Abstract
Aims: The rePOT (proximal optimisation technique) sequence proved significantly more effective than final kissing balloon (FKB) with two drug-eluting stents (DES) in a bench test. We sought to validate efficacy experimentally in a large range of latest-generation DES.
Methods and results: On left main fractal coronary bifurcation bench models, five samples of each of the six main latest-generation DES (Coroflex ISAR, Orsiro, Promus PREMIER, Resolute Integrity, Ultimaster, XIENCE Xpedition) were implanted on rePOT (initial POT, side branch inflation, final POT). Proximal elliptical ratio, side branch obstruction (SBO), stent overstretch and strut malapposition were quantified on 2D and 3D OCT. Results were compared to FKB with Promus PREMIER. Whatever the design, rePOT maintained vessel circularity compared to FKB: elliptical ratio, 1.02±0.01 to 1.04±0.01 vs. 1.26±0.02 (p<0.05). Global strut malapposition was much lower: 2.6±1.4% to 0.1±0.2% vs. 40.4±8.4% for FKB (p<0.05). However, only Promus PREMIER and XIENCE Xpedition achieved significantly less SBO: respectively, 5.6±3.5% and 10.0±5.3% vs. 23.5±5.7% for FKB (p<0.05).
Conclusions: Platform design differences had little influence on the excellent results of rePOT versus FKB. RePOT optimised strut apposition without proximal elliptical deformation in the six main latest-generation DES. Thickness and design characteristics seemed relevant for optimising SBO.
Abbreviations
CoCr: cobalt-chromium
DES: drug-eluting stents
FKB: final kissing balloon
POT: proximal optimisation technique
PtCr: platinum-chromium
RePOT sequence: initial POT - SBI - final POT
SB: side branch
SBI: side branch inflation
SBO: side branch obstruction
Introduction
Provisional coronary bifurcation stenting should take account of vessel diameter differentials according to fractal geometry, and maintained side branch (SB) ostium opening. The final kissing balloon (FKB) technique failed to demonstrate benefit; a new sequence, rePOT1, without FKB, showed superiority over all FKB strategies in a fractal bifurcation bench test. RePOT provides almost perfect stent apposition and optimal SB ostium opening without the proximal elliptical deformation by overstretch induced by FKB. RePOT was validated on two latest-generation active stent models1. However, platform design may influence mechanical behaviour2-5, especially with iterative post-dilatation.
The present study assessed rePOT efficacy experimentally in six latest-generation drug-eluting stents (DES).
Methods
EXPERIMENTAL PROTOCOL
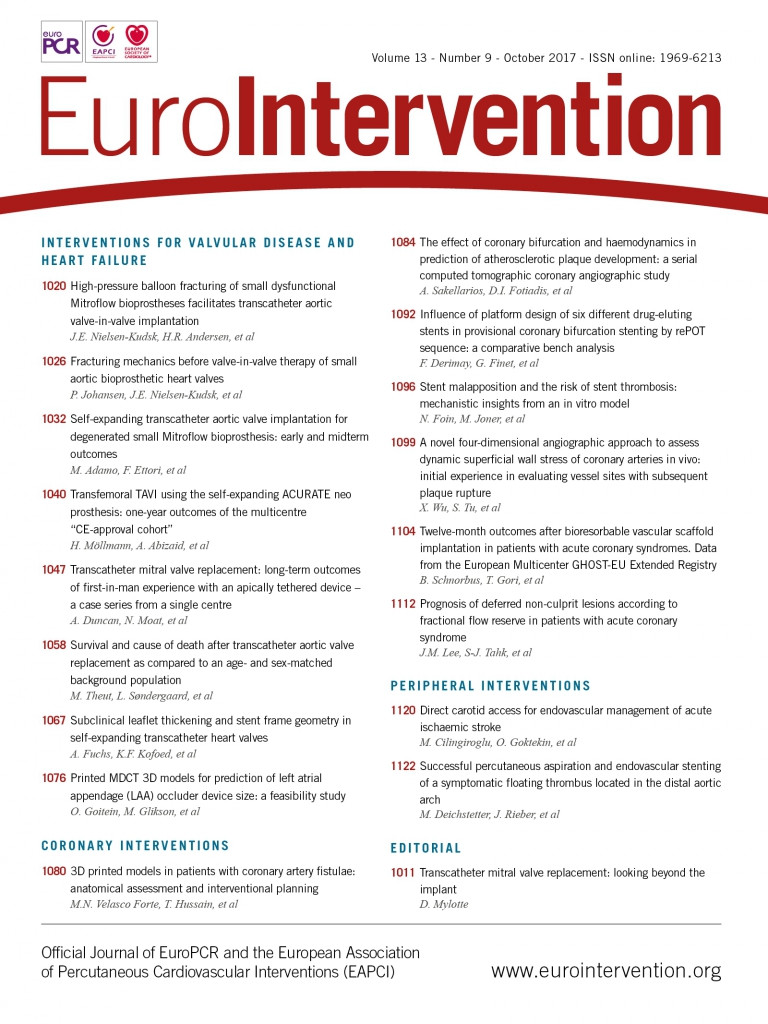
Five samples of each of the six latest-generation DES (Coroflex® ISAR [B. Braun Medical, Melsungen, Germany], Orsiro [Biotronik, Bülach, Switerland], Promus PREMIER™ [Boston Scientific, Marlborough, MA, USA], Resolute Integrity® [Medtronic, Minneapolis, MN, USA], Ultimaster® [Terumo Corp., Tokyo, Japan], XIENCE Xpedition [Abbott Vascular, Santa Clara, CA, USA] were implanted in previously described fractal coronary bifurcation bench models1 [Segula Technologies, Saint-Priest, France]) at 14 atm, adapted to main branch diameter, and the rePOT sequence was applied. Stent characteristics are shown in Figure 1.
