Abstract
Aims: High rates of restenosis and stent thrombosis are still often observed after bifurcation stenting despite the recommended stent post-dilatation using the kissing balloon (KB) technique. We investigated the potential benefits of a final post-dilatation step in bifurcation stenting with a balloon that respects the natural diameter ratio of the proximal and distal vessels in bifurcations (Murray’s law).
Methods and results: Fourteen commercially available stents (Xience V, Taxus Liberté and Presillion) were deployed in a silicone model of a coronary bifurcation using a provisional stenting approach. After side branch (SB) ostium dilatation and KB inflation, stent geometry and strut apposition was analysed using micro-CT. A final proximal inflation step was then performed to post-dilate only the proximal segment of the main vessel (MV). KB inflation produces an asymmetrical dilatation of the stent in the proximal part of the bifurcation with a number of struts left malapposed in the MV. Using the proposed final proximal inflation (FPI) step reduces the average stent eccentricity index from 0.72 to 0.90 (p<0.001) and the percentage of malapposed struts in the proximal part of the MV from 33.4% to 0.6% (p=0.02), while increasing the minimum stent area from 6.8 mm2 to 8.5 mm2 (p < 0.0001).
Conclusions: A final dilatation of the stent only in the MV proximal to the SB with a balloon sized according to the mother vessel is suggested to prevent stent malapposition and optimise stent deployment in bifurcation stenting.
Introduction
Bifurcations have represented a challenge since the early days of coronary interventions as they are common sites for lesions, and stenting at these locations can be problematic1,2. Several techniques were designed for treating bifurcations but recent trials suggest that more complex techniques offer no improvement over simple techniques and, when applicable and successful, a provisional technique with only one stent should be the preferred strategy3,4.
Final kissing balloon (KB) post-dilatation is often performed when stenting bifurcations, to prevent stent struts covering the side branch (SB) ostium, correct the ostial narrowing of the main branch (MB), and post-dilate the main vessel proximal to the SB. However, a recent randomised study in bifurcations treated with the provisional approach is challenging this practice by showing no improvements of routine KB post-dilatation on patient outcomes (NORDIC bifurcation study III)5.
Based on in vivo clinical observations by optical coherence tomography6,7, we hypothesised that KB post-dilatation of stents in bifurcations can produce significant stent distortion and may fail to ensure circular expansion and full apposition of the stent struts in the MV.
This study investigates, in a silicone model and using micro-CT, the effect of a final proximal post-dilatation with a balloon size taking into account the diameter change of the vessels in the bifurcation (Murray’s law) to optimise stent geometry and strut apposition in bifurcation stenting.
Material and methods
Model and stents
Commercially available 3.0 mm diameter coronary stents were deployed in a bifurcation silicone model mimicking the anatomy of a coronary bifurcation (proximal part of the MV=3.5 mm, distal MV=2.5 mm, SB=2.5 mm, MV/SB angle=45 degrees) using a provisional approach (Figure 1).
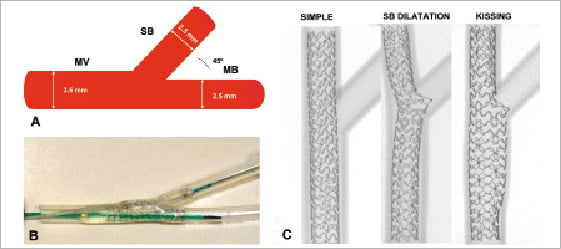
Figure 1. A) Dimension of the bifurcation model. Diameters and angles are representative of coronary anatomy. B) Silicone model with a deployed 3.0 Xience stent and simultaneous kissing with a 3.0 balloon in the MB and a 2.5 balloon in the SB inflated at 10 atm. C) Representative planar micrograph of provisional stenting technique with main branch stent deployment, SB opening and final kissing balloon inflation.
