The coronary bifurcation has long proven to be a common but challenging lesion subset that the interventional cardiologist must face.1-3 Despite the general consensus that the “simpler is better approach” to be the preferred treatment strategy1,4 –as endorsed by the European Bifurcation Club2– practices amongst interventional cardiologists in certain bifurcation lesion subtypes differ, with the quote that “the simplest approach is not always the best approach.”1 Specifically that in selected cases an upfront 2 stent strategy may be preferable to the relatively simple provisional T-stenting approach.
Improvements to the provisional T-stenting approach are increasingly being reported in the literature: these range from the pressure wire assessment of jailed side branches (SideB);5 the passage of the coronary wire into the distal cell covering the SideB ostium after main branch (MainB) stenting to allow for kissing balloon post-dilatation (KBPD) and subsequent clearance of over-hanging struts at the SideB ostium6-10; the proximal optimisation technique (POT)2 to best avoid SideB compromise, facilitate coronary rewiring of the SideB and allow for appropriate stent apposition; fluoroscopic based assessment of stent expansion (such as Stent Boost)11; – the list continues to grow…
In this issue of EuroIntervention, two important papers are added to the expanding literature on undertaking the provisional T-stenting approach. Mylotte et al12 describe the clinical application of the novel technique – first reported by the European Bifurcation Club 20102 – of utilising non-compliant balloons to undertake KBPD after MainB stenting. The use of non-compliant balloons to perform KBPD would theoretically minimise balloon over-expansion (a feature of compliant balloons) in the SideB with a consequent risk of vessel injury/restenosis, and stent under-expansion in the MainB stent. The lack of a control arm and the relatively small numbers (n=100) in this pilot study are obvious; the authors, however, do demonstrate the safety and feasibility of this technique, utilising the low profile Hiryu (Terumo Corporation, Tokyo, Japan) non-compliant balloon. The take-home message is very practical and can be incorporated with relative ease into clinical practice. One perhaps notable critique of this study is that angiographic criteria alone were used for assessing the need for SideB stenting – noting that only a quarter (27%) of cases with a residual angiographic narrowing of ≥75% in the SideB had a functionally significant narrowing in a previous classic pressure wire study.5 Furthermore, the requirement to make an angiographic acceptable appearance of the SideB ostium may have driven the operators to use higher pressure balloon inflations or larger size balloons, with the consequent risk of inducing SideB ostial dissection and the need for two stents.
It is becoming increasingly clear that further adjunctive device(s) may be required to assess the ostium of the SideB. Two-dimensional axial intravascular ultrasound (IVUS), optical coherence tomography (OCT) and pressure wire assessment have all proven feasible.5,6,13-15 Furthermore, in this issue of EuroIntervention, Suárez de Lezo et al16 elegantly demonstrate the use of longitudinal IVUS studies to describe the ‘eyebrow’ sign, “a powerful predictor of ostial SideB damage after stent implantation in the MainB in bifurcation coronary lesions without plaque involving the SideB.”
The eyebrow sign is impressively illustrated in the figures accompanying the paper. The concept being that MainB stenting during the provisional T-stenting approach can lead to carina shift and pinching of the SideB ostium, with subsequent SideB compromise. Furthermore, when KBPD is performed, the authors demonstrate the repositioning – “endoluminal displacement” – of the carina so that the SideB is no longer compromised. The authors use the term “damage” to describe the eyebrow phenomenon which is helpfully defined as “an increase of the percentage of ostial stenosis by QCA ≥30%”. Further adding to this novel concept is that plaque located at the carina –which most often can occur when it grows from the opposite lower shear stress wall to the higher shear stress carina17– was significantly less likely to be associated with the eyebrow sign. Presumably, the presence of more fibro-calcific plaque on the carina would make it more resistant to expansion and, subsequently, at a reduced risk of carina shift.
The authors then continue by associating the presence of the eyebrow sign with shallower bifurcation angles, and the lack of the eyebrow sign with a more perpendicular bifurcation angle (62°±23° vs. 76°±24° respectively, p<0.05). These absolute values of the bifurcation angle, although statistically supportive of this concept, should be viewed as a guide given the lack of 3-dimensional quantitative coronary angiography, which would have improved the accuracy of the SideB angulation measurements.18,19
Yet when we interpret the results of this study and its implications for clinical practice, can we now be sure we fully understand the mechanisms of SideB closure? Not until recently has the concept of carina shift as the predominant mechanism of SideB closure been widely accepted, with the previously long-held view that the so-called “snow-plough” effect, secondary to plaque shift, being the main aetiology. The latter does still occur, but to a substantially lesser degree than previously thought,1,5,14,17,20,21 and rarely in this reported study by Suárez de Lezo et al16.