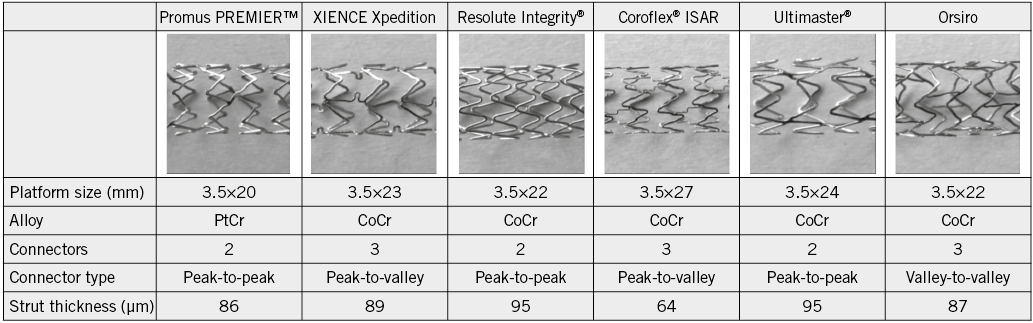
Figure 1. Main technical characteristics of the six latest-generation active stents. CoCr: cobalt-chromium; PtCr: platinum-chromium
RePOT, as previously described by Finet et al1, associates the initial proximal optimisation technique (POT)+side branch inflation (SBI)+final POT. All POTs used Maverick™ compliant balloons (Boston Scientific) (Figure 2).
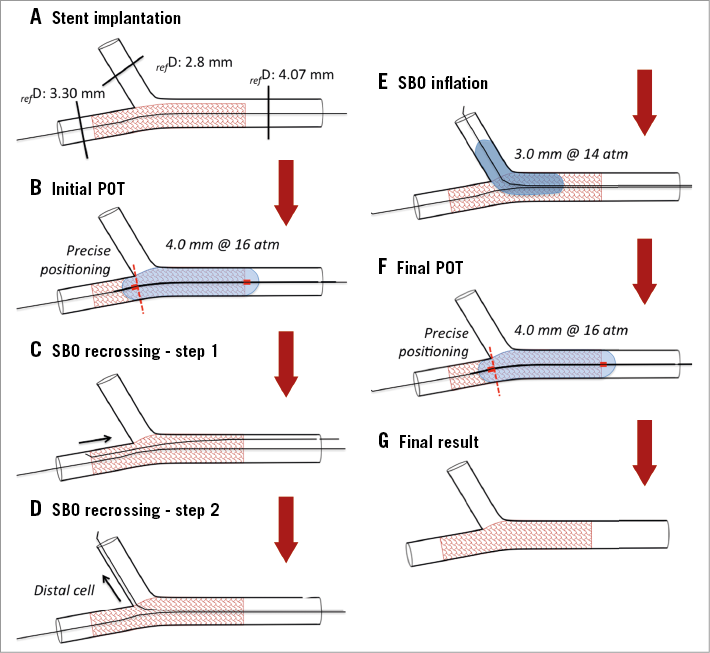
Figure 2. RePOT sequence kinematic. POT: proximal optimisation technique; SB: side branch; SBO: side branch obstruction. All post-dilatations were performed with a Maverick compliant balloon.
Each DES was compared to classic FKB results on five Promus PREMIER stents using two 3.5×15 mm and 3.0×15 mm non-compliant Emerge™ balloons at 12 atm (Boston Scientific).
2D- and 3D-OCT analysis used the Lunawave® OFDI system (Terumo Europe, Leuven, Belgium). 2D-OCT quantified elliptical ratio, side branch obstruction (SBO%), overstretch and strut malapposition, measuring cross-sectional area (mm2), and mean (Dmean), maximal (Dmax) and minimal diameter (Dmin). Elliptical ratio was calculated as Dmax/Dmin (1.0=perfect circularity). Strut malapposition on OCT was defined by a 130 µm threshold, covering stent+coating thickness and OCT axial resolution (15 µm). After millimetric cross-sectional stent analysis, global malapposition was calculated as percentage malapposed/total struts. Final SBO was calculated by planimetry on 3D-OCT as (A1/A2)×100% (A1=total strut area in ostium; A2=total ostium area).