The stents used for this study (n=14) were 18 to 28 mm in length and included the polymer coated everolimus-eluting stents Xience V (n=5, Abbott Vascular, Santa Clara, CA, USA), the paclitaxel-eluting Taxus Liberte (n=5, Boston Scientific, Natick, MA, USA) and the bare metal CoCr Presillion stent (n=4, Cordis, Johnson & Johnson, Warren, NJ, USA). After the stents were deployed in the MV at nominal pressure, a guidewire was advanced under direct visual inspection into the SB through the most distal stent cell of the SB ostium. The side branch was then dilated using a 2-step kissing balloon post dilatation as previously described8. A non-compliant (NC) balloon (2.5×15 mm, NC Sprinter; Medtronic, Santa Rosa, CA, USA) was inflated at nominal pressure (10 atm) in the side branch; then KB inflation was performed with the 2.5 NC balloon in the SB and the 3.0 balloon in the MV simultaneously inflated at 10 atm for 20 seconds, and then deflated and removed. Thereafter, the stents were scanned by micro-CT. A final proximal optimisation step was then performed using a NC balloon (3.75×15 mm, Mercury; Abbott Vascular, Santa Clara, CA, USA) to optimise the stent/artery diameter ratio in the mother vessel, proximal to the bifurcation. The balloon was positioned before the bifurcation to post-dilate only the proximal part of the stent, taking into consideration the natural change in diameter in the bifurcation between the proximal and the distal part of the MV (Figure 2).
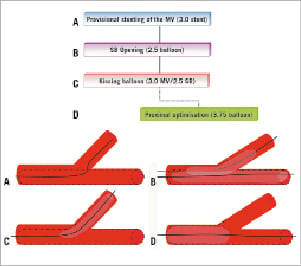
Figure 2. Flow chart of the deployment in the bifurcation. After deployment of the 3.0 stent in the MV at nominal pressure (A), the SB was dilated (B) with a 2.5 balloon and kissing balloon inflation performed with a 3.0 balloon in the MV and the 2.5 balloon in the SB simultaneously inflated at 10 atm (C). To optimise stent apposition, a final proximal post dilatation was performed on the stent only in the proximal part of the MV (distal marker of the balloon positioned at the bifurcation) with an oversized (3.75) NC balloon. Stents were scanned after each dilatation step.
Micro-CT
The models were scanned at each step of deployment using micro computed tomography (HMX-ST CT, X-TEK Systems Ltd, UK, courtesy NHM London) with a voxel resolution of 5 microns.
The stents were scanned after each step (n=56) and the results processed to extract quantitative measurements including minimum lumen diameter, minimum stent area,% of malapposed struts in different cross-sections along the MV (10 mm proximal to the bifurcation, 5 mm proximal to the bifurcation, through the bifurcation, immediately distal to the bifurcation and 5 mm distal to the bifurcation).
For three-dimensional (3D) reconstruction and longitudinal sectioning, the model and the stent were segmented using image processing software (ImageJ, rsbweb.nih.gov). The models could be virtually cut open longitudinally to allow visualisation of the stent struts apposition. Ostial area stenosis was measured from the 3D reconstruction using an appropriate planar projection. Using a 3D reconstruction of the side-branch ostium, the percentage of area of ostial area stenosis was calculated as follows: total ostium area – largest opened cell area/total ostium area×1008. All measurements were repeated at least twice and an average of the repeated measurements was used.
Statistical analysis
Results are expressed as mean±SD. Apposition and geometry of the stent after KB inflation only and after final proximal optimisation were tested by analysis of the variance. Results were considered statistically significant when p<0.05.
Results
Side branch dilatation
SB dilatation through the stent struts (distal cell) with a 2.5 mm balloon at 10 atm considerably improved the result at the SB ostium, compared to MB stenting alone. Ostial area stenosis defined as the area covered by struts outside of the largest open stent cell (cf. methods) was reduced from 68.7±8.4% without SB opening (“keep simple”) to 25.3±9.8% after SB dilatation (p<0.0001).
SB dilatation however, produced a significant detrimental distortion of the stent with a compression in the MV at the MB ostium distal to the SB (Figure 4 B). The minimum lumen diameter (MLD) in the MB at the level of the ostium was reduced from 2.7±0.1 mm before SB dilatation to 2.1±0.3 mm after (p<0.0001) (Table 1).
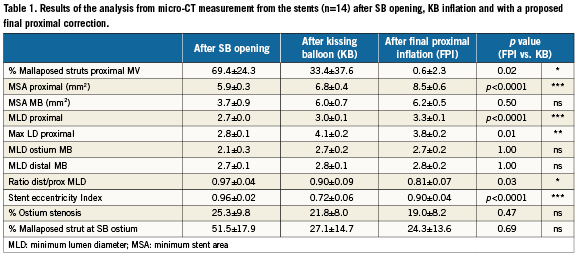
A large number of struts (69.4±24.3%) remained malapposed in the proximal part of MV due to a mismatch between the stent diameter and the diameter of proximal MV (Figure 3 and Figure 4 B).
