Abstract
Final kissing balloon inflation (KBI) after provisional bifurcation stenting has failed to provide clear clinical benefit except for a decrease in side branch stenosis, while a significant reduction of major adverse cardiac events has been documented in two-stent deployment. The optimisation of KBI in terms of proximal optimisation technique, appropriate guidewire re-crossing, minimal balloon overlapping, and balloon size selection may overcome the drawbacks of conventional KBI by: 1) correcting the proximal malapposition expected from fractal geometry; 2) optimising side branch ostium strut opening while conserving a bifurcation area free of malapposition at both the carina and the side branch ostium; and 3) optimising the geometry, velocity fields and shear rate.
Benefit and risk of final kissing balloon inflation
EFFICACY IN A ONE-STENT STRATEGY
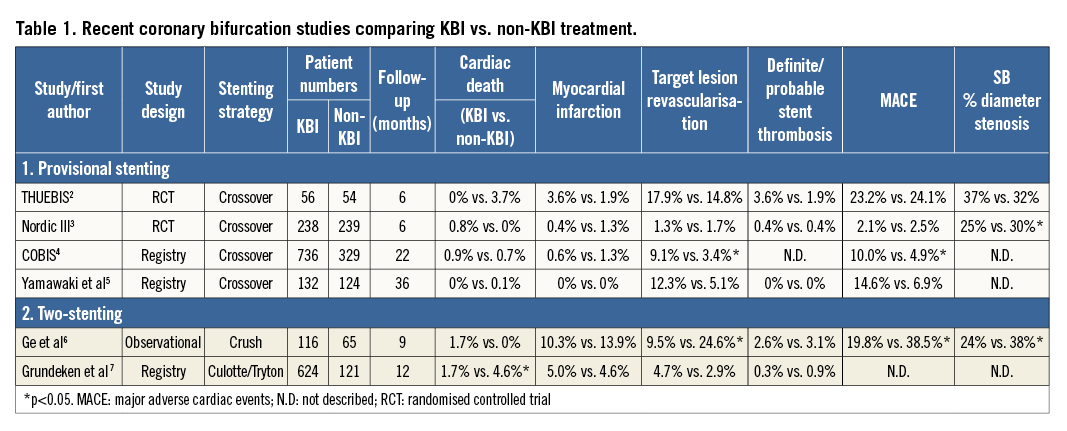
Final kissing balloon inflation (KBI) when the main vessel (MV) and side branch (SB) balloons are simultaneously inflated has been thought to be effective after crossover MV stenting in order to secure SB patency, reduce SB stenosis and remove jailed struts1. The clinical outcomes of recent studies comparing KBI vs. non-KBI are listed in Table 1 2-7. Most studies failed to show its advantage over non-KBI treatment in terms of the rate of major adverse cardiac events (MACE), despite lowering SB % diameter stenosis at six to 12-month follow-up2-5. In the Korean Coronary Bifurcation Stenting (COBIS) registry, KBI was associated with a higher MACE rate4. On the contrary, the effectiveness of KBI on MACE was reported in a small observational study of acute coronary syndrome (n=251, 8.2% vs. 20.3%, hazard ratio 0.398, 95% CI: 0.190-0.836, p=0.015)8. The COBIS II registry demonstrated that the occlusion of the SB after MV stenting was associated with more frequent cardiac death and myocardial infarction (n=2,227, hazard ratio 2.34, 95% CI: 1.15-4.77, p=0.02)9, which suggested the importance of KBI to secure SB patency.
FATE OF THE SIDE BRANCH
The long-term effects of a jailed strut at the SB ostium are unclear. A six-month follow-up study of SB treatment guided by fractional flow reserve (FFR) revealed no significant worsening of FFR in the non-SB treatment group1. However, opening the jailed strut and relieving the SB stenosis may lead to improvement in flow distribution and shear stress1. A recent study of optical coherence tomography (OCT) revealed that a thrombus, defined as a protruding mass beyond the stent strut into the lumen with significant attenuation, was more often attached in the jailed struts of the group without (30.4%) rather than with (5.3%) final KBI10. Endothelialisation on the jailed struts may increase the risk of SB restenosis (Online Figure 1)11. Further studies are needed to assess the effects of jailed struts on the coronary blood flow, which may be related to the development of restenosis or thrombosis.
