Abstract
Aims: We aimed to review the technical characteristics of DES platforms which have been documented to influence bifurcation stenting procedures conducted according to the provisional approach.
Methods and results: DES platforms have remarkable technical differences (side cell diameter, shape, deformability, etc.). We reviewed the literature data and performed original virtual bench tests to highlight the characteristics of DES platforms which influence the following phases of bifurcation stenting conducted according to the provisional approach: stent implantation in the main vessel across side-branch take-off (“crossover” stenting), proximal optimisation technique, rewiring and kissing balloon inflation. Available data show that the response of different DES platforms to the various procedural steps of provisional stenting is different.
Conclusions: When treating bifurcated lesions according to the provisional stenting approach, the search for an ideal matching between individual bifurcated anatomy and DES selection should take into account an articulated series of technical parameters.
Introduction
Drug-eluting stent (DES) implantation according to the so-called “simple strategy” or “provisional stenting” technique represents the main approach for percutaneous coronary interventions (PCIs) on unselected bifurcated lesions1. Recently, five-year follow-up data from a randomised trial showed that the clinical outcomes after provisional stenting are at least equal to those of planned stenting of both the main vessel (MV) and the side branch (SB)2.
Coronary bifurcations have been recognised as complex arterial segments characterised by three different diameters (proximal MV, distal MV and SB) linked by geometrical relationships1. Thus, a stenting procedure over a coronary bifurcation inevitably implies the presence of floating stent struts jailing the SB ostium, and poses the problem of matching a single tubular stent size with two different vessel sizes (proximal and distal MV). Moreover, novel insights from clinical studies based on invasive imaging modalities have shown that stent implantation in the MV may cause deterioration of SB lumen due to the phenomenon of “carina shift”3-5. Thus, in daily clinical practice, DES platforms selected for “provisional stenting” and implanted in the MV across an SB (“crossover stenting”) are often required to be exposed to:
– proximal post-dilation according to the proximal optimisation technique (POT) (in order to fit with a larger proximal MV size)1;
– side cell dilation towards the SB according to the kissing balloon inflation (KBI) technique (in order to ensure or restore SB patency)1.
As an example of the steps of this technique, Figure 1 shows the sequence of crossover stenting, POT, distal rewiring and KBI in a patient with a complex, bifurcated lesion with major mismatch between proximal and distal MV size.
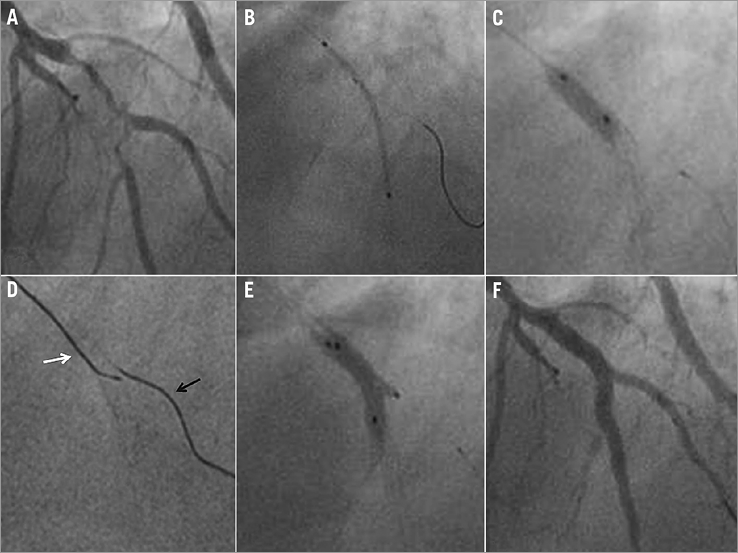
Figure 1. Clinical example of the provisional approach to treat a complex bifurcated lesion with major mismatch between proximal and distal MV size. A) Baseline angiography. B) “Crossover” stenting with jailed wire in the SB. C) POT. D) Distal SB rewiring according to the pullback technique (note the distance between the jailed wire, black arrow, and the tip of the rewiring guide, white arrow). E) Kissing balloon inflation. F) Final angiographic result.
