
Abstract
Aims: A new coronary bifurcation provisional stenting technique without kissing balloon, rePOT, associating the proximal optimisation technique (POT), side branch inflation and final POT, showed excellent mechanical results in a bench test. The present study sought to use optical coherence tomography (OCT) to quantify the mechanical results of rePOT in vivo in a large patient sample with complex coronary bifurcations.
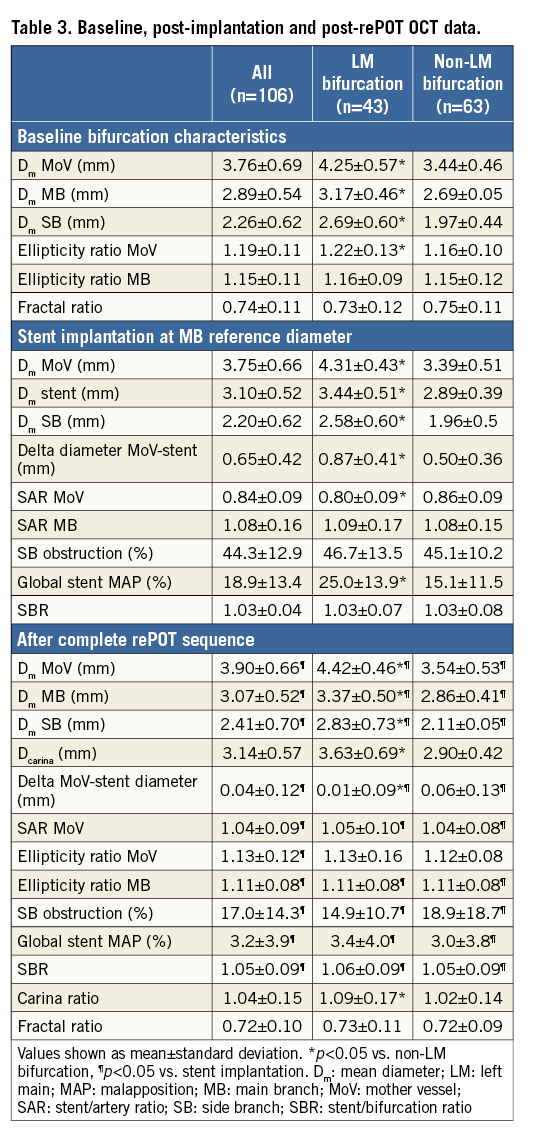
Methods and results: A total of 106 patients with coronary bifurcations were included in a multicentre prospective registry (left main, 40.6%; true Medina bifurcation, 39.6%). Three OCT runs were performed, at baseline, just after stent implantation and after the complete rePOT sequence, quantifying global malapposition, side branch obstruction (SBO), and various geometric arterial criteria. RePOT was completed systematically. RePOT significantly reduced global strut malapposition from 18.9±13.4% just after stent implantation to 3.2±3.9% (p<0.05), residual SBO from 44.3±12.9% to 17.0±14.3% (p<0.05), and ellipticity index from 1.19±0.11 to 1.13±0.12 (p<0.05). Exhaustive six-month follow-up found only one mother-vessel target lesion revascularisation.
Conclusions: This clinical study of a large sample of complex coronary bifurcations with OCT analysis showed the benefit of the rePOT sequence in provisional stenting, replicating in vivo the excellent in vitro geometric results previously reported, and confirming ease of implementation and medium-term safety.
Abbreviations
DES: drug-eluting stent
EBC: European Bifurcation Club
KBI: kissing balloon inflation
MB: main branch
MoV: mother vessel
OCT: optical coherence tomography
POT: proximal optimisation technique
SAR: stent/artery ratio
SB: side branch
SBO: side branch obstruction
SBR: stent/bifurcation ratio
TLR: target lesion revascularisation
Introduction
The poor clinical results of kissing balloon inflation (KBI) in provisional stenting1-4 led to a novel technique being developed to treat coronary bifurcations without juxtaposing two balloons, namely “rePOT”, comprising initial proximal optimisation technique (POT) + side branch (SB) inflation + final POT5.
