
Bifurcation lesions are associated with increased procedural complications and worse long-term outcome. Multiple techniques are available, including the dedicated drug-eluting Axxess™ stent system (Biosensors International Ltd., Singapore, Singapore), providing complete bifurcation support without covering the carina. Low rates of restenosis in both main vessel (MV) and side branch (SB) have been demonstrated. High-resolution imaging techniques such as intravascular optical coherence tomography (IV-OCT) may help the positioning and implantation of the Axxess device, as angiographic guidance alone may be insufficient.
A Medina 1,1,1 bifurcation lesion was treated using the Axxess device and BioMatrix™ stents (Biosensors International Ltd.) in the distal branches (Moving image 1-Moving image 5). High-resolution IV-OCT pullbacks were performed during different procedural stages (Moving image 6-Moving image 8) and 3D IV-OCT reconstructions were created using dedicated software. We describe device-specific characteristics and provide key landmarks visible in on-line 2D IV-OCT cross-sections, which may be useful in guiding device implantation.
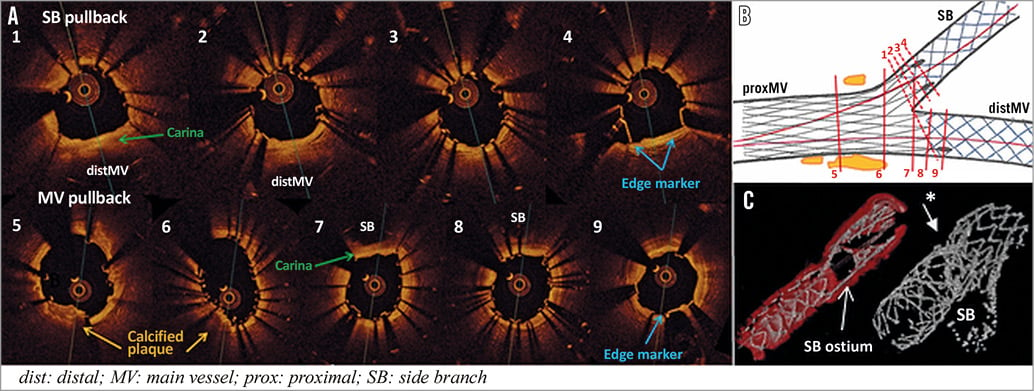
Final OCT pullback cross-sections in the SB (cross-sections 1-4) and MV (cross-sections 5-9) after implantation of the Axxess device, additional BioMatrix stents in the distal branches and final proximal stent optimisation are shown in panel A. Panel B shows a schematic illustration of levels of cross-sections. A single stent layer is maintained in the bifurcation core (cross-section 6) and the branch ostia. The carina itself is free of struts (cross-sections 1,7). The Axxess device spans the outer vessel wall at the level of the flow divider, creating a short segment of partial non-circumferential stent overlap at the side opposing the carina, i.e., an outer layer of Axxess stent struts and an inner layer of BioMatrix stent struts (cross-sections 2,7). Circumferential coverage of BioMatrix struts is seen in the distal branches (cross-sections 3,8). Two gold edge markers extend in the SB (cross-section 4) and one in the distal MV lumen (cross-section 9), covered by a circumferential layer of BioMatrix stent struts. 3D IV-OCT reconstructions illustrate distal flaring of the Axxess device providing optimal SB coverage. Early suboptimal proximal stent deployment caused by a calcified plaque is illustrated (cross-sections 5 and 6, and panel C asterisk).
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Baseline angiography demonstrating a Medina 1,1,1 bifurcation lesion involving the LAD coronary artery and first diagonal branch (LAO view with cranial inclination).
Moving image 2. Angiography showing positioning of the Axxess device in the bifurcation core. Progressive flaring of three gold markers at the distal stent edge, positioned in both distal branches, facilitates positioning of the self-expanding Axxess stent system. Once an optimal position is obtained, the sheath is further retracted from the rapid exchange delivery catheter and complete stent deployment is seen (LAO view with cranial inclination).
Moving image 3. Additional BioMatrix stents are positioned in both distal branches and implanted using the V-stenting technique. Special attention is given to avoid too proximal stent deployment which might compromise the advantage of sparing the carina from stent struts. Distal edge markers of the Axxess stent system extend beyond the distal stent edge (LAO view with cranial inclination).
Moving image 4. Simultaneous kissing balloon inflation using the stent delivery balloons is performed after additional distal stent implantations, to avoid stent malapposition at the short area of stent overlap and correct possible geometrical alterations at the level of the carina after distal stent implantation (LAO view with cranial inclination).