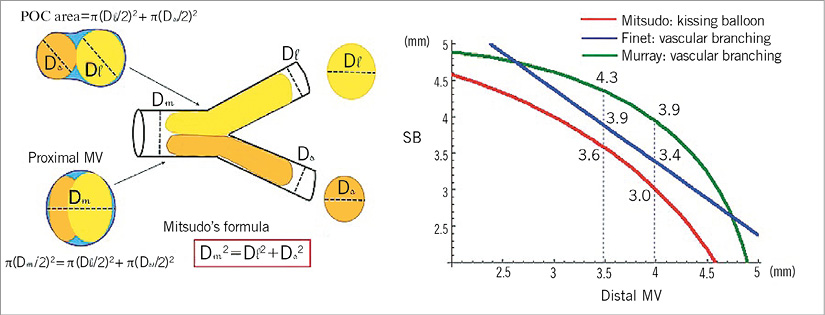
Figure 1. KBI formula and vascular branching law. A) Principle of KBI formula (Mitsudo’s law). B) Correlation between main branch and SB sizes in mother vessel size of 5 mm in various vascular branching laws.
STENT DEFORMATION IN THE MOTHER VESSEL
Final KBI consists of juxtaposing two non-compliant balloons12 with diameters sized respectively according to the diameters of the daughter vessels: distal main branch (MB) and SB. The expected summed diameter of both balloons in the mother vessel (MoV) turned out to be in disagreement with the principle of minimum energy cost (Murray’s law), which relates the MoV diameter DMoV to the two daughter vessels such that DMoV3=DMB3+DSB3, or the linear fractal ratio for coronary bifurcations based on angiographic analysis (Finet’s law), which indicates that DMoV=0.68 (DMB+DSB)13. In practice, the MoV expansion induced by the KBI results in the proximal diameter being not circular but rather oblong or elliptical (Figure 1A). By computational modelling and in vitro bench testing, Mortier et al found an ellipticity ratio of 1.3614. The negative impact on fluid dynamics, stress and strain distribution has been clearly illustrated15,16.
This elliptical MoV deformation is part of the reason for the lack of clinical benefit found with KBI2-5. In the COBIS registry, quantitative angiographic analysis found a linear fractal ratio of 0.72, with more than 18% arterial diameter overstretch, leading to more frequent reintervention in the MV (8.5%) vs. the SB (3.4%) and also in the KBI (9.1%) vs. the non-KBI group (3.4%)4.
PROXIMAL MALAPPOSITION
In the KBI procedure, the diameter selected for the main vessel balloon should fit the diameter of the distal site (MB) to prevent carina shift17. Since the differential of the diameter between proximal (MoV) and distal sites (MB) may be about 0.4 to 1.3 mm, it has a risk of inducing stent malapposition in the MoV segment18. The SB balloon overlaps at the carinal site, so that balloon juxtaposition in the MoV is about half of the balloon length. If the stented length in the MoV is greater than the balloon overlapping site, the proximal malapposition will not be corrected due to a partially juxtaposed balloon; proximal malapposition or bottleneck may be induced (Figure 2A1-2, Figure 2B1-2)19. Proximal malapposition can be corrected by the inflation of a short optimally sized balloon only in the MoV (proximal optimisation technique [POT]) (Figure 2B3, Figure 2C1-3).