Of note, available DES types from different manufacturers have technical characteristics which are often radically inhomogeneous. Such structural differences may theoretically change the response to similar interventional steps like ballooning inside the stent or across its side cells.
In the present paper, we review the data on the differences existing across the DES platforms which may play a role in the various steps of the “provisional stenting” technique. Moreover, since computer simulation is a recognised tool to improve knowledge in this field6, we report the results of original virtual bench tests of the provisional approach conducted with different DES platforms.
Main vessel stenting across side-branch take-off (“crossover stenting”)
The main step of “provisional stenting” is “crossover stenting”. Despite the inherent simplicity of crossover stenting, to obtain perfect matching between the stent and the MV by just delivering the stent with a single balloon inflation is almost impossible. Indeed, due to the different size of proximal and distal MV segments:
– if the stent size is selected according to the distal MV, the stent struts will not be apposed in the proximal MV segment (Figure 2A);
– if stent size is selected according to the proximal MV, the stent struts will induce vessel wall overstretching in the distal MV, thus increasing the risk of both carina shift and distal MV overstretch/dissection (Figure 2B).
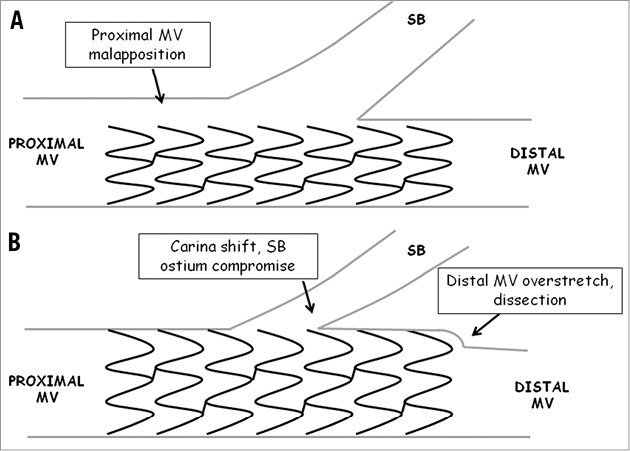
Figure 2. Theoretical impact of MV stent sizing. A) Stent sizing (ratio 1:1) according to the MV distal segment. B) Stent sizing (ratio 1:1) according to the MV proximal segment.
Theoretically, differences in DES characteristics may change the response to crossover stent implantation. Figure 3 shows the pattern of stent-to-artery wall distance obtained by virtual simulation (performed according to a previously described methodology7) with four different DES implanted in the MV across the SB (sizing selected according to the distal MV, same inflation pressure). It is evident that all stent platforms have high degrees of stent-to-artery distance at the proximal MV. The relevance of this phenomenon has recently been confirmed by an optical coherence tomography study showing an increased frequency of malapposition at the level of the proximal MV during provisional stenting8. Besides the possible risk of stent thrombosis, malapposed stent struts may hinder the advancement of balloons (eventually needed for SB interventions or MV post-dilation) and may facilitate the occurrence of longitudinal stent deformation. Indeed, longitudinal compression usually occurs at the proximal stent edge, and bifurcation interventions have been found to be associated with this phenomenon9. Since longitudinal stent compression has been recognised to be highly influenced by stent design10-12, when dealing with a major mismatch between proximal and distal MV size, DES selection for crossover stenting should probably take into account the issue of possible stent deformation during the subsequent procedural steps.
