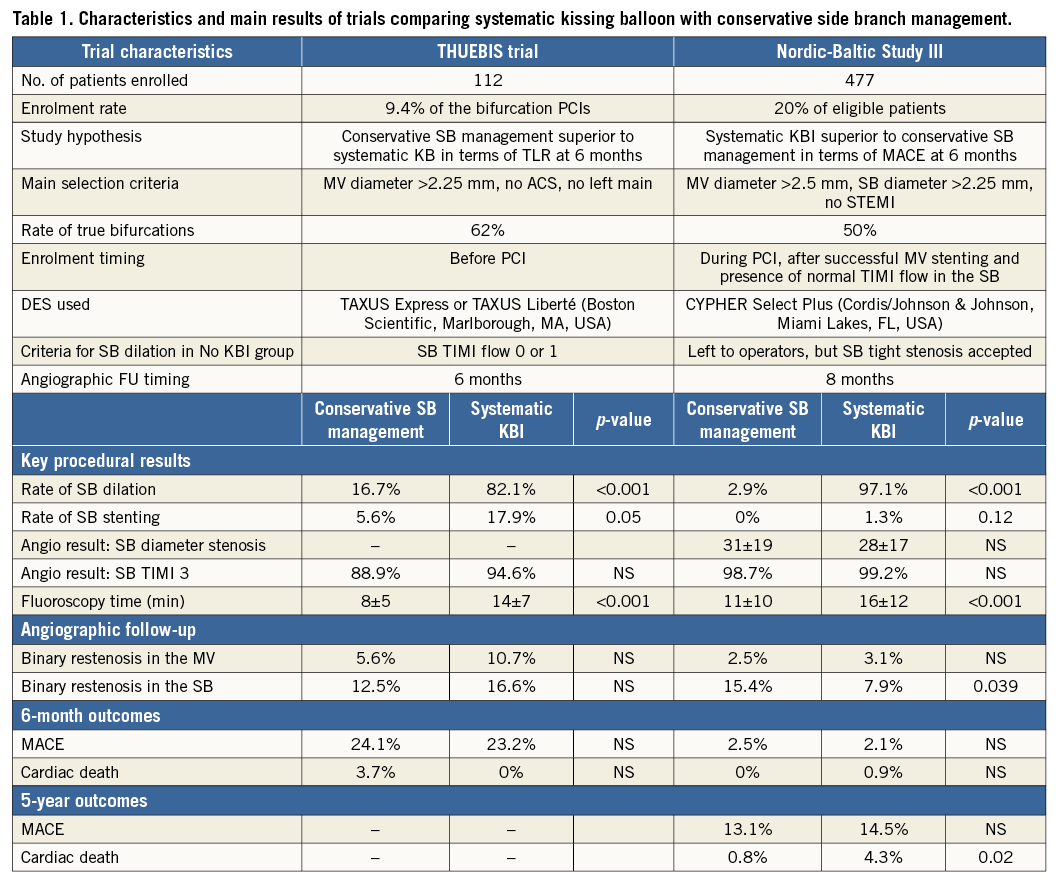
The possible value of systematic KBI use has been explored in two randomised trials (the THUEBIS study12 and the Nordic-Baltic Bifurcation Study III13), whose characteristics are summarised in Table 1. Both studies were conducted on selected subgroups of bifurcation interventions since randomised patients represented <20% of those undergoing bifurcation stenting in the enrolling institutions (Table 1). For instance, since the overall risk of study patients was lower as compared with that expected by the two investigators’ teams12,13, it may be speculated that higher-risk patients were excluded. According to the study protocols, first-generation DES only were used (Table 1), while the SB rewiring technique and rewiring site control were not considered. The overall results (Table 1) suggested that, after first-generation DES implantation in the MV, systematic KBI is feasible, may be associated with better angiographic results in the SB at six to eight-month follow-up but does not improve early clinical outcome. Recently, the five-year follow-up data of patients randomised in the Nordic-Baltic Bifurcation Study III have been disclosed (Niemela, oral presentation at TCT 2015), reporting similar MACE rates but increased mortality in the systematic KBI group.