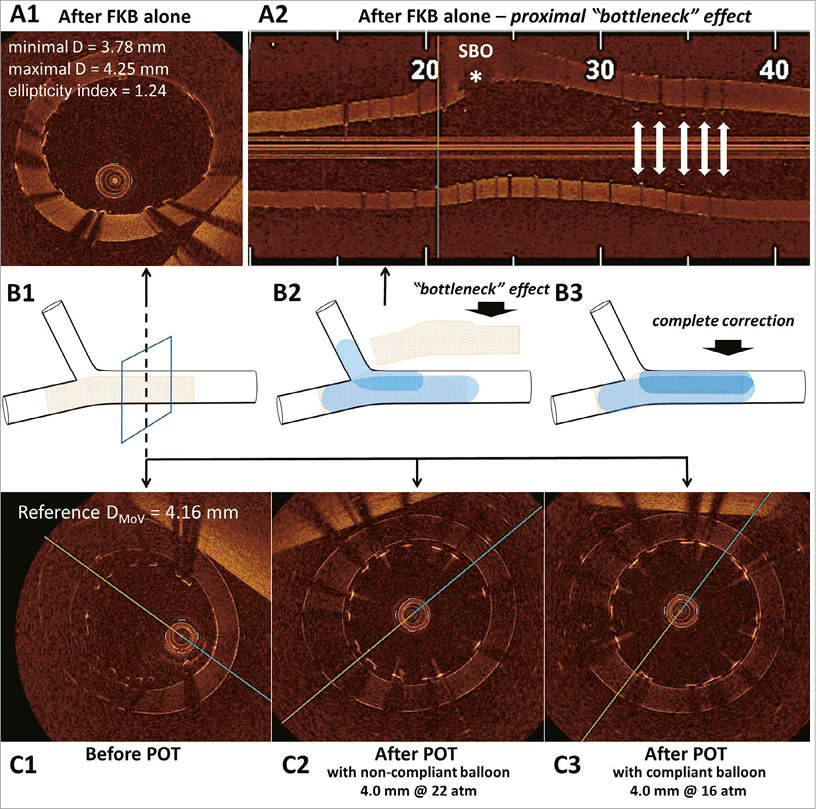
Figure 2. Detrimental effects of final kissing balloon (FKB) and one pitfall in proximal optimisation technique (POT) in provisional stenting. A1) The elliptical mother vessel deformation with arterial overstretch after FKB. A2) “Bottleneck effect”: proximal stent malapposition predicted by fractal bifurcation geometry and not completely corrected when the two balloons are not juxtaposed in this proximal segment. B1) 2D-OCT cut plane for A1, C1, C2, C3. B2) & B3) Schematic representations. C1) Before POT: the expected proximal stent malapposition with respect to the fractal ratio for coronary bifurcation. C2) Incomplete correction of stent malapposition when POT is performed with non-compliant balloon. C3) Complete and perfectly circular correction when POT is performed with compliant balloon.
EFFICACY IN THE TWO-STENT TECHNIQUE
In the two-stent technique, KBI plays a pivotal role for acquiring adequate expansion and apposition of the stents (Online Figure 2). In crush stenting, KBI reduced SB restenosis (hazard ratio 1.79, 95% CI: 1.14 to 2.80, p<0.01) (Table 1)6. Double kissing crush stenting (DK crush) which required two KBI procedures after SB and MV stentings provided a lower cumulative MACE rate (11.4% vs. 24.4%, p=0.02) than standard crush stenting with lower performance of the KBI (100% vs. 78%, p<0.001)1. Favourable KBI effects on restenosis were also reported in culotte stenting (odds ratio: 0.37, 95% CI: 0.13 to 1.10, p=0.07)1. The IVUS study indicated that the optimal threshold of minimal stent area to minimise SB restenosis was 4.83 mm220. In order to achieve adequate stent expansion, high-pressure ballooning in each daughter branch and KBI are generally recommended; however, this has not yet been formally investigated in a randomised trial. A recent report on final KBI after culotte stenting using the SB-dedicated Tryton stent (Tryton Medical, Inc., Durham, NC, USA) did not show any significant advantage over the treatment without KBI except for a lower cardiac death rate7. Its unique design of a large-sized cell in the proximal zone may provide possible advantages over the standard two-stent technique using normal stents.
