
Abstract
Aims: The impact of final kissing balloon inflation (FKBI) after percutaneous coronary intervention (PCI) of bifurcation lesions on long-term clinical outcomes remains controversial. We sought to determine the impact of FKBI on four-year outcomes after PCI of distal left main (LM) bifurcation lesions.
Methods and results: The EXCEL trial compared PCI with everolimus-eluting stents and coronary artery bypass graft surgery (CABG) in patients with left main (LM) disease. We examined four-year clinical outcomes after PCI of distal LM bifurcation lesions according to use of FKBI. The primary endpoint was the composite rate of death, myocardial infarction (MI), or stroke. The major secondary endpoint was the composite rate of death, MI, stroke, or ischaemia-driven revascularisation (IDR). Among 948 patients randomised to PCI, 759 had distal LM lesions treated, 430 of which were treated with one stent and 329 of which were treated with two or more stents. The four-year rates of the primary and major secondary endpoints were similar with versus without FKBI in both the one-stent and ≥2-stent groups in both unadjusted and adjusted analyses.
Conclusions: In the EXCEL trial, the performance of FKBI after PCI of distal LM bifurcation lesions was not associated with improved four-year clinical outcomes regardless of whether one stent or ≥2 stents were implanted.
Introduction
Coronary bifurcations remain one of the most challenging lesion subsets for percutaneous coronary intervention (PCI), with increased rates of acute complications and long-term adverse events compared with non-bifurcation lesions1. Optimal treatment of the distal left main (LM) bifurcation is particularly important given the large amount of myocardium subtended. Whether a provisional one-stent or planned two-stent strategy is preferred for bifurcation lesions continues to be debated. Several randomised trials have demonstrated that a provisional side branch (SB) stenting approach is preferred to routine two-stent implantation for many non-LM bifurcation lesions1,2,3,4, although one study reported that the double kissing (DK)-crush two-stent technique may be superior to the provisional approach in true bifurcation lesions5. The DK-crush two-stent technique has also been reported to afford better one-year outcomes than provisional stenting in true distal LM bifurcation lesions6. Regardless of whether one versus two or more stents are implanted in a coronary bifurcation, optimising the post-treatment geometry is believed to be essential to prevent stent thrombosis and restenosis1. A final kissing balloon inflation (FKBI) was one of the first specific techniques developed for bifurcation PCI and, based on bench tests, computer simulation, and intravascular imaging studies, FKBI may optimise stent apposition, correct stent deformation, improve SB access, and mitigate flow disturbances7,8,9,10. Nonetheless, the impact of FKBI on long-term clinical outcomes remains uncertain. Some non-randomised studies11,12 have suggested its utility in patients undergoing bifurcation PCI with a complex two-stent strategy. The benefits of routine FKBI after provisional bifurcation stenting are even more controversial13,14,15. Moreover, to our knowledge, the impact of FKBI on clinical outcomes after PCI of distal LM bifurcation lesions has not been examined.
The EXCEL (Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial demonstrated that PCI with second-generation everolimus-eluting stents (EES) is an acceptable or preferred alternative to coronary artery bypass graft surgery (CABG) in selected patients with LM coronary artery disease and low or intermediate SYNTAX scores16. More than 80% of patients enrolled in EXCEL had distal LM bifurcation or trifurcation lesions. The outcomes of distal LM bifurcation treatment with one versus two stents from the EXCEL trial have been reported previously17. In the present analysis we examined whether performance of FKBI influenced long-term outcomes after distal LM bifurcation PCI according to the number of stents implanted.
Methods
STUDY POPULATION
The design, enrolment criteria, and principal findings from the EXCEL trial have been described previously16,18. Briefly, 1,905 patients with LM disease and operator-assessed low or intermediate (≤32) SYNTAX scores were enrolled at 126 sites in 17 countries between September 2010 and March 2014 and randomly assigned to undergo either PCI with EES (948 patients) or CABG (957 patients). For distal LM bifurcation lesions, a one-stent provisional technique was preferred unless a large side branch (usually the left circumflex) was present with a lesion length >5 mm or in the presence of specific anatomic considerations such as heavy calcification or marked LM bifurcation angulation. The decision to perform an FKBI was also left to the discretion of the operator, but in general was recommended after implantation of one stent if a >50% stenosis or other evidence of a suboptimal side branch result was present and in most cases after two-stent implantation.