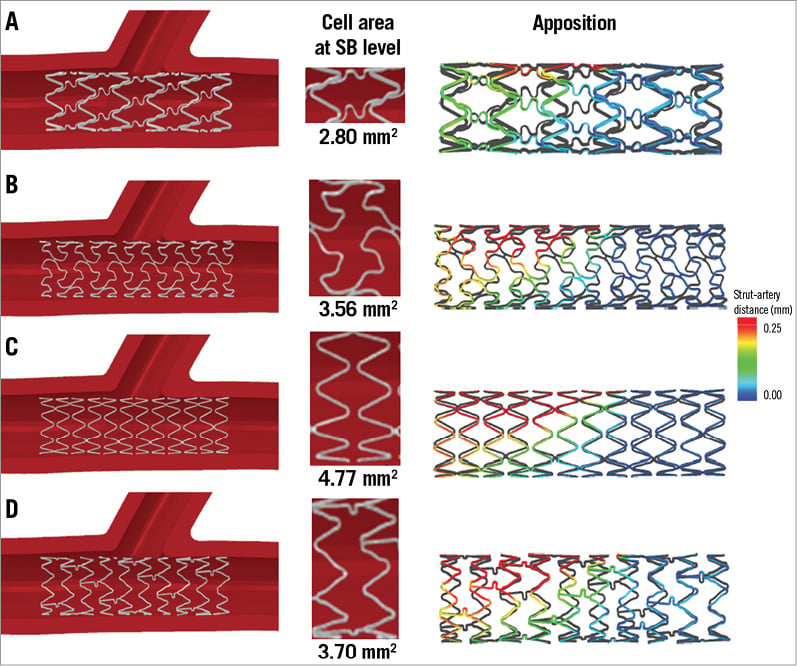
Figure 3. Virtual simulation and estimated strut to artery distance of “crossover stenting” performed with different DES platforms. The figure shows the three-dimensional aspect, the magnified side cell and the apposition analysis as obtained by virtual simulation. Virtual simulation conditions were: virtual modelling of silicon phantom of coronary bifurcation (tube lumen diameters: 4 mm proximal MV, 3.5 mm distal MV, 2.5 mm SB); implantation in the MV of 3.5 mm×18 mm DES (Panel A: CYPHER®; Cordis, Johnson & Johnson, Warren, NJ, USA; Panel B: TAXUS® Liberté®; Boston Scientific, Natick, MA, USA; Panel C: Endeavor Resolute; Medtronic, Minneapolis, MN, USA; Panel D: XIENCE V®; Abbott Vascular, Santa Clara, CA, USA) at 12 atmospheres. Apposition analysis was performed by measuring the distance between stent struts and vessel wall (distance range colour scale provided alongside).
Another relevant anatomic issue is represented by the complex spatial geometric aspect of coronary bifurcations. Variable angulations exist not only between the MV and the SB axis but also along the MV axis (as measured by the angle between proximal and distal MV, usually called angle “γ”). DES are known to change the three-dimensional geometry of coronary vessels by straightening curved segments13,14. When dealing with bifurcations, the geometrical modification induced by stenting procedures is known to be lower after single compared with double stenting techniques15, and major deformation has been reported to be associated with worse clinical outcome16. Notably, as a consequence of heterogeneity in design and physical properties, different DES platforms may induce different modifications to angled vessels17.
Proximal main vessel optimisation by post-dilation (POT)
To overcome most of the limitations mentioned in the previous paragraph, the POT technique has been proposed (Darremont, oral communication at 4th European Bifurcation Club meeting) and consists in the post-dilation of the proximal part (up to the carina level) of the MV stent with a short balloon. The adoption of this technique after selection of MV stent size according to the distal MV has been recommended1 in order to limit carina shift, distal edge dissections and proximal malapposition. Figure 4 shows the appearance after virtual simulation of POT with four different DES together with the apposition analysis, showing that all DES types exhibit a marked reduction in strut malapposition at the proximal MV after POT. Nevertheless, despite such an overall similar behaviour, careful analysis of some parameters may disclose the existence of remarkable differences in the response to POT across various DES platforms. Indeed, in response to the oversized post-dilation necessary for the POT technique, different DES have been recognised to have:
– different degrees of maximal dilation,
– different degrees and pattern of side cell enlargement.