3D-OCT
Recently 3-dimemsional OCT has demonstrated the potential application in improving our understanding of coronary bifurcations and the effects of the provisional T-stenting approach.9,22-24 Firstly, a proposal of classification was made based on the number of compartments the SideB orifice was divided into by the jailed stent struts.24 Secondly, hypotheses based on 3-OCT reconstructions during the provisional T-stenting approach were made, introducing concepts such as “parallel” (Figure 1) and “perpendicular” (Figure 2) bifurcations related to the SideB angulation with the MainB.9,22,23 The results of Suárez de Lezo et al16 further add to the evidence supporting these hypotheses. The eyebrow sign is related to shallower bifurcation angles, and fits into the concept of a parallel bifurcation, where the origin of the MainB and SideB take off parallel to each at the carina (Figure 1) until the SideB undergoes a change of direction. Consequently, MainB stenting in a parallel bifurcation may compromise the SideB (with the resultant eyebrow sign), whereas with the perpendicular bifurcation (Figure 2) this may not be so apparent because of the differing appearances of the carina. In support of this hypothesis are studies associating smaller bifurcation angles with more carina shift.15,25-27 The implications of these findings may be that by simply assessing the bifurcation angle with QCA, a prediction could be made through which SideB may be at risk of carina shift and compromise, and thus need protecting with a coronary wire.
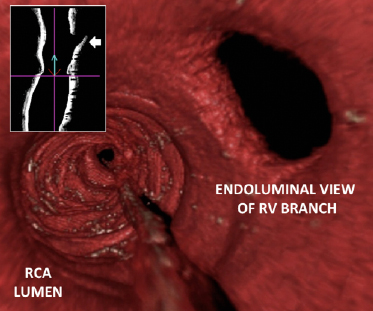
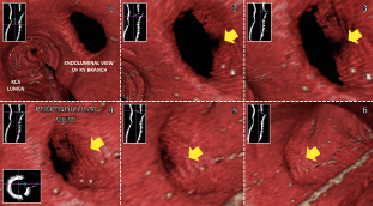
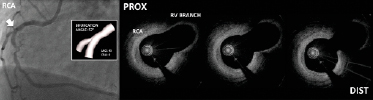
Figure 1. Principle of a “parallel bifurcation”. Downstream (proximal to distal) fly-through view of the right coronary artery (RCA) – right ventricular (RV) branch bifurcation (upper image). Note the characteristics of the carina interposed between the parallel origins of the MainB and SideB. Further note the progressive more perpendicular endoluminal views of the RV branch opening (middle image: numbers 1-4) culminating in the almost apparent concealment of the RV branch opening behind the proximal rim of the carina. With more retrograde endoluminal views (middle image: numbers 5-6), this leads to the apparent “disappearance” of the RV branch opening. The bifurcation angle is 57° on the corresponding 3-dimensional QCA (CAAS 5.9, Pie Medical Imaging, Maastricht, The Netherlands) (lower images). Longitudinal and cross-sectional 2D OCT images of the bifurcation, with a blue arrow superimposed on it are used to orientate the reader within the vessel – the base and direction of the blue arrow indicates from and in which direction respectively the 3D image is visualised from in 2D plane(s). Adapted and reproduced from Farooq et al.9 (with kind permission from Elsevier)
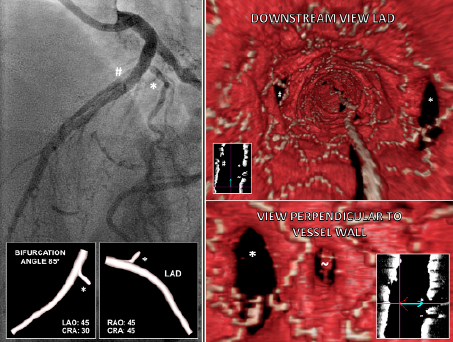
Figure 2. Principle of a “perpendicular bifurcation”. The take-off the SideB (diagonal vessel) from the MainB (left anterior descending artery - LAD) originates perpendicular to the LAD at the point of divergence of both vessel origins, with a bifurcation angle of 85° demonstrated on 3-dimensional QCA.19 A downstream fly-through view (proximal to distal) of the LAD (upper right image) demonstrates the diagonal vessel opening (asterisked), note the elliptical shape of the vessel opening and the observation that the diagonal vessel opening is fully visible, and not concealed by the carina, when visualised perpendicular to the vessel wall (lower right image). Reproduced from Farooq et al.9 *indicates diagonal branch, ~ small diagonal branch, # septal branch.
One interesting observation of the coronary bifurcation on 3D-OCT is the ellipsoid or oval appearances of the SideB opening, which is especially notable in the illustrated LAD diagonal bifurcation (Figure 2), and appears to be evident in most bifurcations, especially after MainB stenting.9,15,30 This observation perhaps warrants closer attention given the lack of any association between QCA and ostial SideB “lesions”.5,28,29,31 Once again, 3D-OCT may hold the answers to explaining this apparent paradox. It may be hypothesised that during coronary angiography, the plane of the angiography cuts the SideB in the narrower segment of the ellipsoid opening (which would be more likely to occur) rather than the longer segment given its oval shape, consequently the impression of angiographic SideB compromise is erroneously visualised.