ENDPOINTS
Follow-up is currently complete up to four years. The primary endpoint was the composite rate of death from any cause, myocardial infarction (MI), or stroke. The major secondary endpoint was the rate of death, MI, stroke, or ischaemia-driven revascularisation (IDR). Additional secondary endpoints included the components of the primary and secondary endpoints as well as stent thrombosis at 30 days and four years. Detailed definitions of the endpoints have been provided elsewhere18. All endpoints were adjudicated by an independent committee. An independent angiographic core laboratory assessed the baseline SYNTAX score, the severity of LM disease, and Medina classification as well as post-procedural outcomes.
STATISTICAL ANALYSIS
The study patients were grouped according to whether they were treated with one stent or two (or more) stents and according to the use of FKBI (as-treated analysis). Continuous data were compared with t-tests unless the normality assumption failed per the Shapiro-Wilk test, in which case a Wilcoxon rank-sum test for the difference in median outcomes was used. Categorical data are presented as percent (count) and were compared using the χ2 test unless >20% of the expected cell frequencies were <5, in which case Fisher’s exact test was used. Hazard ratios (HR) and 95% confidence intervals (CI) were generated using Cox regression. Multivariable analysis was performed using Cox proportional hazards regression to adjust for the effect of potential confounders (selected for their historical relationship to the major clinical outcomes from prior studies) on the relationship between FKBI use and major composite adverse events at four years. The variables entered into these models included age, sex, diabetes, prior MI, and core laboratory-assessed SYNTAX score and Medina classification (1,1,1 versus other).
Results
BASELINE CLINICAL AND ANGIOGRAPHIC CHARACTERISTICS
PCI was the first procedure performed in 935 of the 948 patients randomised to PCI in the EXCEL trial, among whom 759 patients (81.1%) had distal LM bifurcation involvement. One stent was implanted in these lesions in 430 patients (56.7%), and ≥2 stents were implanted in 329 patients (43.3%). FKBI was performed in 175 (40.7%) of the one-stent cases and in 235 (71.4%) of the ≥2 stent cases. There were no significant differences in the baseline clinical or demographic characteristics between the FKBI and no FKBI groups in either the one-stent or the ≥2-stent group (Supplementary Table 1). The SYNTAX score was higher in the FKBI group of patients treated with one stent and similar between the FKBI and no FKBI groups with ≥2 stents implanted. Patients in whom FKBI was performed had a higher prevalence of Medina classification 1,1,1 (involvement of the distal LM as well as both the ostial left anterior descending coronary artery and the left circumflex) in both the one-stent and ≥2-stent groups. Patients treated with one stent followed by FKBI had longer lesions, smaller minimal lumen diameters (MLD), and higher percent diameter stenosis (%DS) in both the main vessel (MV) and SB compared with one-stent cases in which FKBI was not performed (Supplementary Table 2). There were no significant differences in angiographic lesion characteristics between the FKBI and no FKBI groups in patients treated with ≥2 stents except that SB lesion length was longer in FKBI cases. After one-stent PCI, the in-stent MLD was comparable in the FKBI and no FKBI groups, but the MV %DS was higher in the FKBI group. Performance of FKBI resulted in greater acute gain and SB MLD compared to no FKBI. Patients treated with ≥2 stents followed by FKBI had a greater post-procedural MLD compared to those treated with ≥2 stents without FKBI.
PROCEDURAL OUTCOMES
Performance of FKBI was associated with greater fluoroscopy time in both the one-stent and ≥2-stent groups, while the procedure duration was longer only in patients treated with one stent (Supplementary Table 3). In patients treated with one stent and FKBI, the implanted stents had smaller diameters and greater length compared with no FKBI. Longer stents were also implanted in patients treated with ≥2 stents and FKBI. LM post-stent dilatation was performed more frequently in the one-stent FKBI group compared with no FKBI, although smaller balloons were inflated with lower pressure. Post-stent dilatation use was similar in FKBI and no FKBI patients treated with ≥2 stents. Site-reported procedural complications did not differ between the groups.