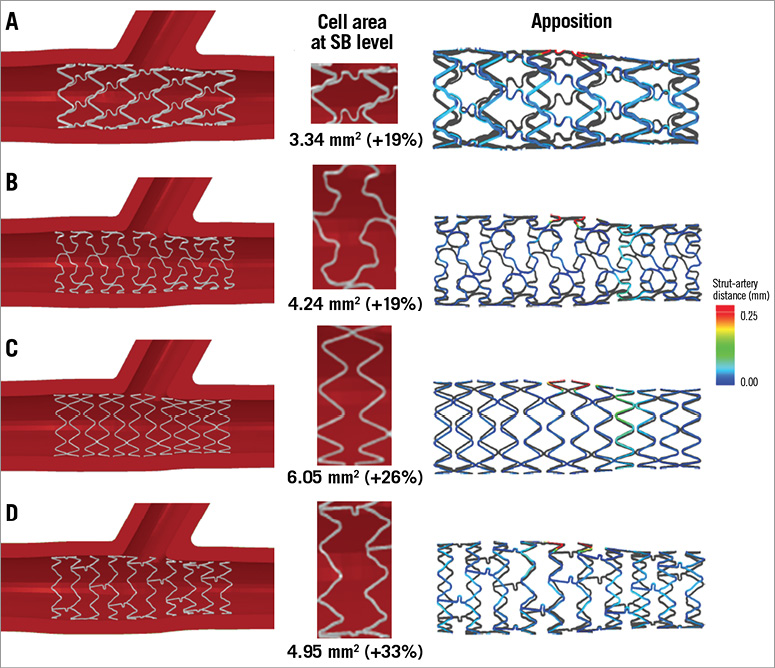
Figure 4. Virtual simulation and estimated strut to artery distance after POT performed with different DES platforms. The figure shows the three-dimensional aspect, the magnified side cell and the apposition analysis as obtained by virtual simulation. Virtual simulation conditions are described in the Figure3 legend. Implantation in the MV of 3.5 mm×18 mm DES (Panel A: CYPHER®; Cordis; Panel B: TAXUS® Liberté®; Boston Scientific; Panel C: Endeavor Resolute; Medtronic; Panel D: XIENCE V®; Abbott Vascular) at 12 atmospheres followed by proximal post-dilation with a 4×12 mm semi-compliant balloon at 12 atmospheres. Side cell areas are provided for each DES together with the relative increase compared with cell area after simple crossover stenting (Figure3). Apposition analysis was performed by measuring the distance between stent struts and vessel wall (distance range colour scale provided alongside).
Two studies based on bench testing followed by micro-computed tomography investigated the issue of maximal DES dilation and clearly found a difference across stent expansion achieved with different DES after dilation with oversized balloons18,19. In the first study, Basalus et al post-dilated with non-compliant 5.0 mm balloons the proximal part of 3.5 mm diameter DES from five manufacturers18. In the second study, Foin et al post-dilated with non-compliant 4.0, 5.0 mm and with semi-compliant 6.0 mm balloons the proximal part of different workhorse designs of 6 DES types19. Both studies found that a similar (oversized) ballooning induces different final stent dilation in different DES platforms18,19. The issue of maximal diameter achievable by post-dilation may be relevant in the treatment of bifurcated lesions (especially those with major drop of vessel size across the SB take-off) since the chances of achieving correct stent apposition in the proximal MV may be highly dependent on DES selection. Furthermore, it is crucial to understand how each manufacturer combines different variants of a certain design (usually two or three) with a range of delivery balloon sizes. The other relevant aspect associated with DES post-dilation is represented by the modification of side cell shape and size. Generally, POT increases the size of side cells, but such an increase is different across various DES. In Figure 4, virtual simulation of MV post-dilation of four DES types shows that an increase in cell size area is always induced (thus supporting the concept that POT may facilitate access towards the jailed SB). However, the relative increase in side cell area is different and results in completely different shapes and areas of side cells across different DES (Figure 4). Of note, among different DES platforms, not only the size but also the pattern of side cell opening induced by post-dilation may be different. Indeed, as reported by Basalus et al18, POT induces a specific modification of stent geometry which may be summarised by three different stent segments: 1) the post-dilated region, 2) the “transitional region” (in which the stent diameter shows a gradual decline), and 3) the non-post-dilated region (Figure 5). According to the pattern of side cell expansion in response to POT, two types of response may be categorised: 1) largest cells obtained in the transitional region, and 2) largest cells obtained in the post-dilated region18. Again, such different responses may have procedural relevance since:
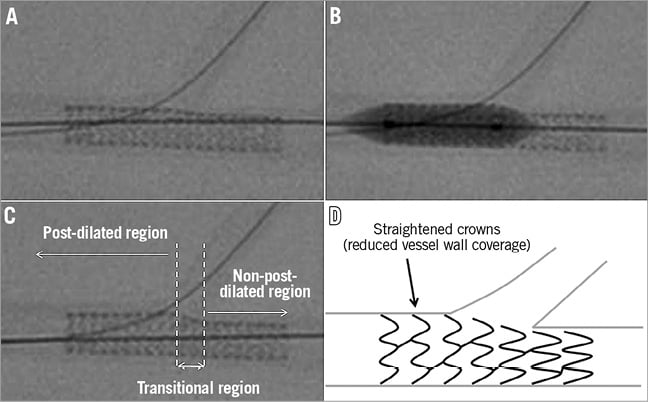
Figure 5. Change in DES structure induced by POT technique. A) Crossover stenting in a bench model of coronary bifurcation. B) POT technique with semi-compliant, short balloon. C) Aspect of DES after POT showing that POT induces a three-segment modification in DES. D) A schematic representation allowing appraisal that POT-induced enlargement of DES is mediated by straightening of stent crowns.
