
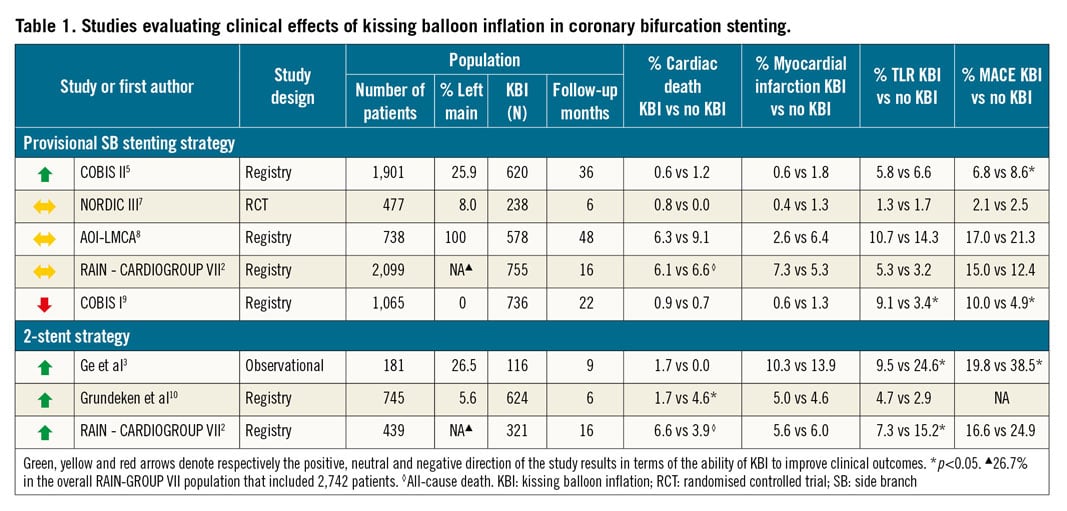
The goal of coronary bifurcation percutaneous coronary intervention (PCI) is optimal stent deployment/apposition, aimed at restoring natural fractal vessel geometry and blood flow pattern. Among different optimisation strategies, the proximal optimisation technique (POT) is recommended by expert consensus as a mandatory procedural step, while the use of kissing balloon inflation (KBI) has shown consistent clinical benefit and should be obligatory in two-stent strategies, whilst it remains optional in provisional side branch (SB) stenting due to conflicting evidence (Table 1).
In this issue of EuroIntervention, Kini et al1 present a sub-analysis of the EXCEL trial (Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularisation), which investigated the impact of final KBI in 759 patients undergoing distal left main (LM) bifurcation stenting, 430 of whom were treated with one stent and 329 with ≥2 stents.
The main findings were that the four-year composite of death, myocardial infarction (MI) or stroke was similar with and without final KBI in both patients treated with one stent (17.5% vs 15.9%, respectively; adjusted HR 1.12, 95% CI: 0.68-1.84, p=0.65) and those treated with ≥2 stents (19.8% vs 25.8%; adjusted HR 0.65, 95% CI: 0.38-1.10, p=0.11). There was also no difference in the target lesion revascularisation (TLR) rates. Although KBI did increase the overall procedural and fluoroscopy time, this was not paralleled by an increase in radiation exposure or contrast volume, nor were there more periprocedural complications (including periprocedural MI) reported. Therefore, in this EXCEL sub-analysis, performing KBI did not improve outcomes of LM PCI, but there was also no penalty attached. While this was expected in patients treated with one stent, given the prior evidence, the absence of outcome improvement with KBI in patients treated with two-stent bifurcation PCI may be surprising2,3.
Therefore, and notwithstanding the main limitations of this secondary analysis, namely its non-randomised design with possible selection bias, and the lack of a standardised protocol for the use of final KBI, the following additional points may also need to be taken into consideration when interpreting the overall results.
First, the subgroup of patients with ≥2 stents implanted was heterogenous with respect to both the intention to perform two-stent PCI (planned versus bail-out) and to the stenting technique (T/TAP versus Culotte versus Crush versus V/simultaneous kissing stent [SKS]). Moreover, the majority of patients with ≥2 stents implanted but without final KBI were initially subjected to a provisional strategy (60%), and almost all were ultimately treated with the T or TAP technique (only five patients were treated with other two-stent techniques in the non-final KBI group). This heterogeneity appears not to have been accounted for in the analysis.
Second, no specific details are provided with regard to the technique of KBI used in the trial. Since prior studies associated the use of non-compliant balloons with sequential balloon inflation4 and short proximal overlap2 with improved outcomes5, these variables could potentially be effect modifiers and would need to be considered in the overall analysis.
Third, bifurcation stenting optimisation has increasingly been understood as a concept of adapting stent geometry to the underlying bifurcation anatomy. This is particularly relevant in bifurcations with a large side branch (SB), where there is a greater discrepancy between the proximal and distal main vessel (MV) diameters, such as the LM, so that stenting optimisation may go beyond a single technique, such as KBI. When stent size is selected according to distal MV reference, performance of POT is mandatory to correct malapposition and distortion in the proximal part of the MV4. The advantage of KBI, in addition to better stent expansion in the proximal MV, is relocation of the carina in the centre, with an improvement in wall shear stress pattern4. However, the effect of the interaction of POT and KBI on the procedural result and clinical outcomes has not been well established. Consequently, the rate of POT, which seems not to be specifically reported in the manuscript, may have significantly impacted on the result of KBI and the outcomes in both patients with one and in those with ≥2 stents implanted in the LM.
Fourth, even though intravascular ultrasound (IVUS) was used in ≈80% of the cases, it is not reported whether there was any standardised protocol mandating action in terms of immediate post-stenting result optimisation. This is important since a recent study confirmed the primacy of a standardised protocol over non-standard IVUS protocols for improving outcomes of LM PCI6.
In summary, this and prior studies (Table 1) seem to suggest no clear penalty associated with performing KBI, whereas its potential benefits may depend on a specific stenting technique (one- versus two-stent), underlying anatomy, complementary use of other optimisation techniques, such as POT, and a procedural feedback loop that is based on an actionable standardised intracoronary imaging protocol6. Taken together, it thus seems to be a question of when and how, rather than if, KBI should be performed in LM PCI.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.