CLINICAL OUTCOMES
The four-year rate of the composite primary endpoint of death, MI, or stroke in patients with distal LM bifurcations treated with one stent was 17.5% after FKBI and 15.9% after no FKBI (adjusted HR 1.12, 95% CI: 0.68-1.84, p=0.65) (Table 1, Figure 1). In distal LM bifurcations treated with ≥2 stents, the four-year composite primary endpoint was 19.8% after FKBI and 25.8% after no FKBI (adjusted HR 0.65, 95% CI: 0.38-1.10, p=0.11). Similarly, there were no significant differences in the composite major secondary endpoint of death, stroke, MI, or IDR at four years after FKBI versus no FKBI, whether treated with one stent (25.0% vs 25.9%, adjusted HR 1.02, 95% CI: 0.68-1.53, p=0.92) or ≥2 stents (32.3% vs 33.2%, adjusted HR 0.77, 95% CI: 0.49-1.22, p=0.27) (Table 1, Figure 1). Additional 30-day and four-year outcomes are shown in Supplementary Table 4. There were no significant outcome differences between the FKBI and no FKBI groups. A trend towards a higher four-year rate of definite stent thrombosis was observed in the one-stent FKBI group. A summary of each stent thrombosis case is provided in Supplementary Table 5 and Supplementary Table 6.
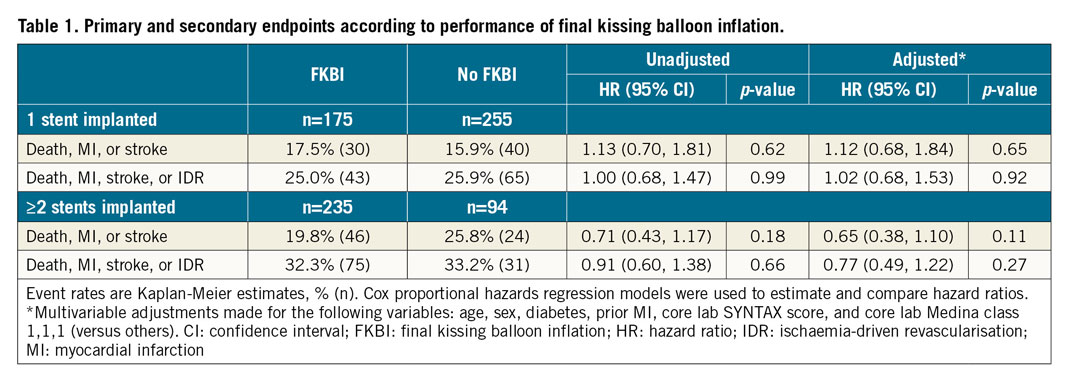
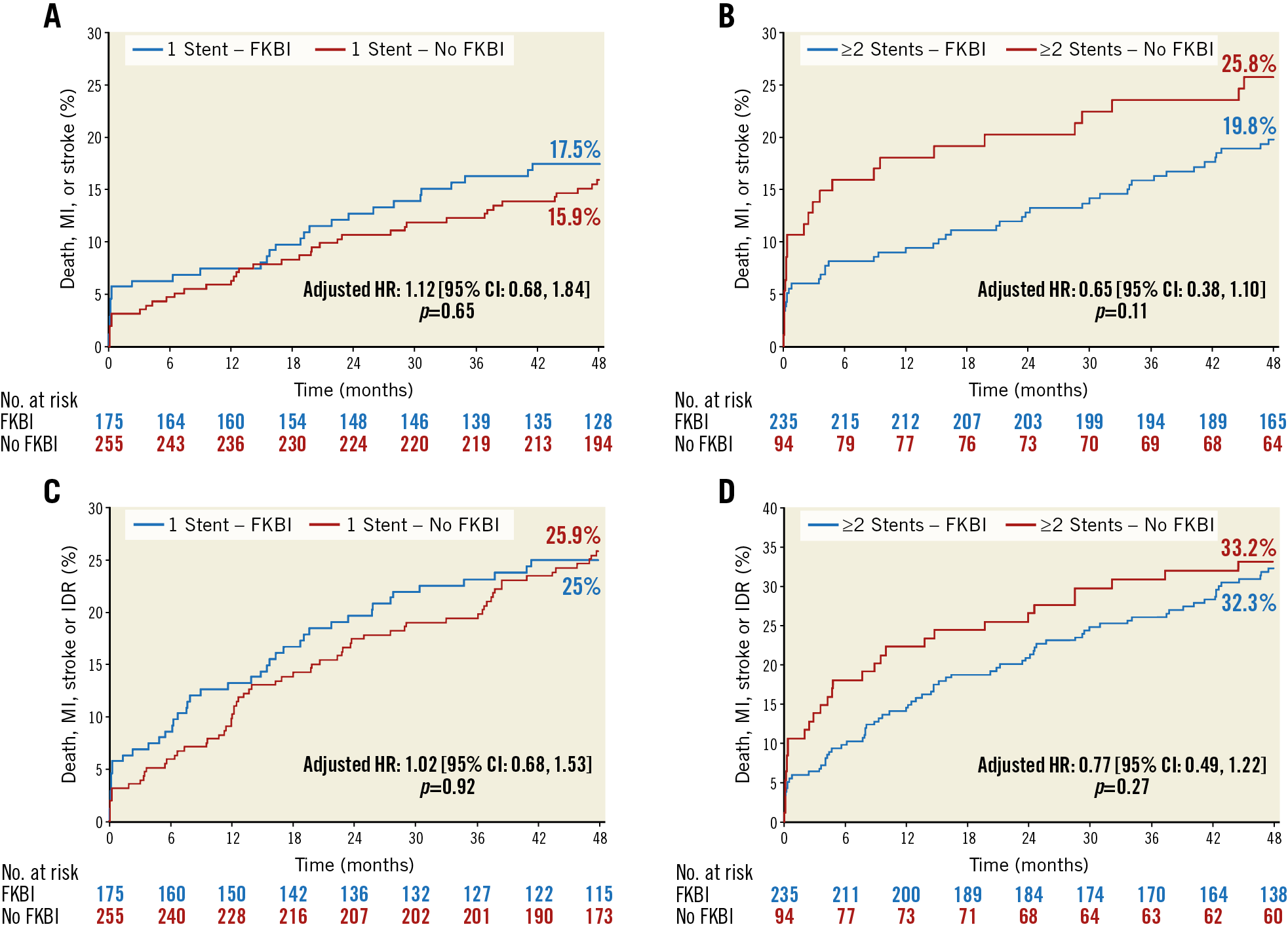
Figure 1. Time-to-event curves after distal left main treatment according to final kissing balloon inflation. The primary composite endpoint (death, MI, or stroke) with implantation of (A) one stent and (B) ≥2 stents, and for the major secondary composite endpoint (death, MI, stroke, or IDR) with (C) one stent and (D) ≥2 stents. CI: confidence interval; FKBI: final kissing balloon inflation; HR: hazard ratio; IDR: ischaemia-driven revascularisation; MI: myocardial infarction
Discussion
In the present study, we investigated the association between the performance of FKBI and long-term outcomes among patients undergoing distal LM bifurcation PCI in the EXCEL trial with implantation of either one stent or ≥2 stents. At four years, the rates of the composite primary endpoint of death, MI, or stroke and the composite major secondary endpoint of death, MI, stroke, or IDR were similar with or without FKBI regardless of the number of distal LM bifurcation stents implanted. No significant differences were noted with FKBI for other secondary endpoints at 30 days or four years. These findings suggest that a routine strategy of FKBI after distal LM bifurcation treatment may not be necessary regardless of whether one or more stents are required for treatment. Randomised trials are warranted to evaluate the utility of FKBI.
Notwithstanding the results of randomised trials with the DK-crush technique5,6, a provisional one-stent approach is considered the preferred strategy for the majority of LM19,20,21 and non-LM coronary bifurcation lesions1,2,3,4; however, a second stent is required in ~10-25% of provisional attempts1,2, and a planned routine two-stent technique is recommended for complex or severely angulated bifurcations. Regardless of whether one stent or two stents are ultimately implanted in bifurcation lesions, the benefits of FKBI remain uncertain from both experimental and clinical studies.