KBI was introduced in the 2000s, moving directly from technical concept to randomised controlled trials and registries1-4 as early as 2009, with no intervening experimental validation or clinical anatomic underpinning. It was only in 2013 that Rahman et al6 conducted the first comprehensive volumetric intravascular ultrasound (IVUS) trial assessing the impact of KBI, intended to correct deformation of the SB inflation polygon of confluence; the authors clearly demonstrated proximal deformation caused by juxtaposing the two balloons, with the ellipticity ratio increasing to 1.23±0.06, associated with significantly increased stent volume in the proximal part of the bifurcation, caused by asymmetric overexpansion of the stent. In 2014, Mortier et al7 demonstrated experimentally the harmful effects of juxtaposing the two balloons, with an ellipticity ratio as high as 1.36, causing large asymmetric arterial overstretch, as seen in the results of the COBIS registry2.
The concept underlying the initial POT + SB inflation + final POT sequence emerged, as so often, from a methodical convergence of concepts initially proposed at various meetings of the European Bifurcation Club (EBC)7-11. Finet et al5 used a fractal coronary bifurcation bench test to assess benefit in terms of optimising the final result of provisional stenting in comparison with five other techniques, including KBI. RePOT gave the best results, maintaining proximal circularity in the stented area without arterial overstretch, and minimising side branch obstruction (SBO) and global stent malapposition, while respecting the fractal geometry of the bifurcation12, which is the anatomic basis underpinning the law of conservation of flow: the sum of the outflows equals the inflow. Recently, Dérimay et al13, in a comparative bench-test analysis in a large range of six main latest-generation drug-eluting stents (DES), demonstrated the reproducibility of the excellent results obtained with rePOT versus KBI.
We sought to apply a rigorous four-step methodology in developing this new technique for optimising the management of coronary bifurcations in provisional stenting: 1) precise description of the rationale; 2) experimental bench-test validation; 3) clinical replication of the targeted morphologic effects found on bench test; and 4) final validation in a randomised controlled trial.
We here report the third methodological step towards validation: we set up a multicentre prospective registry, using serial optical coherence tomography (OCT) analysis to quantify the geometric results of rePOT in a wide range of complex coronary bifurcations.
Methods
STUDY DESIGN AND POPULATION
The present clinical study was based on a multicentre (five-centre) prospective registry and aimed to quantify the morphological results of the rePOT sequence in provisional stenting. All patients admitted for coronarography with a significant coronary bifurcation lesion between October 2014 and October 2016 were eligible if the first-line revascularisation strategy was provisional stenting in line with the EBC consensus11.
Exclusion criteria comprised indications for valvular or coronary surgery, severe multivessel involvement liable to make for a complex procedure, presumed lesion instability (underlying STEMI <12 hrs, large thrombosis), contraindications to OCT (clearance <60 ml/min, tortuous coronary, major calcification, massive thrombus, narrow artery) or technical impossibility of having good-quality OCT runs, contraindications to 12-month dual antiplatelet therapy, and revascularisation strategy other than provisional stenting. Patients under 18 years of age and pregnant women were not eligible.
National ethics committees approved the study protocol, which was registered in the French clinical trial registry as ANSM N°2015-A00029-40. All patients provided written informed consent.