Further support in favour of a conservative SB management strategy recently came from the SMART-STRATEGY trial14. The authors randomised 258 patients undergoing provisional bifurcation stenting to a conservative or an aggressive SB intervention strategy. The following criteria for performing an SB intervention after MV stenting were adopted for SB intervention in the conservative and aggressive strategy groups: TIMI flow grade <3 versus diameter stenosis >75% for non-left main bifurcations and diameter stenosis >75% versus diameter stenosis >50% for left main bifurcations. Power calculations were based on an expected 12-month target vessel failure rate of 24% in the conservative group; however, a 9.4% rate was observed, thus reflecting a lower than expected risk profile of the enrolled patients. At one year, target vessel failure was similar between the two arms but a lower rate of periprocedural myocardial necrosis and higher SB restenosis at angiographic follow-up were observed in the conservative strategy group.
Altogether, these observations suggest that systematic KBI cannot be recommended and that a conservative management of the SB is advisable, especially when patients with a lower-risk profile (similar to those enrolled in such trials) are treated.
Remember that nice kissing may have good effects on the heart!
Even if KBI has not been recognised as significantly improving late clinical outcome, it is practised daily worldwide. Why does this happen? The main answer is that KBI has been proven in clinical practice to play a valuable role in bifurcation interventions. First of all, in the case of a large territory supplied by the SB, it facilitates access to the distal branches in case of the need for further interventions (the “open door” concept) (Figure 2). Secondly, as it is an extensively adopted technique to treat the SB in the context of the provisional approach, KBI has been documented as having a series of favourable periprocedural and late beneficial effects. In particular, the performance of KBI has been associated with:
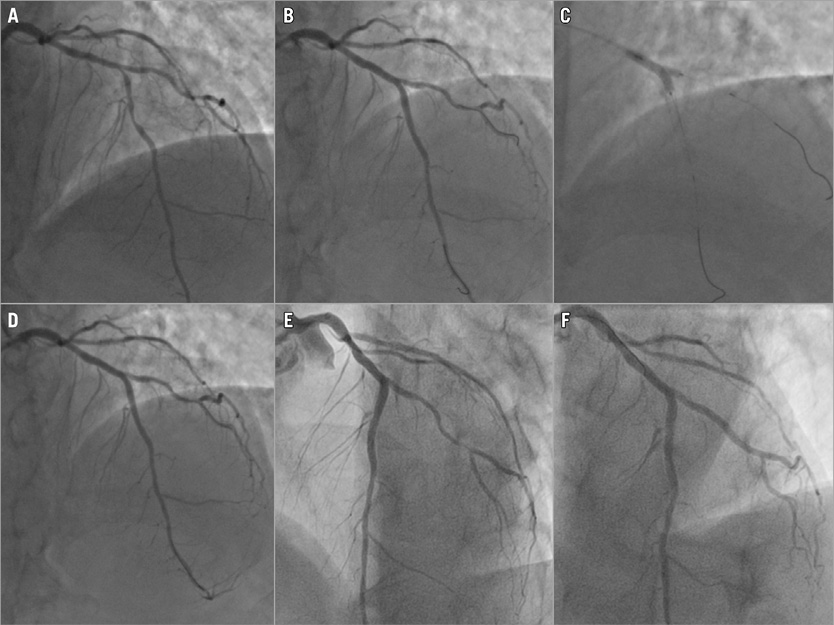
Figure 2. Example of the “open door” concept for kissing balloon inflation. A) Pre-PCI angiography showing left anterior descending/diagonal bifurcation. B) After crossover stenting, the diagonal branch was fairly patent. The operator decided to perform KBI (C) obtaining a final result (D) which was angiographically similar to that obtained before kissing. E) After one year, the patient presented with acute coronary syndrome. Urgent angiography showed subocclusion of the distal segment of the diagonal branch. Two wires and a long stent were easily advanced into the lesion through the left anterior stent side cells opened by kissing (“open door”) at the time of the first intervention, obtaining an optimal angiographic result (F).