The percentage of struts malapposed remained high also in the bifurcation (51.5±17.9%) with a large number of malapposed struts opposite the SB ostium (Figure 4 B).
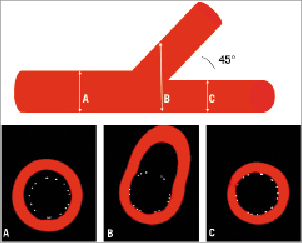
Figure 3. Stent apposition just after deployment at nominal pressure (8 atm) of a 23 mm long 3.0 Xience V stent in the MV. The stent struts remain malapposed in the proximal part of the bifurcation (A) as well as at the side branch ostium (B). On the other hand complete strut coverage is observed in the distal part of the MB (C).
Kissing balloon
Application of simultaneous KB inflation restored the stent geometry at the MB ostium just distal to the SB (MLD at the MB carina after KB: 2.7±0.2 mm).
At the level of the ostium, final KB produces a small increase in ostium area compared to SB dilatation only: ostial stenosis was reduced from 25.3% after SB dilatation only to 21.8% after KB (p=0.41).
KB inflation also increased the minimum stent area measured 5 mm proximal to the bifurcation from 5.9±0.3 mm2 to 6.8±0.4 mm2 post KB (p<0.0001). KB resulted in better strut apposition both in the bifurcation from 51.5±17.9% after SB dilatation to 27.1±14.7% after KB, as well as in the proximal MV from 69.4±24.3% to 33.4±37.6% after KB (Table 1).
The effect of kissing was limited however to the regions where the two balloons overlapped (Figure 4 C, arrow).
Overlapping balloons simultaneously inflated in the MV proximal to the bifurcation produced a significant asymmetric over-expansion of the stents (5 mm proximal to the bifurcation after KB: average maximal LD 4.1±0.2 mm, average minimal LD: 3.0±0.1 mm and stent eccentricity index: 0.72±0.06) (Table 1).
Final proximal inflation
Final proximal inflation (FPI) was performed at 10 atm with a balloon (3.75×15) sized and positioned to dilate only the part of the stent in the MV before the MB ostium (distal marker at the level of the SB). Final proximal inflation reduced the stent asymmetry caused by KB from an SEI of 0.72±0.06 after KB to 0.90±0.04 after FPI (p<0.0001), while achieving a larger MSA in the proximal MV (from 6.8±0.4 mm2 after KB to 8.5±0.6 mm2 after FPI, p<0.0001) (Figures 4 C and 4 D).
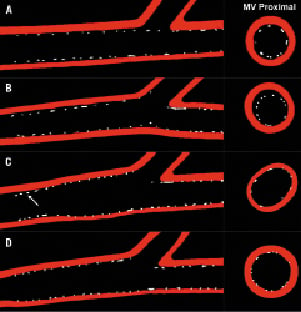
Figure 4. Effect of provisional approach and kissing inflation on strut distribution. Strut malapposition and stent underexpansion during stenting of the MV (A) and dilatation of the SB (B). Longitudinal and cross-sectional views show the asymmetrical distortion of the stent in the proximal MV after KB inflation (C). Final Proximal Inflation (FPI) with a post-dilatation of the proximal part of the MV corrects for the stent distortion induced after KB while ensuring complete apposition of stent struts (D).
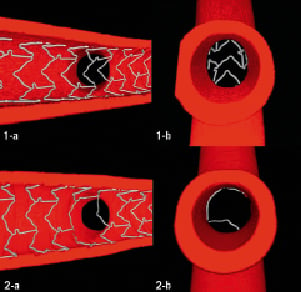
Figure 5. 1-a: Covering struts at the SB ostium of the bifurcation phantom after MV stenting using a Xience 3.0 stent, deployed at nominal pressure without SB dilatation. 1-b: View of the ostium from the SB 2-a: Kissing balloon inflation with a 3.0 balloon in the MV and a 2.5 balloon in the SB results in less struts covering the SB ostium. The final proximal correction prevents malapposed struts in the proximal MV 2-b: View of the ostium from the SB
Ostial opening was not affected by the final proximal inflation (Table 1) but this post-dilatation prevented almost complete strut malapposition in the proximal MV (33.4±37.6% after KB reduced to 0.6±2.3% after FPI, p=0.02).