STUDY PROTOCOL
All the coronary bifurcations were revascularised using the rePOT provisional stenting technique5. During the procedure, three OCT runs along the principal axis (mother vessel [MoV]-main branch [MB]) were performed as shown in Figure 1 (1, baseline; 2, just after stent implantation; and 3, after complete rePOT). Stents were latest-generation drug-eluting (DES) models with diameter adapted to the MB so as to obtain a distal stent-artery ratio (SAR) between 1.0 and 1.1, as recommended by the EBC11. The rePOT was to be performed in full (Figure 1), with three steps. 1) Initial POT was performed with a compliant balloon adapted to the MoV diameter and positioned so that balloon parallelism was lost exactly at the carina; balloon inflation pressure was adjusted to achieve a proximal SAR between 1.0 and 1.1. 2) SB opening was achieved using a compliant balloon adapted to the reference SB diameter, calculated from fractal geometry14 based on the mean reference MoV and MB diameters determined on OCT. 3) Final POT was performed exactly as initial POT. Compliant balloons were used in post-dilatation in accordance with the new EBC recommendations11. If the operator considered it necessary, post-dilations or even bail-out with T- or Y-stenting could be performed. The implantation strategy for the second stent was left open.
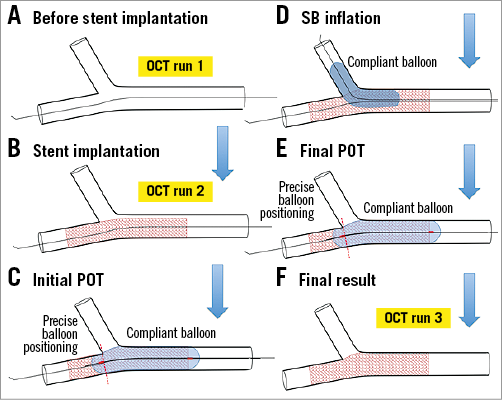
Figure 1. Clinical rePOT study protocol and analysis. A) Before stent implantation. B) Stent implantation. C) Initial POT. D) SB inflation. E) Final POT. F) Final result. OCT: optical coherence tomography; POT: proximal optimisation technique; SB: side branch
ANGIOGRAPHY ANALYSIS
Coronarography was performed according to each centre’s habits, without specification for the approach except that it should be at least 6 Fr and OCT-compatible. Angiographic parameters were quantified with quantitative coronary angiography (QCA) analysis (QAngio XA 3D/QFR; Medis, Leiden, the Netherlands) retrospectively to determine percentage stenosis, bifurcation angle, TIMI flow, and Medina classification15.
OCT ANALYSIS
The three OCT acquisitions used the Lunawave® optical frequency domain imaging (OFDI) system (Terumo Europe, Leuven, Belgium) or the Dragonfly™ Duo ILUMIEN™ (St. Jude Medical, St. Paul, MN, USA). Automatic pullback was at 10 mm/sec with contrast-medium flush left up to the operator. Run and segment (MoV and MB) parameters were: cross-sectional area (mm2), and mean (Dm), maximum (Dmax) and minimum diameter (Dmin). Ellipticity ratio was calculated as Dmax/Dmin, where 1.0 corresponds to perfect circularity. The strut malapposition threshold on OCT was set at 110 µm, whatever the DES. Global malapposition was measured on millimetre slices all along the stent, counting the number of visible and of malapposed struts per slice, to calculate global percentage malapposition. Percentage SB strut obstruction could not be quantified by QCA, and we therefore defined a new SBO parameter from the 2D-OCT runs illustrated in Figure 2. On each slice between the carina and anti-carina, SBO was estimated by the mean ratio between the longest strut-free segment (d) and the estimated SB ostium diameter (D) (i.e., %SBO=![]() ×100). Fractal ratio was calculated using the linear formula8: fractal ratio=Dm MoV/(Dm MB+Dm SB). SAR was defined as Dstent/Dref. Correct overall final bifurcation fractal geometry was assessed on stent/bifurcation ratio (SBR) defined as (Dm stent MoV+ Dm stent MB)final/(Dm ref MoV+Dm ref MB)initial. Final SBR, like SAR, should lie between 1.0 and 1.1 to avoid focal (SAR) or global (SBR) arterial overstretch. Finally, carina diameter Dcarina was defined as MB ostium diameter perpendicular to the carina (Figure 3). The carina ratio (Dcarina/Dm MB) after full rePOT thus detected and quantified any carina shift, considered significant if >10% (i.e., ratio <0.90).