In an in vitro model, FKBI was demonstrated to restore distorted stent symmetry caused by SB balloon dilation through the MV struts and increased stent area8 in vivo as assessed by intravascular ultrasound (IVUS)22, which might translate into reduced restenosis and target lesion revascularisation (TLR). Conversely, other bench tests with first-generation DES demonstrated that FKBI may damage the polymer coating leading to reduced drug delivery, proximal segment elliptical deformation23, residual stent deformation, and gap formation after stenting of LM bifurcation lesions24. Intravascular imaging studies have suggested that stent area and symmetry index might not be normalised in all cases after FKBI25.
Non-randomised clinical studies have suggested that FKBI may be beneficial in bifurcation lesions treated with a two-stent approach11,12. Conversely, previous studies have reported conflicting findings for the impact of FKBI after the one-stent technique, either harmful (increased TLR), neutral, or favourable (reduced TLR)13,14,15. These discordant results may be explained by differences in study design, vessel size, lesion type and location, stenting approach, and immediate post-procedural outcomes. The only randomised trial performed to date (the Nordic-Baltic Bifurcation Study III) demonstrated reduced eight-month rates of SB angiographic restenosis with routine FKBI in one-stent treated bifurcation lesions, but no significant differences in six-month clinical outcomes; contrast use and procedural and fluoroscopy times were greater with routine FKBI compared with no FKBI14.
To our knowledge, no prior study has examined outcomes after LM distal bifurcation PCI according to the use of FKBI. The present report from EXCEL, the largest trial to date of LM PCI in which contemporary EES were used, is therefore novel and informative. Although drawn from non-randomised data, all events were monitored and adjudicated, an independent angiographic core laboratory evaluated all films, and multivariable analysis was used to adjust for clinical, angiographic, and procedural differences between groups stratified by performance of FKBI. The as-treated analysis of distal LM bifurcation lesions with one versus two or more stents implanted also provides insight into FKBI utility regardless of whether a provisional one-stent or planned two-stent technique was initially adopted. The results of the present analysis did not demonstrate clinical benefits of FKBI in distal LM bifurcation lesions treated with either one stent or ≥2 stents, and procedure duration and fluoroscopy times were greater with FKBI (although radiation dosage and contrast volume were not significantly increased). These data suggest that routine FKBI may not be necessary after distal LM bifurcation PCI if an acceptable procedural result is achieved. In this regard it should be noted that IVUS was used to guide LM treatment in nearly 80% of patients in EXCEL, and it was used more in patients treated with one-stent PCI without versus with FKBI. Whether the present results would be similar after treatment of distal LM bifurcation lesions without IVUS guidance is unknown. Finally, regardless of the technique utilised, the use of intravascular imaging guidance for stent optimisation in all cases of distal LM bifurcation PCI is recommended to improve early and late outcomes.
Although the present study suggests that routine FKBI may not be necessary after distal LM bifurcation PCI, by four years death, MI, stroke, or IDR had occurred in >25% of one-stent treated patients and in >32% of ≥2-stent treated patients (regardless of FKBI use), warranting further efforts to optimise the bifurcation technique in these high-risk patients. The DK-crush technique may improve outcomes compared to a standard crush technique; alternatively, a sequential two-step post-dilatation of the SB and MV without kissing has been proposed for provisional stenting of bifurcation lesions. This approach includes an initial proximal optimisation technique (POT), SB dilation, and final POT sequence (re-POT); in bench models this resulted in greater stent circularity and better stent apposition at the proximal stent edge.
Limitations
The decision to use FKBI in the EXCEL trial was not randomised and the detailed reasons for performing or not performing a final kiss were not collected. Therefore, although multivariable analysis was used to adjust for measured differences, whether unmeasured confounders contributed to the lack of differences between the groups cannot be excluded. The results of the present study should thus be considered hypothesis-generating. Finally, although the largest trial of its kind to date, EXCEL may still have been underpowered to detect modest differences between the groups in low frequency endpoints such as stent thrombosis. Adequately powered randomised trials are thus warranted to study the outcomes of FKBI, especially in two-stent use applications.