Discussion
In this study we used a bench silicone phantom and micro-CT to determine if simultaneous KB inflation improves stent results, and if it should be used as the final step when performing bifurcation stenting. We investigated the benefits of using a final proximal inflation step after KB only in the proximal part of the MV.
Stent expansion and apposition
Previous studies based on bench investigation of stent in bifurcations9,10 reported the distortion of the MV stent immediately after SB dilatation. Based on these results, a systematic use of final kissing inflation has been recommended when performing stenting of bifurcations, including in provisional approach.
Where the two balloons overlap during kissing inflation, the added nominal diameter of the two balloons is 2.5+3.0=5.5 mm, well above the proximal artery diameter (3.5 mm). This produces an asymmetric expansion of the stent in the proximal MB. In addition, there is almost no control during KB inflation of the axis of where the balloons overlap and cause the stent oval deformation.
Early bench studies based on rigid models may have underestimated some of the detrimental effects of overlapping balloons on stent geometry9,10.
Stent asymmetric deployment has been previously reported in vitro11 as well as in vivo using intravascular ultrasound12 and optical coherence tomography (OCT)13. Animal studies show stent over stretch can produce higher injury to the vessel wall, increasing inflammatory and neointimal response.14,15 In a recent OCT study, stent asymmetry (quantified by the SEI: stent eccentricity index) has been correlated in DES with stent thrombosis and higher risk of major adverse outcomes13.
A final kissing inflation is generally recommended to prevent strut malapposition and optimise stent deployment in bifurcation stenting. Evaluation post stenting by optical coherence tomography (OCT) show that the risk of malapposed struts is significantly higher in bifurcation7,16. Recent pathological evidence suggests also that malapposed struts may significantly increase the risk of restenosis and stent thrombosis17-20.
Here, we show that KB is not sufficient to prevent strut malapposition, even in the simple single stent provisional approach. Current practice suggests placing both balloons so they overlap in the MB during kissing. The impact of the KB dilatation on the final apposition and geometry of the stent is dependent on the position and diameter of both balloons during the kiss (Figures 2 and 4). A SB balloon positioned along the entire length of the proximal MV may produce an extensive asymmetric distortion of the stent, with a potential risk of arterial injury in the MV. Conversely, a balloon inserted too distal in the SB will leave some malapposed struts in the MV proximal to the bifurcation, and may increase the risk of SB dissection.
Moreover, here we show that the application of a final proximal post-dilatation step, not only corrects for the asymmetric deployment of the stent associated with the final KB technique, but also prevents strut malapposition –all of which may improve the long-term outcome of PCI in bifurcations. Although this study focused on KB with provisional stenting, the same findings are expected for KB in bifurcation strategies using two stents.
Importance of opening the SB ostium
Recent evidence suggests, for a lesion localised mainly in the MV, stenting of both the MV and SB with two stents does not produce any clinical benefit compared to only stenting the MV21-23. Nowadays, provisional stenting with only one stent deployed in the MV is the preferred default approach in bifurcations1,22,23.
Deployment of only one stent in the MV without considering opening the SB is, however, limited by the risk of compromising the flow to the SB. Evidence suggests that the SB flow is mainly affected by carina displacement during intervention and a focal high rate of restenosis at the SB ostium, caused by incomplete scaffolding and struts jailing the SB ostium1,17,24,25.
Final KB inflation is generally recommended to open struts at the SB ostium and thereby prevent SB re-occlusion1,10. The benefits of the KB technique has been clearly demonstrated for two stents strategies26, but it is still unclear from recent trials whether final KB inflation is beneficial in provisional stenting technique with only one stent4,5. A trade-off between the benefits of opening the SB and the detrimental effect caused by the overlapping balloons distorting the stent in the MV might explain the recent findings from randomised trials with the provisional one stent technique, suggesting there is no difference in early clinical outcome between using final KB versus leaving the SB jailed4,5.
As anticipated from previous studies8, we observed a slight increase in the SB ostium opening between the approach of SB dilatation only and the KB. The difference was however not significant. On the other hand, significant differences were observed between stent designs in terms of ostium opening and percent malapposition. The aim of this study was however to provide general principles on post-dilatation techniques rather than comparing stent platforms. Previous work using computational models have reported the importance of the stent design for opening the SB ostium27,28.