×100). Fractal ratio was calculated using the linear formula8: fractal ratio=Dm MoV/(Dm MB+Dm SB). SAR was defined as Dstent/Dref. Correct overall final bifurcation fractal geometry was assessed on stent/bifurcation ratio (SBR) defined as (Dm stent MoV+ Dm stent MB)final/(Dm ref MoV+Dm ref MB)initial. Final SBR, like SAR, should lie between 1.0 and 1.1 to avoid focal (SAR) or global (SBR) arterial overstretch. Finally, carina diameter Dcarina was defined as MB ostium diameter perpendicular to the carina (Figure 3). The carina ratio (Dcarina/Dm MB) after full rePOT thus detected and quantified any carina shift, considered significant if >10% (i.e., ratio <0.90).
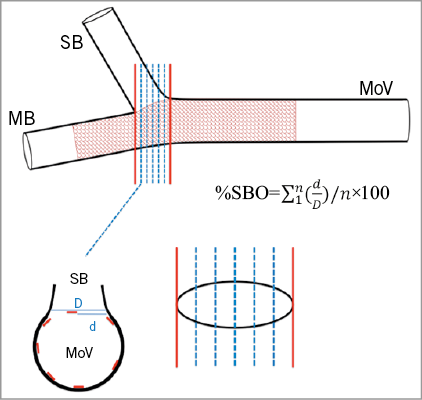
Figure 2. Quantification of the side branch obstruction (SBO). SBO was quantified by the mean ratio between the maximum strut-free distance (d) and SB diameter (D) at each frame in 2D OCT, in the MB axis, between the carina and the anti-carina (red lines). MB: main branch; MoV: mother vessel; SB: side branch
CLINICAL FOLLOW-UP AND ENDPOINTS
The primary endpoint of this study was in vivo confirmation of the mechanical and geometrical benefit of the rePOT sequence previously demonstrated in vitro 5,13, in terms of global stent strut malapposition, SBO, proximal ellipticity deformation and arterial overstretch. The secondary endpoint was outcome at six-month follow-up, defined as a composite event of cardiac death, all-cause death, myocardial infarction, stent thrombosis and target lesion revascularisation (TLR).
STATISTICAL ANALYSIS
Quantitative variables were expressed as mean±standard deviation. Mann-Whitney and Wilcoxon tests were used to compare quantitative effects, and the chi2 test for qualitative effects. GraphPad Prism 5 software (GraphPad Software, La Jolla, CA, USA) was used for analyses; p<0.05 was considered significant.
Results
CLINICAL AND TECHNICAL CHARACTERISTICS
Table 1 and Table 2 show data for the 106 patients included in the study: 40.6% of bifurcations involved the left main, 39.6% were true bifurcations according to the Medina criteria, and 48.1% showed <70° bifurcation angle. Most procedures used a radial approach (78.3%), with 6 Fr (95.3%), or else 7 Fr introducers. The rePOT sequence was always performed in full. Initial and final POT were performed in the same way. Based on the operator’s decision, four procedures (3.9%) were completed by SB stenting, without difficulty, namely one SB dissection and three residual SB stenosis >70%; these bail-outs were not followed by KBI. In seven cases, the operator abstained from treating a residual SB ostium stenosis, as it was less than 70%.