Conclusions
In the EXCEL trial, the performance of FKBI after PCI of distal LM bifurcation lesions was not associated with improved rates of the composite primary endpoint of death, MI, or stroke or the composite major secondary endpoint of death, MI, stroke, or IDR regardless of the number of distal LM bifurcation stents implanted. No clinical benefits of FKBI were present in distal LM bifurcation lesions treated with either one stent or ≥2 stents, and procedure duration and fluoroscopy times were greater with FKBI, although radiation dosage and contrast volume were not significantly increased. These data suggest that routine FKBI may not be necessary after distal LM bifurcation PCI if an acceptable procedural result is achieved.
|
Impact on daily practice The performance of FKBI after PCI of distal LM bifurcation lesions was not associated with improved four-year clinical outcomes in the EXCEL trial, regardless of whether one stent or ≥2 stents were implanted. No significant differences were observed with FKBI for other secondary endpoints at 30 days or four years. These findings suggest that a routine strategy of FKBI after distal LM bifurcation treatment may not be necessary regardless of whether one or more stents are required for treatment. |
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Funding
The EXCEL trial was sponsored by Abbott Vascular (Santa Clara, CA, USA).
Conflict of interest statement
G. Dangas reports grants and personal fees from Abbott Vascular and personal fees from Boston Scientific, outside the submitted work. R. Mehran reports grants and personal fees from Abbott Vascular, personal fees from Boston Scientific, grants from Medtronic, personal fees from Medscape/Web MD, personal fees from Siemens Medical Solutions, other from Philips/Volcano/Spectranetics, personal fees from Roivant Sciences, personal fees from Sanofi (ITA), grants from AstraZeneca, grants from Bayer, grants from Beth Israel Deaconess, personal fees from Janssen, grants and other from BMS, grants from CSL, grants from DSI, grants from Novartis, grants from OrbusNeich, personal fees from Watermark Research, personal fees from Medtelligence (Janssen), personal fees from ACC, personal fees from AMA, other from Abiomed, other from The Medicines Company, other from Claret Medical, and other from Elixir Medical, outside the submitted work. U. Baber receives honoraria from Boston Scientific and AstraZeneca. D. Kandzari reports consulting honoraria from Medtronic, Biotronik, Boston Scientific and research/grant support from Medtronic, Biotronik and Boston Scientific. M. Leon receives institutional grant support from Abbott, Boston Scientific, Medtronic and Edwards Lifesciences and personal fees from Gore Medical and Meril Life Sciences. P.W. Serruys reports personal fees from Abbott Laboratories, AstraZeneca, Biotronik, Cardialysis, GLG Research, Medtronic, Sino Medical Sciences Technology, Société Europa Digital & Publishing, Stentys France, Svelte Medical Systems, Philips/Volcano, St. Jude Medical, Qualimed and Xeltis, outside the submitted work, and is a consultant for Biosensors, Medtronic, Micell Technologies, SINOMED, Philips/Volcano, and HeartFlow. A.P. Kappetein is an employee of Medtronic. J. Sabik is a consultant to and reports personal fees from Medtronic, Edwards Lifesciences and Sorin, outside the submitted work, and grants from Abbott, and is on the Advisory Board of Medtronic Cardiac Surgery. S. Sharma receives honoraria and is on the Speakers Bureau of Abbott, Boston Scientific, and Cardiovascular Systems, Inc. G. Stone receives speaker honoraria from Terumo and Amaranth, is a consultant to Shockwave, Valfix, TherOx, Reva, Vascular Dynamics, Robocath, HeartFlow, Gore, Ablative Solutions, Matrizyme, Miracor, Neovasc, V-wave, Abiomed, Claret, Sirtex, Ancora, MAIA Pharmaceuticals, Spectrawave, Orchestra Biomed and Qool Therapeutics, and has equity/options in Qool Therapeutics, Cagent, Applied Therapeutics, Biostar family of funds, MedFocus family of funds, Spectrawave, Orchestra Biomed, Aria and Ancora. The other authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.
Supplementary data
To read the full content of this article, please download the PDF.