HOW TO OPTIMISE FINAL KISSING BALLOON INFLATION
GUIDEWIRE CROSSING LOCATION/SIDE BRANCH ACCESS
With the prevalence of the open-cell design, which has in general three connectors or less, stent design is nowadays not generally a limiting factor for SB optimisation15,19,21-25. The cell opening that can be obtained with dilatation of a side branch through the stent mesh is sufficient to accommodate even a large SB diameter15,19,21-25.
It is recommended to re-access the SB through a distal cell of the MV stent in order to achieve an optimal opening of the ostium and scaffolding at the SB take-off (Online Figure 3)15,19,21-25. Re-crossing into the SB through a proximal cell leads to a significant lower area of the SB lumen free of struts and a higher rate of strut malapposition in front of the flow divider (neo-carina) (Online Figure 3)15,19,21,22. Furthermore, struts left unapposed in the path of the central highest velocity components produce high shear disturbance22. High shear rate is known to induce platelet activation and potential thrombosis cascade23.
Intravascular imaging with OCT is useful to guide the guidewire re-crossing in a distal centred cell prior to SB dilatation, and was shown to reduce strut malapposition significantly compared to angiographic guidance (9.5% vs. 42.3%, p<0.0001)26. On the contrary, the presence of a link between hoops at the carina increased the percentage of incomplete stent apposition compared to the type without it (12.2±6.5% vs. 0.7±0.9%, p=0.0074)27.
SELECTION OF BALLOON SIZE
In the selection of balloons for KBI, the references of both MB and SB should be assessed. Theoretically, the dilated balloon areas in daughter branches are maintained in the MoV (Figure 1A), and the sum of these areas is ideally identical to the MoV luminal area, thus the following formula (Mitsudo’s law) is introduced: DMoV2=DMB2+DSB2. An IVUS study of the left main bifurcation revealed that the mean MoV stent diameter was significantly correlated with Mitsudo’s law28. Another IVUS analysis of normal and diseased bifurcation revealed that vessel size of the external elastic membrane obeyed Murray’s law29. The correlation between MB and SB sizes in an MoV size of 5 mm is shown in Figure 1B. Both Murray’s and Finet’s laws13,18 always indicate higher values than Mitsudo’s law. Since both Murray’s and Finet’s laws demonstrate that the area of MoV is smaller than the sum of the areas of the two daughter branches, KBI using an optimally sized balloon for each branch is most likely oversized in the MoV. Therefore, it is important to select non-compliant balloons with a wide working range capable of accomplishing the requirements both of quarter-size down dilation during KBI according to Mitsudo’s law and of full expansion in the isolated dilation of each branch according to Finet’s law, which is more consistent with the actual vessel size of each bifurcated branch than Murray’s law18.
PROXIMAL OPTIMISATION TECHNIQUE (POT)
The aim of the POT is to facilitate rewiring and access to the SB by inflating in the proximal part of the stent and bifurcation a balloon large enough to appose the proximal stent segment and enlarge the stent cell facing the SB ostium12,17. In vitro experiments show how the POT technique can help in SB re-crossing and SB optimisation (Figure 3)12,17.
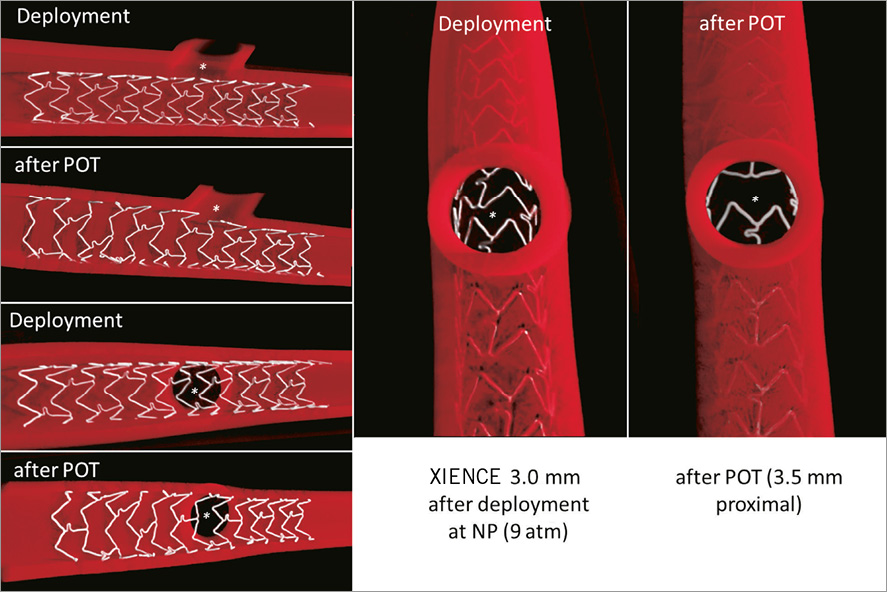
Figure 3. Impact of the POT technique on stent apposition and SB access. Comparison of the differences in stent configuration and cell available for re-crossing before (deployment) and after POT. View of the strut configuration from the SB (right panel) shows how POT can facilitate re-crossing by creating a “funnel effect” through enlargement of the cells located in front of the SB, reducing the number of possible cells available for crossing19.