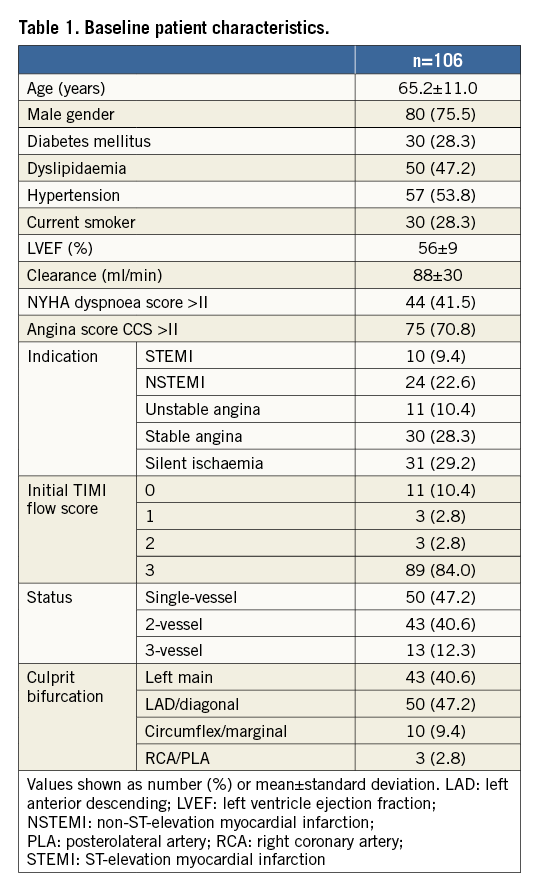
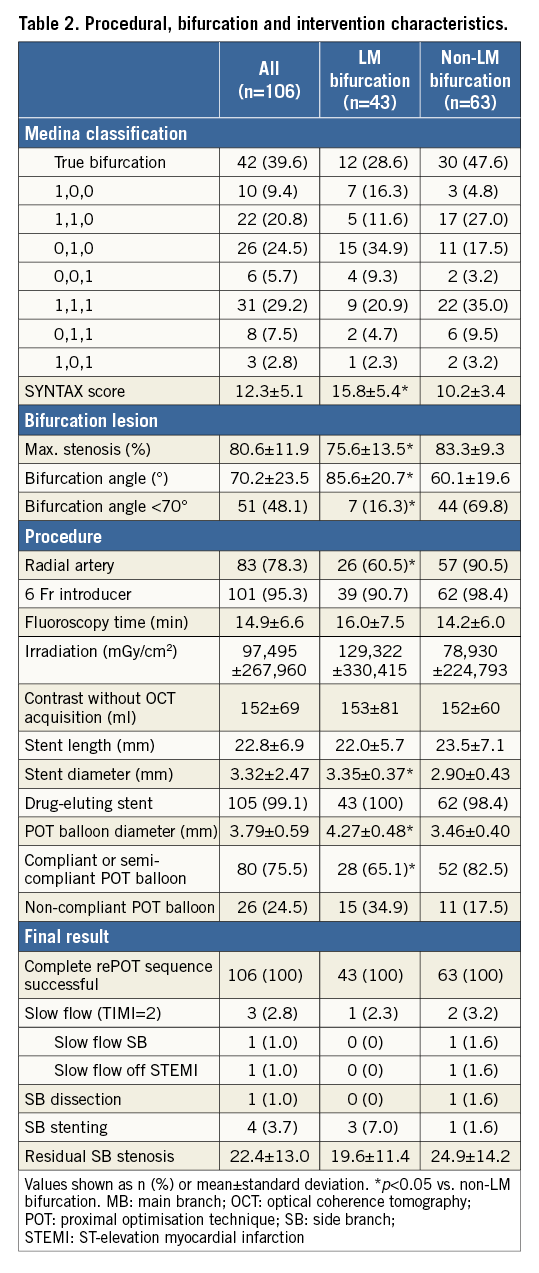
OCT DATA
Table 3 shows OCT data for the three runs - baseline, just after stent implantation, and after complete rePOT. Compared to simple stenting, rePOT reduced global malapposition from 18.9±13.4% to 3.2±3.9% (p<0.05) and residual SBO from 44.3±12.9% to 17.0±14.3% (p<0.05). This optimisation induced no additional elliptic deformation; indeed, the proximal ellipticity ratio improved significantly, from 1.19±0.11 at baseline to 1.13±0.12 at the end of the sequence (p<0.05). Global stent apposition was optimal, without harmful overstretch: final proximal SAR was 1.04±0.09 and final distal SAR 1.08±0.16, and final SBR was 1.05±0.09. There were no notable differences according to whether the bifurcation was left main or not. RePOT induced no carina shifting: carina ratio changed from >1 to 1.04±0.15. These good results were independent of carina angle, whether acute (≤70°: 1.02±0.14) or not (>70°: 1.07±0.16) (p=0.09).