Moving image 5. Angiography after final proximal stent optimisation shows an optimal angiographic result after bifurcation PCI using the Axxess stent system and additional implantation of BioMatrix stents in both distal vessels. The three distal edge markers of the Axxess device are clearly positioned in the distal branches. Despite post-dilatation, a small area of early suboptimal stent deployment is seen in the main vessel at the side opposite the carina, just proximal to the bifurcation (LAO view with cranial inclination).
Moving image 6. Baseline high-resolution IV-OCT pullback in the main vessel demonstrates a large eccentric calcified atherosclerotic plaque extending in the MV from 9 to 5 o’clock, opposite the SB origin. Typical bifurcation lesion plaque distribution with sparing of the carina is clearly demonstrated. A normal three-layered arterial wall structure is seen in the distal side branch.
Moving image 7. High-resolution IV-OCT pullback in the side branch after Axxess device implantation shows progressive transition from a proximal circular stent expansion to a more oval shape in the bifurcation core, proximal to the flow divider. The flow divider itself and branch segments in the immediate vicinity of the carina remain free of stent struts. Two distal edge markers extend in the distal SB lumen and one marker in the distal MV. Mild stent malapposition is seen in the proximal main vessel.
Moving image 8. Final high-resolution IV-OCT pullback in the SB after additional BioMatrix stent implantation in the distal branches and POT. A single stent layer is maintained in the bifurcation core and branch ostia, while the carina remains free of stent struts. Axxess stent struts span the outer vessel wall of both branches at the level of the flow divider, creating a non-circumferential double strut layer with Axxess stent struts at the outside and an inner layer of BioMatrix stent struts. Circumferential coverage with an inner layer of BioMatrix stent struts is documented more distal in the SB. A protruding calcified plaque is seen in the proximal main vessel, resulting in regional suboptimal stent deployment despite final POT.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Baseline angiography demonstrating a Medina 1,1,1 bifurcation lesion involving the LAD coronary artery and first diagonal branch (LAO view with cranial inclination).
Moving image 2. Angiography showing positioning of the Axxess device in the bifurcation core. Progressive flaring of three gold markers at the distal stent edge, positioned in both distal branches, facilitates positioning of the self-expanding Axxess stent system. Once an optimal position is obtained, the sheath is further retracted from the rapid exchange delivery catheter and complete stent deployment is seen (LAO view with cranial inclination).
Moving image 3. Additional BioMatrix stents are positioned in both distal branches and implanted using the V-stenting technique. Special attention is given to avoid too proximal stent deployment which might compromise the advantage of sparing the carina from stent struts. Distal edge markers of the Axxess stent system extend beyond the distal stent edge (LAO view with cranial inclination).
Moving image 4. Simultaneous kissing balloon inflation using the stent delivery balloons is performed after additional distal stent implantations, to avoid stent malapposition at the short area of stent overlap and correct possible geometrical alterations at the level of the carina after distal stent implantation (LAO view with cranial inclination).
Moving image 5. Angiography after final proximal stent optimisation shows an optimal angiographic result after bifurcation PCI using the Axxess stent system and additional implantation of BioMatrix stents in both distal vessels. The three distal edge markers of the Axxess device are clearly positioned in the distal branches. Despite post-dilatation, a small area of early suboptimal stent deployment is seen in the main vessel at the side opposite the carina, just proximal to the bifurcation (LAO view with cranial inclination).
Moving image 6. Baseline high-resolution IV-OCT pullback in the main vessel demonstrates a large eccentric calcified atherosclerotic plaque extending in the MV from 9 to 5 o'clock, opposite the SB origin. Typical bifurcation lesion plaque distribution with sparing of the carina is clearly demonstrated. A normal three-layered arterial wall structure is seen in the distal side branch.
Moving image 7. High-resolution IV-OCT pullback in the side branch after Axxess device implantation shows progressive transition from a proximal circular stent expansion to a more oval shape in the bifurcation core, proximal to the flow divider. The flow divider itself and branch segments in the immediate vicinity of the carina remain free of stent struts. Two distal edge markers extend in the distal SB lumen and one marker in the distal MV. Mild stent malapposition is seen in the proximal main vessel.
Moving image 8. Final high-resolution IV-OCT pullback in the SB after additional BioMatrix stent implantation in the distal branches and POT. A single stent layer is maintained in the bifurcation core and branch ostia, while the carina remains free of stent struts. Axxess stent struts span the outer vessel wall of both branches at the level of the flow divider, creating a non-circumferential double strut layer with Axxess stent struts at the outside and an inner layer of BioMatrix stent struts. Circumferential coverage with an inner layer of BioMatrix stent struts is documented more distal in the SB. A protruding calcified plaque is seen in the proximal main vessel, resulting in regional suboptimal stent deployment despite final POT.