1) DES with first type of response may be associated with SB access facilitation;
2) the POT balloon positioning is relevant for SB access facilitation.
Finally, within the post-dilated region, inhomogeneity in the distribution of stent strut vessel coverage may be induced by POT. Since the mechanism of stent enlargement is mainly represented by stent crowns straightening, a possible measure of this phenomenon is represented by stent crown angle reduction, a parameter which has been found to differ among various DES19. Possible consequences of stent crown overstretching are the creation of variable gaps between struts, resulting in impaired vessel wall scaffolding and inhomogeneous drug elution20.
Moving to the clinical ground, the different side cell shape and size (both after nominal expansion and after POT) achieved with different DES platforms may influence the management of SBs during PCI. In a recent clinical study, significant differences between DES were observed in the occurrence, after MV stenting, of SB TIMI flow <3 or the need for specific wires for SB rewiring, or failure to re-wire/dilate the SB21.
Kissing balloon inflation
Kissing balloon inflation represents a pivotal step of the provisional approach22. Although no clinical evidence supports the routine adoption of kissing balloon inflation, its use in patients undergoing the “provisional technique” has been recognised to:
– improve the SB FFR in the case of a suboptimal result after MV stenting23,
– improve the SB acute angiographic24 and physiological result25,
– reduce post-procedural inducible ischaemia26,
– reduce the angiographic SB stenosis in the angiographic follow-up24.
It should be recognised that the response of various DES platforms to side cell ballooning is highly variable due to a series of differences in stent structural characteristics.
Historically, a stent’s side cell dilatability in response to balloon inflation has been the first parameter recognised as a main determinant of a stent’s suitability for bifurcation interventions. The first evidence was collected by Ormiston et al27 and by Kinoshita et al28 who independently set up bench tests comparing the side cell enlargement induced by side cell dilation in different stent platforms. Both studies highlighted a main pitfall of side cell dilation: the induction of MV stent deformation causing residual stenosis at the level of the distal MV. These studies also suggested that the performance of final kissing inflation may allow such adverse distal MV stent distortion to be limited. More recently, a virtual simulation study testing contemporary DES platforms29 has reported similar findings. Indeed, after MV stenting, SB ballooning induced an enlargement of side cells, something which is dependent on stent design and which (in the absence of kissing ballooning) may compromise the downstream MV lumen29. Interestingly, the relevance of side cell dilatability is highly dependent on the specific bifurcation geometry. This issue has been assessed in a micro-computed tomography study assessing the impact of SB size and SB take-off angle on SB ostium size30. In this study, larger SBs with acute take-off angles have been found to be associated with larger, oval shaped SB ostia which may easily exceed the theoretical expandability of the side cells of some, but not all, tested DES30. Of note, the different dilatability of side cells may have an influence on the final SB opening. Indeed, in a recent trial on patients with bifurcated lesions undergoing provisional stenting with POT and eventual kissing balloon inflation, the (three-dimensional) angiographic results at the level of the SB ostium were significantly different according to DES type31.