CLINICAL FOLLOW-UP
Six-month follow-up was systematic and exhaustive. There was only one adverse event, i.e., TLR treated by complementary angioplasty for a focal restenosis at stent entry in the MoV. Functional improvement was also significant: mean NYHA and CCS grades decreased, respectively, from 1.6±0.8 to 1.2±0.5 (p<0.05) and 2.5±1.6 to 0.1±0.4 (p<0.05).
Discussion
This rePOT study constitutes the third methodological step, after development of the technical concept and experimental validation5,13. It is the first OCT-guided clinical study quantifying the mechanical effects of the new rePOT provisional stenting technique. It included a large sample of coronary bifurcations, with 40% left main involvement and the same proportion of true bifurcations according to the Medina criteria15. It confirmed in vivo, in 106 patients, all the expected mechanical benefits of the rePOT sequence previously demonstrated in vitro 5,13: global malapposition decreased from 18.9±13.4% to 3.2±3.9%, SBO from 44.3±12.9% to 17.0±14.3%, and proximal ellipticity from 1.19±0.11 to 1.13±0.12 without parietal overstretch. These excellent results were found for both left main and other bifurcations.
LIMITATIONS OF KBI
It is difficult to compare these present very good rePOT results with those of KBI, which have never had a real morphological analysis: unlike the present step-by-step assessment of rePOT, KBI had no experimental bench-test demonstration of its geometric effects before it became widely used. Since the early 2000s, none of the large trials performed was able to demonstrate a clinical benefit with KBI1-4. In all KBI studies, the procedural details (balloon characteristics and positioning, inflation pressures) were unknown, and KBI was compared only to simple stenting with no post-dilation, which systematically leads to the proximal malapposition expected on the basis of fractal geometry, and to SBO, the rates of which in the present post-implantation run 2 were, respectively, 20% and 36% (Figure 3, Figure 4). Independently of the subsequent technique, the 11th EBC consensus document recommends initial POT11, which was not used in any of the KBI studies.
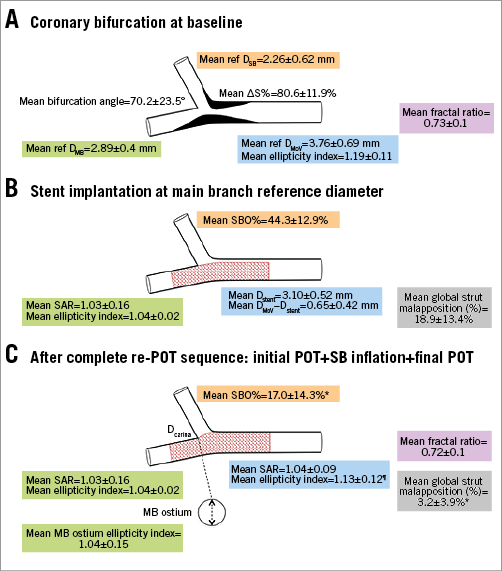
Figure 3. Morphological impacts of the rePOT sequence in the clinical setting (n=106 patients). A) Coronary bifurcation at baseline. B) Stent implantation at main branch reference diameter. C) After complete re-POT sequence: initial POT+SB inflation+final POT. *p<0.05 vs. stent implantation; ¶p<0.05 vs. baseline; D: diameter; MB: main branch; MoV: mother vessel; POT: proximal optimisation technique; ref: reference; ∆S%: percentage stenosis; SAR: stent/artery ratio; SB: side branch; SBO: side branch obstruction