STATISTICAL ANALYSIS
Quantitative variables were expressed as mean±standard deviation. Quantitative effects were compared using the Wilcoxon test on GraphPad Prism 5 software (GraphPad Software, La Jolla, CA, USA). The significance threshold was p<0.05.
Results
The rePOT sequence was complete in most DES, except for two of the five Coroflex stents included in final analysis, where the balloon could not cross the SB (Table 1, Figure 3).
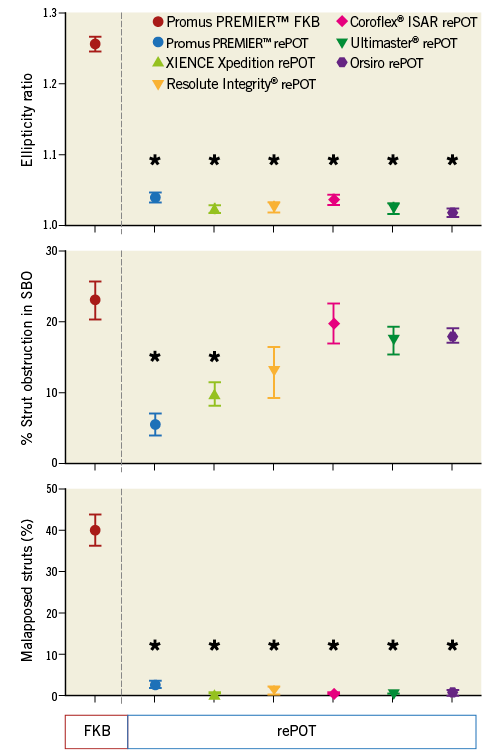
Figure 3. Comparison of main results of rePOT on the six DES versus FKB on Promus PREMIER. n=5 per group. *p<0.05 vs. Promus PREMIER by FKB. FKB: final kissing balloon; SBO: side branch obstruction
Discussion
The study validated the feasibility of rePOT provisional stenting in a range of latest-generation DES. The only two failures in SBI concerned Coroflex stents, which have the thinnest (64 µm), and possibly most fragile, struts, hence the difficulty of crossing the SB ostium.
RePOT results confirmed initial findings1, with final stent apposition and optimal SB opening without the proximal elliptical deformation caused by FKB.
The expected proximal malapposition correction after rePOT, inherent to the fractal law (2.6±1.4% to 0.1±0.2% vs. 40.4±8.4% for FKB), and conserved circularity (1.02±0.01 to 1.04±0.01 vs. 1.26±0.02) seemed less influenced by platform design. Final malapposition and elliptical deformation were homogeneous among the six stents, except for the Promus PREMIER, in which malapposition was slightly increased (p<0.05), although incomparably less than with FKB.
Platform design seems more relevant to residual SBO, which ranged from 5.6% to 20.2%, with only the Promus PREMIER and XIENCE Xpedition showing significant decrease: respectively, 5.6±3.5% and 10.0±5.3% vs. 23.5±5.7% for FKB. There are four possible hypotheses. 1) Cell size and residual SBO: the larger the design’s cell area, the smaller the SBO2; likewise, cell distensibility may influence SBO. The present results do not fully confirm these relations, as the lowest SBO was not found with the design (Promus PREMIER) with the largest cell area3. 2) DES alloy: all models were in CoCr, except Promus PREMIER in PtCr, which shows less recoil than CoCr4, perhaps accounting for the reduced SBO. 3) Strut thickness: this differed little except in Coroflex, with thinner struts (64 µm); stent mechanical properties may be affected, being proportional to the square of strut thickness. 4) Connectors and SB crossing: wires crossing the SB cell influence the final SBO5. However, no correlations were found between connector number and/or type and SBO.
Conclusions
In conclusion, DES design differences had little impact on the excellent overall rePOT results for global malapposition, vessel circularity and SB opening. The data validate provisional coronary stenting by rePOT, whatever the DES design. In vivo replication should now begin to confirm the expected clinical benefit.
| Impact on daily practice This bench study on bifurcation confirms the excellent mechanical results obtained with the rePOT strategy and side branch provisional stenting in a large range of latest-generation DES. These data suggest that rePOT may be translated into clinical practice instead of a final kissing balloon strategy independently of platform design. |
Funding
DES were provided by Abbott Vascular, B. Braun, Biotronik, Boston Scientific, Medtronic, and Terumo, unconditionally.
Conflict of interest statement
The authors have no conflicts of interest to declare.