– higher fractional flow reserve values in the SB after MV stenting15.
– improvement of FFR in the SB when a suboptimal result is noticed after MV stenting16.
– reduced post-procedural myocardial inducible ischaemia17.
– significant SB restenosis reduction at angiographic follow-up1,13,14.
– significant reduction of uncovered stent struts and thrombus formation over the SB ostium at six- to 12-month follow-up18.
Conclusions
Evidence collected by independent groups in a series of multiple studies suggests that the KBI technique plays a pivotal role in the technical armamentarium of interventional cardiologists practising bifurcation stenting.
Randomised trials have shown that the systematic use of KBI is not advisable. Nevertheless, KBI, especially when practised in a refined way (coupled with the POT technique and performed after distal SB rewiring), may help to treat effectively both branches of selected bifurcated lesions with a single DES (Figure 3).
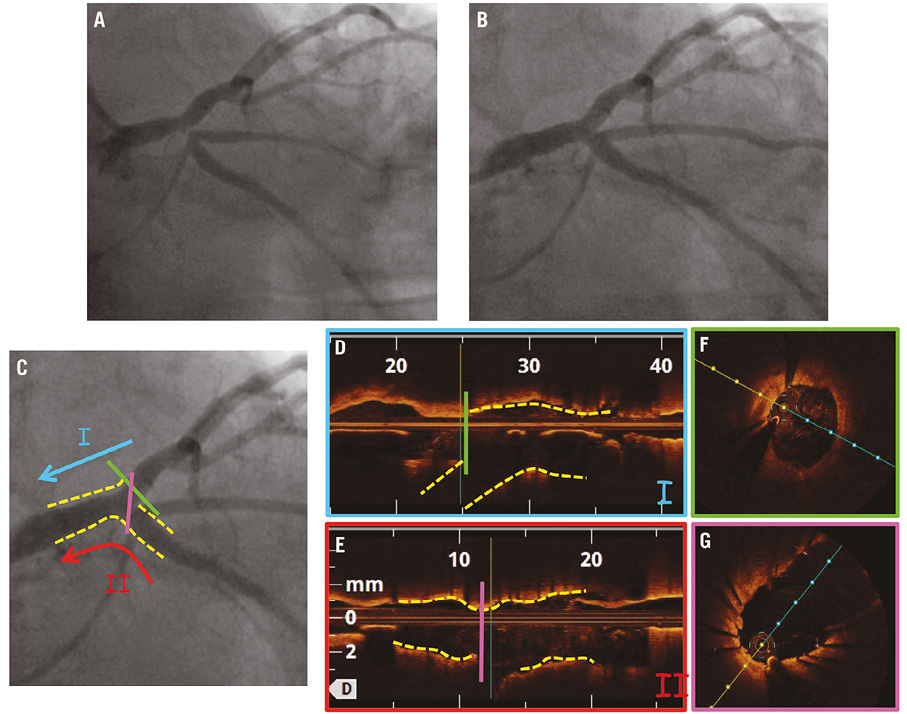
Figure 3. Clinical example of KBI effectiveness. A) Pre-PCI angiography showing tight lesion of the left circumflex. B) Post-PCI angiographic result after stent implantation from the left circumflex to the left main, followed by POT, distal rewiring and KBI. C) Configuration of the stent after interventions and the two axes used for imaging by optical coherence tomography. Optimal opening of the stent struts and perfect result in the ostial left anterior descending artery are documented by pullback I (optical coherence tomography long-axis reconstruction and cross-section shown in D and E, respectively). Good stent expansion and complete removal of the stent struts at the level of bifurcation are documented by pullback II (optical coherence tomography long-axis reconstruction and cross-section shown in F and G, respectively).
Conflict of interest statement
F. Burzotta discloses having been involved in advisory board meetings with Medtronic and having received speaker’s fees from Medtronic, St. Jude Medical and Abiomed. C. Trani received speaker’s fees from St. Jude Medical.