Following remarkable advances in device technology and procedural techniques and experience, percutaneous coronary interventions (PCI) are currently performed in increasingly advanced disease and complex coronary anatomies – configurations that would have been considered only for bypass surgery in the past. Still, complex lesions pose procedural challenges to the interventional cardiologist and remain predictors of poorer PCI outcomes. Bifurcation lesions comprise one of the major components of complex lesions and represent about one of six procedures in current interventional practice; much attention has focused on how treatment options can be refined and outcomes further improved in this context1. The inherent limitations of depicting the 3D coronary anatomy by means of 2D angiographic projections becomes even more problematic in bifurcation lesions due to overlapping and foreshortening with angiography alone. Intracoronary imaging can visualise the intraluminal and transmural anatomy of the native as well as the stented coronary vessel2, and improves PCI outcomes, particularly in more complex patient and lesion subsets, as shown in multiple trials and meta-analyses3,4. It therefore seems reasonable that bifurcation stenting may have greater potential to benefit from more accurate visualisation and technical refinements achievable by means of an imaging-guided strategy. While intracoronary imaging in properly selected patients has been recommended in guidelines for years, it was only recently that an expert consensus paper by the European Association of Percutaneous Cardiovascular Interventions (EAPCI) summarised practical recommendations on the use of imaging for PCI guidance and optimisation. Details of bifurcation PCI were not addressed in that document5. In this issue of EuroIntervention, a consensus document by the European and Japanese Bifurcation Clubs focuses specifically on the use of optical coherence tomography (OCT) in coronary bifurcations6.
The European Bifurcation Club recently celebrated its 10th anniversary and belongs to the most productive consensus groups in cardiology with annual publications that frequently head the download rankings of EuroIntervention, which attests to their high practical impact on operators.
Onuma and colleagues summarise the evidence and make recommendations on the utilisation of OCT including preprocedural lesion assessment, periprocedural guidance, and post-procedural optimisation of the stenting result6. The value of OCT for depicting lesion anatomy and plaque distribution is stressed, including the potential of OCT-angiography co-registration for guidance of the intervention. 3D reconstruction is strongly recommended for better appreciation of the bifurcation anatomy as well as the stent-vessel interaction. The use of on-line and off-line software is discussed; it should be borne in mind that on-line, easy-to-use applications are most helpful to operators and will probably be the key determinant of widespread use in clinical reality. Notably, 3D reconstruction of the OCT pullback of the main vessel (MV) allows reasonably accurate evaluation of the side branch (SB) ostium. This is potentially important as SB OCT is unlikely to become routine practice and the indirect depiction of the SB ostium by screening the MV pullback is an additional, valuable piece of information. OCT-based evaluation of the carina tip angle is also highlighted, as it provides incremental information that may impact on acute SB complications (and thereby bifurcation PCI strategy) and, in the longer term, strut coverage. Regarding stent length selection, the recommendation to add at least 6-8 mm from the proximal stent edge to the bifurcation carina to enable subsequent POT is particularly relevant, even when the proximal MV is free of disease. Given the importance of re-crossing the SB ostium strut cell in the most distal cell, the use of OCT is recommended to assess the position of the re-crossing wire and for exclusion of abluminal rewiring. Verification of distal cell re-crossing may be challenging in clinical practice and the obtained images may not always be as clear as the respective illustrations in the paper. Overall, the above-mentioned aspects are addressed in detail and with clear recommendations. The relevant issue of how to select the bifurcation strategy based on OCT remains a little unclear and could have been explained in more depth. Figure 1 highlights the essential recommendations in the document6.
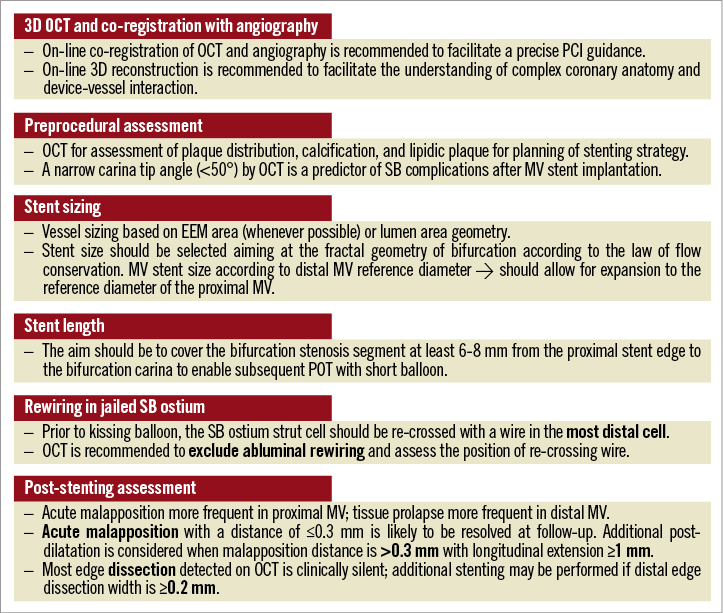
Figure 1. Highlights of the consensus document on OCT in coronary bifurcation lesions.