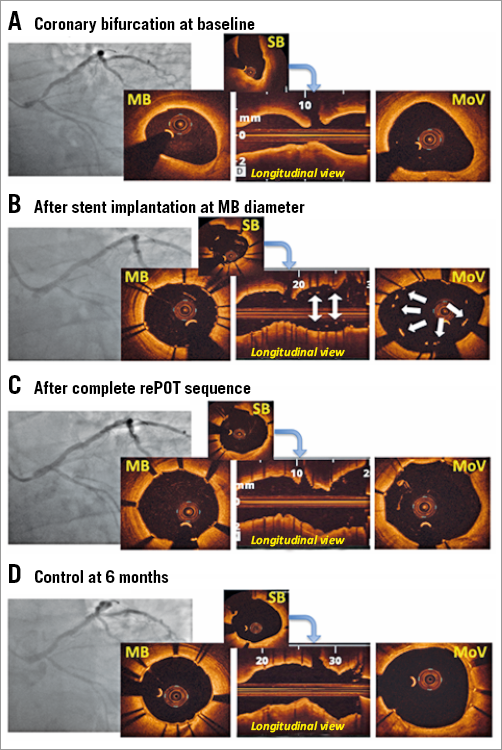
Figure 4. Example of rePOT sequence in left main bifurcation lesion. A) Left main lesion (Medina 1,1,1) in a 66-year-old male (Dm MoV=3.89 mm, Dm MB=2.85 mm). B) After stent implantation at MB diameter, Promus Premier™ (Boston Scientific) 3×16 mm at 12 atm. Large proximal malapposition: 22.4% (white arrows). C) After complete rePOT: proximal optimisation technique (POT) with compliant balloon (Maverick™; Boston Scientific; 4×9 mm at 16 atm)+SB inflation with compliant balloon (Maverick; 2.5×15 mm at 12 atm)+final POT (identical to initial POT). Dm MoV=4.11 mm, global malapposition 0.8%. D) Six-month control for atypical chest pain. Dm: mean diameter; MB: main branch; MoV: mother vessel; SB: side branch
Only recently have experimental7 and clinical studies with intracoronary imaging6,16 been carried out of the mechanical effects of KBI. They showed proximal parietal elliptic deformation induced by balloon juxtapositioning, sometimes complicated by MoV overstretch and damage to the DES coating, leading to late restenosis17-19.
REPOT SEQUENCE: CONCEPT, BENCH TEST AND CLINICAL VALIDATION
In view of this, a new technical strategy in provisional bifurcation stenting without balloon juxtaposition was recommended, respecting fractal geometry. Various concepts were developed, by Foin, Mortier and Finet, culminating in the rePOT sequence5,7-10, which conforms to the new principle of bifurcation revascularisation strategies, that “simpler is better”, as in the proven benefit of single-stent strategies20. RePOT is easy to perform, sequential (without balloon juxtaposition) and 5 Fr-compatible, and respects the geometry of the three bifurcation segments.
It comprises three steps, each essential and fundamental.
1. Initial POT is performed after implantation of a stent with a diameter suited to the MB and inflation of a compliant balloon with diameter suited to the MoV, so as to achieve SAR >1.0 as recommended by the EBC11. POT provides two clearly demonstrated mechanical benefits5: 1) reduced SBO, facilitating recrossing the SB prior to SB inflation; and 2) correction of the expected and systematic proximal malapposition which incurs a risk of the wire passing outside the stent in the MoV during SB recrossing. Recrossing is indeed best performed through the most distal strut cell in initial POT, securing a better morphologic result in the SB ostium21. To achieve all of the mechanical benefits offered by POT, however, balloon positioning is an essential factor. This positioning should be carried out so as to conserve the parallelism of the balloon up to the carina.