As shown in Figure 6, kissing balloon inflation (MV and SB balloons selected according, 1:1, to the distal MV and SB), performed after POT and distal rewiring with four DES types, may result in variable SB openings and prevent distal MV lumen compromise. Of note, the deformations of a particular stent design obtained after kissing balloon inflations can be highly variable depending on the relative position of the stent with respect to the SB ostium, as shown by Gastaldi et al32.
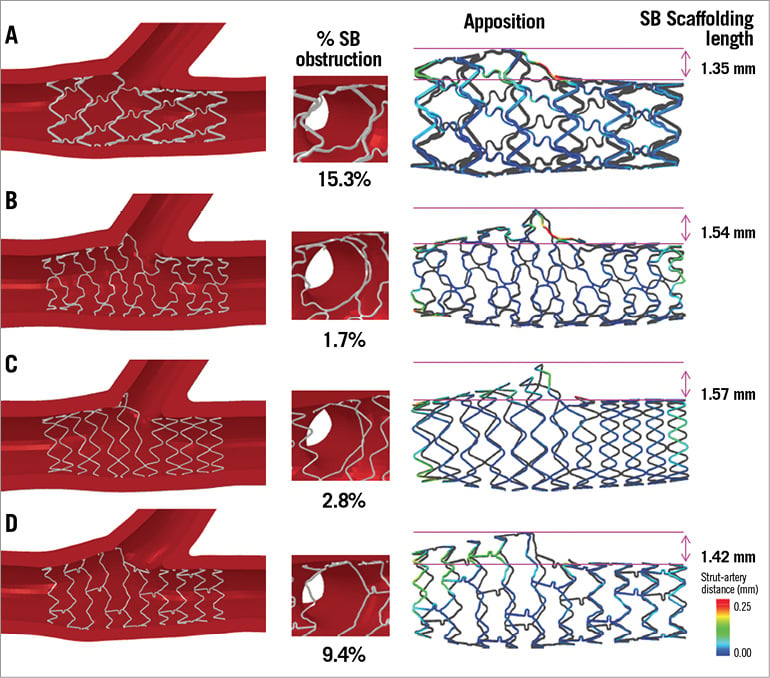
Figure 6. Virtual simulation and estimated strut to artery distance after kissing balloon performed with four different DES platforms. The figure shows the three-dimensional aspect, the magnified side cell, the apposition analysis and SB scaffolding length measure as obtained by virtual simulation. Virtual simulation conditions are described in the Figure3 legend. Implantation in the MV of 3.5 mm×18 mm DES (Panel A: CYPHER®; Cordis; Panel B: TAXUS® Liberté®; Boston Scientific; Panel C: Endeavor Resolute; Medtronic; Panel D: XIENCE V®; Abbott Vascular) at 12 atmospheres followed by proximal post-dilation with a 4×12 mm semi-compliant balloon at 12 atmospheres and by kissing balloon inflation using a 3.5×20 mm balloon in the MV and a 2.5×20 mm balloon in the SB at 12 atmospheres. Apposition analysis was performed by measuring the distance between stent struts and vessel wall (distance range colour scale provided alongside). Percentage (%) area of SB obstruction has been calculated as follows: (area of the ostium – area free of stent struts)/area of the ostium *100.
Besides the discussed side cell size issue, other, less investigated, technical characteristics of DES platforms may potentially influence the response to kissing balloon inflation.
Firstly, a distal site of side cell re-crossing with the guidewire before SB dilation (also called “rewiring”33) is emerging as an important determinant of enhanced stent strut removal from the SB ostium34. A pullback rewiring technique33 has been highlighted as the best practice to facilitate distal rewiring and (if available) optical coherence tomography with on-line three-dimensional reconstruction may allow the rewiring site to be checked34. Nevertheless, the possible relevance of DES design on the ease of distal rewiring is highlighted in Figure 7, which compares the hypothetical distribution of stent rings at the SB ostium obtained with an open or closed cell DES across the SB take-off (Figure 7, legend).