In view of the ability of high-resolution OCT to depict even subtle stent abnormalities, operators are frequently faced with the question of the clinical relevance of the detailed OCT findings, and whether these should be corrected or not. With regard to post-procedural optimisation, the authors attempt to provide clear guidance with specific recommendations and cut-offs6. Separate evaluation of stent expansion in the proximal MV, distal MV and SB vs. the respective reference areas is recommended. It should be noted, in this respect, that (i) current software for both available OCT imaging systems does not allow these assessments for the SB, although future iterations will; and (ii) importantly, no expansion target (% of minimal stent area [MSA] compared with the respective reference) is proposed. The clinical relevance of acute malapposition has been a debatable issue; it is recommended that post-dilatation is considered in cases of malapposition with a distance >0.3 mm (vs. the proposed cut-off of 0.4 mm in the EAPCI consensus paper5) and longitudinal extension ≥1 mm 6. Residual malapposition that is resistant to final kissing balloon inflation and POT is not uncommon in routine clinical practice; expert guidance on how this could be solved is not provided in the document and would be appreciated.
The limitations of OCT in the context of bifurcation stenting and gaps in evidence are appropriately acknowledged by the authors6. First, compared with IVUS, there is much less evidence of clinical outcomes with OCT-guided interventions; the clinical value of this approach (overall, and not specifically in bifurcation stenting) remains to be determined in properly designed studies. Against this background, one may ask why this consensus is focused on OCT only and not IVUS guidance as well; the superior resolution, ease of use and interpretation, and advanced available software are important factors that can reasonably justify the focus on OCT. The ongoing ILUMIEN IV trial (NCT03507777) will compare target vessel failure in 2,500 patients with high-risk clinical or angiographic characteristics randomised to OCT-guided vs. angiography-guided PCI. There is currently observational but sparse randomised evidence for OCT in bifurcation PCI. Dedicated randomised trials are currently underway (OCTOBER: NCT03171311; OPTIMUM: NCT02972489; DOCTOR Recross: NCT02234804). OCT is not suitable for assessing ostial left main lesions or determining the haemodynamic relevance of a stenosis, although studies are underway (OPTICO LM). The SB part that is not visible by OCT should not be ignored; angiography will always remain highly important here and, in a broader perspective, also to select the bifurcation stenting strategy. We need to keep in mind that a solely OCT-based bifurcation PCI is not possible for these reasons despite the enthusiasm for it.
The penetration of intracoronary imaging in real-life practice remains quite low in countries other than Japan due to a number of perceived or real barriers including cost, reimbursement issues, or inadequate training7. In addition to more scientific evidence from ongoing or future studies, there are other unmet needs to be addressed in order to improve the partly unjustified underutilisation of intracoronary imaging in clinical practice. Significant aspects include standardisation of preprocedural assessment and, importantly, post-procedural optimisation strategies, and proper education in the interpretation of OCT findings. In this respect, this consensus paper represents a relevant step forward for OCT in bifurcation stenting. The authors are to be commended for putting together the available evidence, formulating clear recommendations, providing valuable tips and tricks, and highlighting the limitations and current gaps in evidence. The superb work with the supporting Figures deserves particular note, as they provide examples of the incremental information that is simply impossible to obtain by angiography alone and illustrate how OCT will take bifurcation PCI to a higher level. In anticipation of new studies that are expected to inform our clinical practice better, this consensus document will be a useful companion to all operators.
Conflict of interest statement
L. Räber receives research grants to the institution from Abbott Vascular, Boston Scientific, HeartFlow, Sanofi, and Regeneron, and speaker honoraria from Abbott Vascular, AstraZeneca, Amgen, Biotronik, CSL Behring, Sanofi, and Regeneron. K.C. Koskinas has no conflicts of interest to declare.