Further adding to the potential appeal of 3D-OCT is the principle of passing the coronary wire into the distal cell of the struts covering the SideB after MainB stenting, during the provisional T-stenting approach. This is to reduce the likelihood of causing multiple malapposed struts if the coronary wire is passed into the more proximal cells and KBPD performed as illustrated (Figure 3). If the coronary wire is passed into the most distal cell, then KBPD would subsequently displace the struts covering the SideB ostium so that they opposed the SideB vessel wall opposite the carina (akin to the “skirt” technique30).
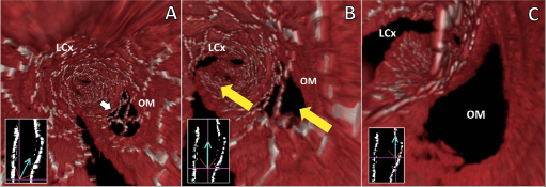
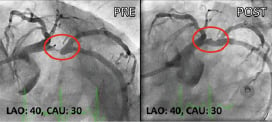
Figure 3. Provisional T-stenting: the principle of re-crossing the coronary wire (after MainB stenting) into the SideB through the most distal cell in a parallel bifurcation. Progressive downstream fly-through views culminating in the endoluminal point of view being located at the carina (A to C). White arrow indicates the most distal cell where the coronary wire would be recommended to be passed; yellow arrows indicates the parallel courses of the left circumflex coronary artery (LCx) and obtuse marginal (OM) vessels at their point of divergence. Use the orientation figures (inset lower left images) in A-C to locate the endoluminal point-of-view (base of blue arrow). In this parallel bifurcation, the struts located in front of the carina (A) are actually a prominent metallic extension of the carina and not covering the SideB opening (B-C). The potential to advance a coronary wire beneath the malapposed struts in the proximal vicinity of the ostial rim appears to be very real, and if SideB dilatation were performed, would result in multiple unappposed struts taking-off from the carina. Corresponding coronary angiograms are illustrated below. Adapted and reproduced from Farooq et al.9 (with kind permission from Elsevier)
In addition, 3D-OCT may potentially allow for the visualisation of the final result after a 2-stent bifurcation stent approach. This may guide the need for passage of the coronary wire into the appropriate cell to allow for further post-dilatation to clear any malapposed struts, guide the size of the angioplasty balloons needed to clear malapposed struts and ensure adequate ostial expansion, even if KBPD had already been performed as illustrated (Figure 4).
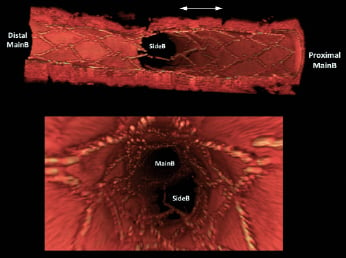
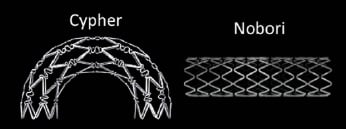
Figure 4. 3D-OCT of a two-stent approach to bifurcation stenting. Complex stenting was performed in a parallel bifurcation in a non-diseased porcine model. Firstly a Nobori® stent (Terumo Corporation, Tokyo, Japan) was deployed from the proximal MainB into the SideB. A Cypher® stent (Cordis Corporation, Johnson & Johnson, Miami Lakes, FL, USA) was subsequently implanted in the MainB – the area of overlap between the SideB and Main B stent was minimal (double white arrow) – followed by kissing balloon post-dilatation (KBPD). Note the malapposed struts straddling the coronary ostium and dividing it into compartments in the oblique longitudinal (upper image) and downstream fly-through views (middle image), presumably secondary to balloon under-sizing during KBPD. If this occurred in the catheterisation laboratory with the availability of on-line 3D-OCT, this may have triggered the operator to ensure the coronary wire was passed into the largest cell in the SideB ostium and to perform KBPD with a larger angioplasty balloon in the SideB. Images of actual Cypher and Nobori stents are displayed below.
The technology of 3D-OCT is rapidly progressing. If features like real-time 3D-OCT to allow for its immediate use in the catheterisation laboratory to assess the results of the bifurcation intervention, the introduction of quantitative measurements to allow for a more objective assessment of the SideB ostium and the need for further intervention, then the potential for the research and clinical application of 3D-OCT would be very promising.22 Perhaps then, 3D-OCT may be seen more as an important adjunctive tool in the catheterisation laboratory, rather than an instrument to create visually appealing images.
Conflict of interest statement
The authors have no conflicts of interest to declare.
References