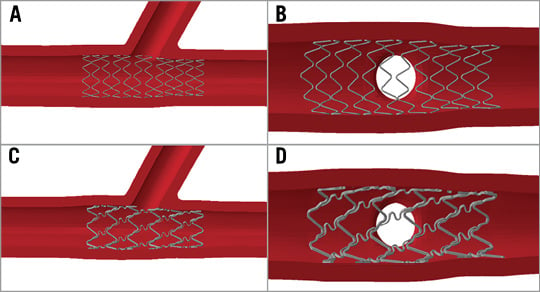
Figure 7. Impact of DES design on chances of performing distal rewiring. The figure shows virtual simulation of DES positioning at bifurcation level (left panels) together with corresponding distribution of stent struts at the SB ostium (right panels). The chances of side cell availability for distal re-crossing will be facilitated using a stent with open cell design and a high number of rings across the SB, as shown in panel A and panel B. On the contrary, when using a closed cell stent design with a low number of crowns across the SB ostium (panel C and panel D), the possibility of performing an effective distal rewiring will depend on the relative position of the stent with respect to the SB ostium (which cannot be controlled during interventions).
Secondly, a potential favourable effect of kissing balloon inflation is represented by the possibility of “scaffolding” the very proximal segment of the SB with the displaced MV stent struts. This phenomenon is clearly dependent on the “distality” of side cell re-crossing but may be limited by the maximal dilatability of the MV stent which (as reported in the previous paragraph) is highly variable across different DES. A possible way to quantify the different SB scaffolding efficacy of different DES is the “SB scaffolding length” (defined as the difference between maximal stent diameter at the bifurcation level and stent diameter in the distal MV) which may be assessed by angiographic images (especially using the recently available stent enhancement tools35). As shown in Figure 6, this parameter has been found to differ across four DES platforms as assessed by virtual simulation. Of note, this parameter cannot be considered univocal since it may be influenced by the vessel geometry36, by the relative position of the stent with respect to the SB ostium, and by the specific technical environment (balloon selection, inflation technique, etc.).
On the basis of such issues, kissing balloon inflation should be regarded as a technique with no univocal result, since its final impact on stent strut distribution at bifurcations has been recognised to be dependent on a series of technical factors.
Limitations
The issues discussed in the present work are mainly based on (published or original) data from bench tests and computer simulations. Both sources have relevant limitations since only a minority of DES platforms and techniques have been explored and some data have been collected using DES which are no longer available.
The results of the original virtual bench tests have to be considered as illustrative only, since a single case for each stent platform has been simulated.
Conclusions
A series of technical characteristics renders the response of different DES to the various steps of the provisional stenting technique highly variable. When treating bifurcated lesions with provisional stenting, the search for an ideal matching between individual bifurcated anatomy and DES selection should take into account an articulated series of technical parameters. Unfortunately, most of these technical parameters are not routinely provided by the DES manufacturers.
| Impact on daily practice The recommended way to manage unselected bifurcations is the provisional approach. This technique, besides its simplicity, is associated with the inherent imperfection of trying to adapt a tubular stent to a bifurcated vessel. Bench tests and computational simulations have consistently shown that various DES platforms, due to different technical characteristics, have different responses to similar procedural steps like crossover stenting, POT and kissing balloon inflation. In particular, stent apposition to the MV, easiness of SB rewiring, SB opening and scaffolding are influenced by an articulated series of DES characteristics. These concepts may help interventionalists to select the appropriate DES and technique to treat individual patients with bifurcated lesions. |
Conflict of interest statement
F. Burzotta reports having been involved in advisory board meetings for Medtronic. P. Mortier is a shareholder of FEops, an engineering consultancy spin-off from Ghent University, and has served as a consultant for several medical device companies. C. Trani has no conflicts of interest to declare.