During KBI, the added diameters of the two balloons overlapping can exceed the MoV reference diameter, producing an asymmetric expansion of the stent and leading to some arterial overstretch with extensive distortion of the stent strut proximal to the SB in in vitro experiments22. Oversizing and the non-uniformity of proximal stent expansion can be limited by minimising balloon overlap as far as possible, then performing proximal dilation of the MoV with an optimally sized balloon12,16,24. Completing the KBI procedure by a final POT restores proximal stent circularity (ellipticity index, 1.11±0.04 vs. 1.39±0.06) and reduces strut malapposition (0.6% vs. 33%, p=0.02) but maintains arterial overstretch in the segment (8.5±0.6 mm2 vs. 6.8±0.4 mm2, p<0.0001)24.
MODIFICATION OF KISSING BALLOON INFLATION
To reduce proximal deformation, a “modified KBI approach” was recently proposed, using asymmetric inflation pressures: the SB is first inflated to 12 atm, then partly deflated back to 4 atm with simultaneous inflation of the MB balloon at 12 atm14. This achieved significantly reduced proximal deformation (the ellipticity index falling from 1.36 to 1.17) with an unchanged rate of malapposed struts and less SB ostial stenosis. Even more interesting is the comparison between standard KBI versus a sequential approach without KBI (SB first and final POT) as tested on a bench model15: strut malapposition was significantly reduced in the MoV (2.8±9.6% vs. 30.7±26.4%, p=0.002). These techniques should be validated in the clinical setting.
Conclusions
In most of the clinical trials of provisional coronary bifurcation stenting, final KBI has failed to provide significant clinical benefits except for the reduction of SB angiographic restenosis. However, these disappointing results may be attributed to non-uniform and oversized stent dilation induced by suboptimal KBI. Optimising the KBI procedure is proposed in order to: 1) correct the proximal malapposition by final POT; 2) optimise SB ostium strut opening with proper guidewire re-crossing in the distal cell, and 3) select the appropriately sized device and procedure for optimising the geometry, coronary flow and shear stress according to vascular branching law. Since these procedures are lacking in clinical evidence, large clinical trials will be required to validate them.
Conflict of interest statement
The authors have no conflicts of interest to declare.