Murray’s law
Murray’s law, based on the principle of minimum work, suggests that arterial calibres follow a systematic law that determines the ratio between vessel diameters in bifurcations29. Based on extensive in vivo measurements on 173 coronary bifurcations angiograms, Finet showed Murray’s law can be approximated by a simpler linear relationship with a ratio of ~ 0.68 relating the diameter of the mother vessel to the sum of the two daughter vessel diameters30. (When the two daughter branches are equally sized, this relationship is equivalent to MV ≈ 1.36×MB). Current approaches for stenting bifurcations consider too rarely the large change in diameter of the MB branch through the bifurcation. The changes in diameter in our model mimicked in vivo conditions (ratio of the distal/proximal LD was equal to 2.5/3.5=0.71).
According to the approximation of Murray’s law by Finet30, given the diameter of the daughter vessels, the proximal MV should be 0.68×(2.5+2.5)=3.4 mm. The choice for the balloon diameter for the final proximal inflation (3.75 mm) was motivated by the aim to apply a recommended stent to artery ratio ~1.1 in the proximal MV.
Without a final proximal inflation, the proximal part of the deployed stent may remain incompletely apposed. Distal/proximal stent MLD ratio was 0.90 after KB. (Table 1 and Figure 4 A and B)
The proposed final proximal inflation takes into account the natural change in diameter of the MV through the bifurcation as only the proximal part of the stent in the MV is dilated. After a final proximal (FPI) post-dilatation, the average diameter of the stent 10 mm proximal to the bifurcation was 3.3 mm compared to a distal diameter of 2.8 mm leading to a distal/proximal stent diameter ratio of 0.81±0.07. (Figure 4 D)
Study limitation
Silicone models can only provide an approximation of the in vivo behaviour of the stent-artery response during stent deployment. Although the geometry used here was representative of a coronary bifurcation, the results must be carefully interpreted as different vessel geometries and side branch angle may produce different results.
Our model was not constrained by surrounding tissue and mimicked a lesion free vessel. Stenosis may affect not only lumen and wall geometry but also local arterial mechanical properties. In particular, calcified lesions have been reported to increase by several fold the local arterial stiffness (Young’s modulus)31. KB inflation in stiffer vessels may result in less eccentric distortion of the stent than was observed in our model. This study underlines the risk of incomplete stent deployment proximal to the MV and the detrimental effect of final kissing inflation of stent geometrical results.
The suggestion of a final proximal post-dilatation step is yet based only on the result of this in vitro study. Nevertheless, preliminary observation using optical coherence tomography shows a similar pattern in vivo (Figures 6 and 7). Further in vivo results are needed to determine the benefit of such final proximal post-dilatation for improving patient outcomes.
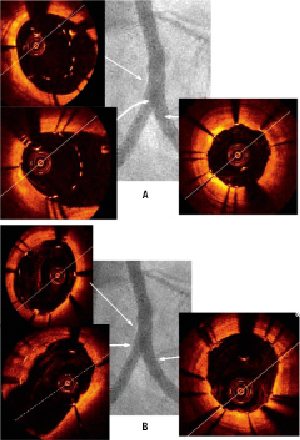
Figure 6. A: Intravascular optical coherence tomography pullback in a left circumflex (LCx) stented with a 2.5 everolimus-eluting stent before SB opening showing the mismatch in the proximal MV between the stent and lumen diameter. B: Kissing balloon inflation with a 3.0 mm (MV) and 3.0 mm (SB) balloon improves SB ostium opening but can produce a significant eccentricity of the stent (oval shape) with a risk of malapposed struts in the proximal MV.
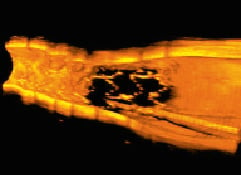
Figure 7. 3D reconstruction from optical coherence tomography pullback in the LCx of figure 6A showing the side branch ostium jailed by the MV stent.
Conclusion
Final kissing inflation, often used as a post-dilatation step in bifurcation stenting, produces sub-optimal stent geometry and does not ensure complete apposition of the struts at the SB ostium and in the proximal part of the bifurcation.
Our results suggest that performing a final proximal post-dilatation to the stent after kissing-balloon inflation can restore a circular stent geometry and ensure complete stent deployment in the MV.
Conflict of interest statement
The authors have no conflicts of interest to declare.