2. SB inflation is an essential step, limiting SB obstruction, which is a major endpoint. Experimentally, SB inflation reduced SBO from 26.0% to 3.3%5.
3. The final POT is just as indispensable, to correct any carina shift to the detriment of the MB and also any malapposition secondary to stent strut attraction facing the carina after SB inflation, mainly in the most proximal part of the polygon of confluence. Here again, benefit has been proved experimentally5, with global malapposition further reduced from 7.9% to 2.6% after final POT.
These three steps thus restore reference fractal geometry in the bifurcation, and optimal flow distribution, as seen in the SBR, which is the parameter that best reflects respect of diameter in the principal axis (MoV-MB) after stenting (without overexpansion or underexpansion).
IMPACT OF GEOMETRY
Any bifurcation stenting technique is sensitive to the angle of bifurcation between the two branches. The more acute it is, the greater the risk of carina shifting to the detriment of the MB. Conversely, angles close to 90° provide more favourable anatomy. In the present study, however, no carina shifting was observed, either for angles ≥70° (n=55) or for more acute <70° angles (n=51). This issue calls for caution in positioning the balloon in the two POT steps; even in the final POT, parallelism should be maintained up to the carina, to correct any carina shift secondary to SB inflation.
The other big problem in bifurcation stenting is the left main. The prognostic implications of its large myocardial territory demand an optimal final morphological result for both the MoV and its two coronary branches. In the present study, which included 43 left main bifurcations (40.6%), this objective seems clearly to have been met, with final malapposition reduced to 3.4% and SBO to around 10% without impairing the circularity of the proximal vessel (the left main).
Study limitations
The main limitation of the present study is that it was based only on a prospective registry. However, the aim was to replicate in vivo the mechanical benefits demonstrated on bench test, and the technical feasibility of the rePOT sequence. This is a methodologically fundamental stage in the step-by-step validation of a new interventional technique.
Another limitation was that 3D OCT was not used, which could have improved on 2D quantification of residual SBO. However, although 3D OCT is effective in vitro5,13, it shows limitations in vivo – longitudinal resolution defect due to voxel width, the spatial resolution of which is non-isotropic, and sensitivity to artefacts due to heart movement. Also, given the need for iterative OCT, compatible coronary networks were chosen. However, only high-resolution 2D intracoronary imaging such as OCT could precisely quantify stent apposition and the final mechanical result. All the OCT runs were analysed in an open label manner for the single technique used, rePOT. Moreover, although rePOT appeared to be safe in the present study, with only one TLR at six months, the small study population entailed a lack of power for any definite conclusion to be drawn. Lastly, despite the multicentre design, a centre effect is possible as the study was performed only in expert centres experienced in percutaneous bifurcation revascularisation and the rePOT technique.
Conclusions
This clinical study with a large sample of complex coronary bifurcations studied on OCT demonstrated the benefit of the rePOT sequence in provisional stenting, replicating in vivo the excellent experimental mechanical results obtained and published in vitro, while also confirming ease of implementation and medium-term safety. The last methodological stage in the step-by-step demonstration of the benefits of rePOT will be an assessment of the clinical impact of this new rePOT sequence in a large randomised controlled trial.
| Impact on daily practice This new sequential, 5 Fr-compatible rePOT provisional bifurcation stenting technique provided optimal morphologic results without kissing balloon inflation. The results previously demonstrated and compared on bench testing were confirmed in vivo in the present study, showing that, in pathological coronary arteries, rePOT 1) restored optimal bifurcation geometry, with a fractal ratio of 0.72, 2) reduced overall strut malapposition to 3.2%, 3) reduced strut obstruction of the side branch ostium to 17.0%, and 4) provided very good six-month safety. The present findings encourage widescale use of rePOT, with no particular restrictions in terms of coronary anatomy. A large randomised controlled trial should validate all the clinical benefits expected from rePOT. |
Conflict of interest statement
The authors have no conflicts of interest to declare.