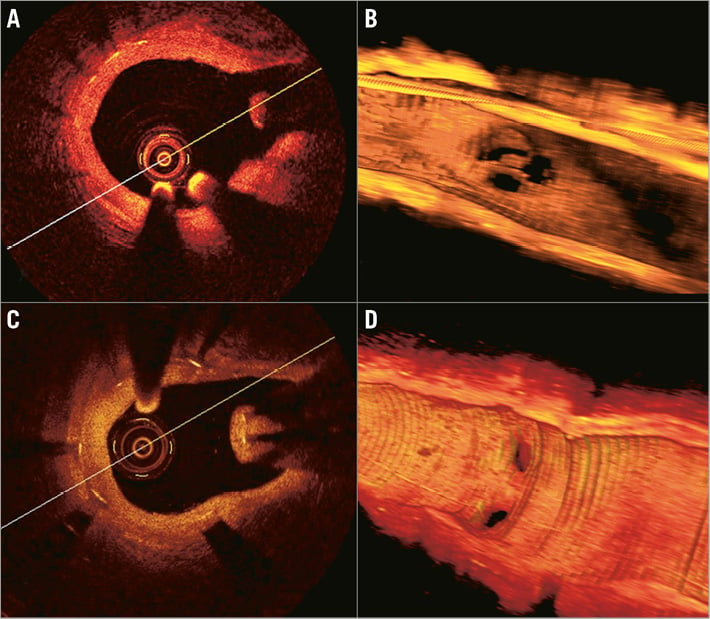
Online Figure 1. Intimal hyperplasia on jailed struts in non-KBI treatment. Diffuse in-stent hyperplasia along the proximal LAD segment with floating struts covered by neointimal proliferation (A) with some restenosis at the diagonal branch ostium in the 3D imaging of OCT (B). The septal branch ostium in the middle LAD was completely covered with more serious restenosis (C, D) (adapted from Foin et al11).
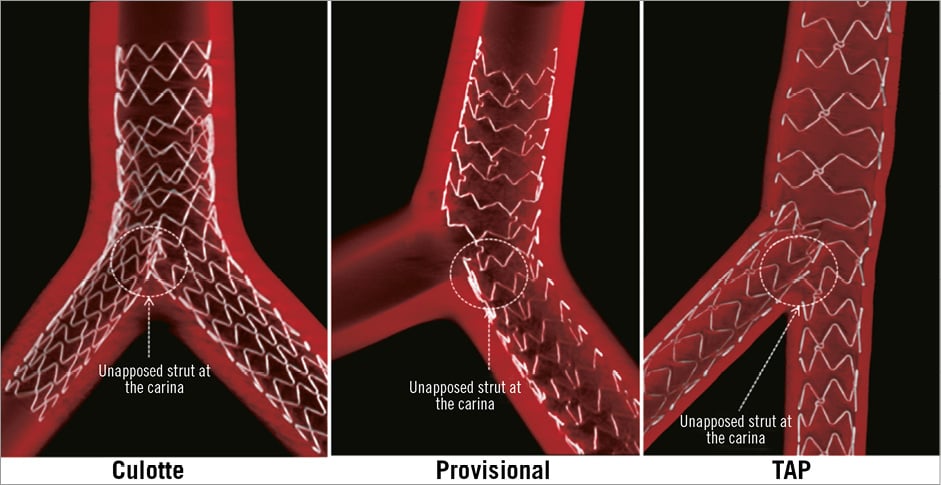
Online Figure 2. Culotte, provisional, and T-stenting and minimal protrusion (TAP) techniques. All techniques can leave a layer of struts unapposed in the main lumen in front of the carina (circle) (adapted from Foin et al19).
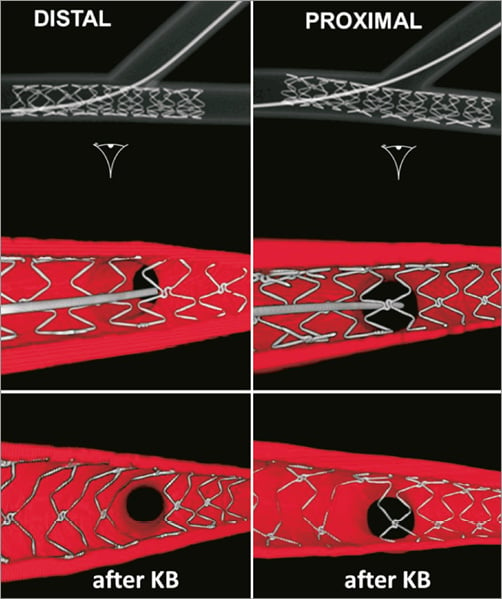
Online Figure 3. Impact of cell crossing location in stent optimisation. Comparison of SB access with distal versus proximal re-crossing (modified from Alegria-Barrero et al26).

