In this chapter of Tools and Techniques Clinical, optimising stenting strategy in bifurcation lesions with insights from in vitro bifurcation models is discussed using a stepwise approach. The following is a summarised overview of this technique. The complete, unabridged version with images is available online at www.eurointervention.org
Introduction
This Tools and Techniques article reviews some of the recent insights gained through experimentation in bench models and in vivo intravascular imaging for the treatment of bifurcation lesions. The article will review insights from recent in vitro studies, and we will see how these may be applied to the management of bifurcation lesions in clinical settings in vivo.
Background
Pioneering work by Lefevre, Ormiston and others introduced the use of in vitro bench models to improve our understanding of bifurcation techniques. The switch to high-resolution three-dimensional quantitative imaging with microfocus CT and scanning electron microscopy now allows a detailed study of the impact of different stent designs and deployment techniques in a controlled and reproducible environment.
Indications
For lesions with critical side branch (SB) involvement, the recommendation is to start with provisional stenting to ensure MV access and to cross over to a two-stent strategy in the case of a suboptimal result (abrupt closure, flow-limiting dissection, >75% stenosis, TIMI flow <3). Kissing balloon (KB) inflation is mandatory in two-stent techniques. KB or sequential SB main dilatation can be used in single-stent techniques to optimise the ostium or in case of SB pinching after MV stent implantation, though the advantage is less clear. Intravascular ultrasound and optical coherence tomography can be used in guiding bifurcation treatment for reducing the risk of complications and to improve stent optimisation.
Difficulties
Techniques requiring double recrossing (culotte) or wire recrossing through multiple layers of struts (mini-crush) have a higher risk for strut malapposition and failure to recross the wire or balloon for optimisation, which may lead to suboptimal deployment.
Post-dilatation of a stent beyond its label overexpansion is not recommended as distortion of the stent crowns during overexpansion can change the stent mechanical response and impair drug delivery. This may affect the ability of the stent to scaffold the lesion as well as the ability of the drug to prevent restenosis.
Although distal side branch recrossing location is critical in theory, it is difficult in clinical practice to assess and control recrossing based solely on angiographic views.
Methods
In this article different strategies of stenting bifurcation lesions will be discussed and compared based on insights learned from recent in vitro studies. Each section will focus on a specific step of the bifurcation strategy and indicate how technical considerations derived from in vitro models can be used to guide optimal treatment and understanding of in vivo intravascular imaging results.
In the online version we cover in particular the following practical topic of interest with a combination of clinical and experimental insights:
– Provisional or complex approach: advantages and drawbacks of each technique and indications for each strategy (Table 1, Figure 1).
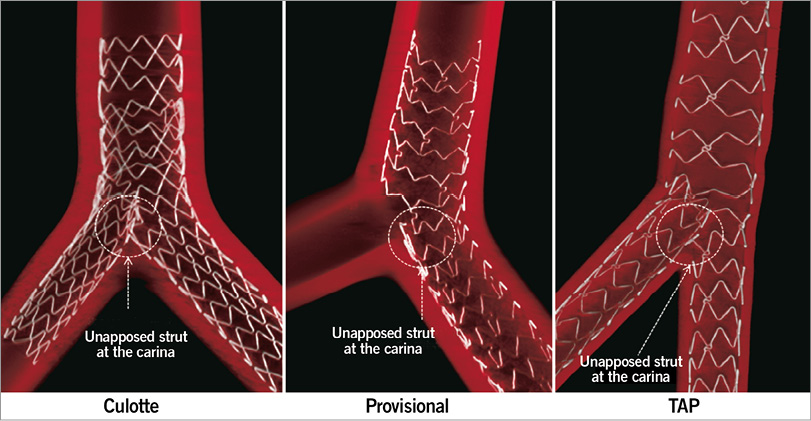
Figure 1. Culotte, Provisional and TAP techniques. The provisional T-stenting approach generally led to better strut apposition results than more complex techniques. TAP aims to avoid any gap in scaffolding but a limitation compared to conventional T-stenting remains the risk of positioning the SB stent too proximal, resulting in a stent protrusion in the MV lumen (right panel).
– Stent sizing and design selection: knowing the cut-off between each workhorse model design is critical when large post-expansion is intended.
– Importance of the proximal optimisation technique (POT): oversized balloon inflation in the proximal segment to facilitate the access to the side branch and to optimise stent expansion (Figure 2, Figure 3).
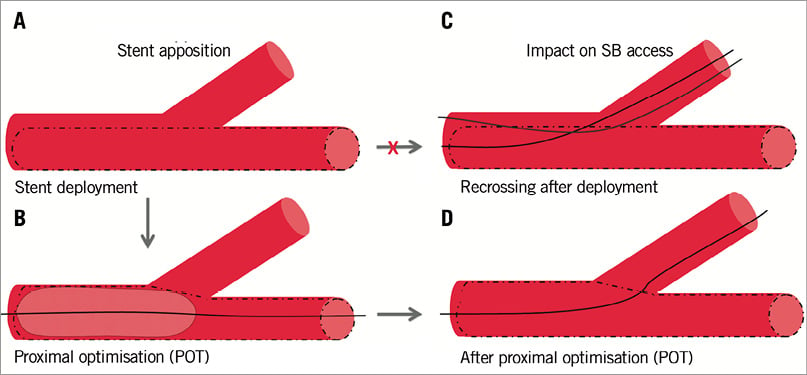
Figure 2. Proximal optimisation technique (POT), introduced by Dr Darremont to facilitate SB access, is performed with a balloon positioned in the proximal stent segment and sized to match the proximal reference vessel diameter.
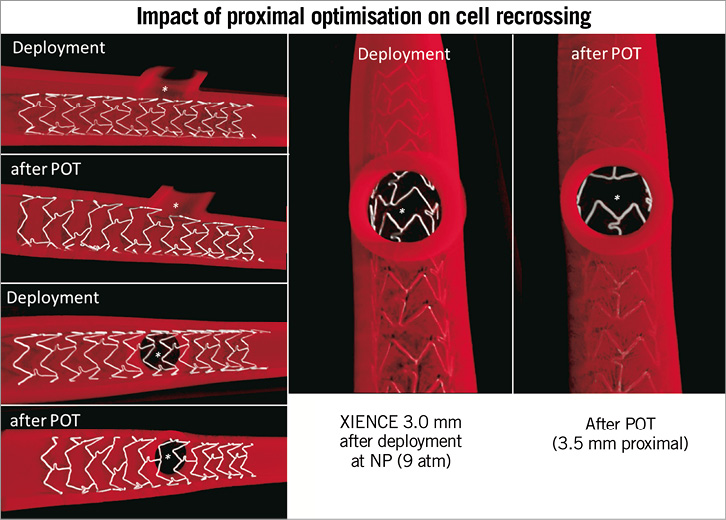
Figure 3. Impact of the POT technique on stent apposition and SB access. Comparison of the difference in stent configuration and cells available for recrossing before (deployment) and after POT. View of the strut configuration from the SB (right panel) shows how POT facilitates recrossing by creating a “funnel effect” through enlargement of the cells located in front of the SB, reducing the number of possible cells available for crossing.
– Kissing or not kissing ? Advantages and drawbacks of kissing and sequential approaches.
– Side branch access : impact of recrossing location and how to achieve distal wire recrossing step by step.
Conflict of interest statement
Research support from Medtronic, Biosensors and Abbott has been declared by all the authors, not in relation to the content of this present manuscript. The authors have no conflicts of interest to declare relative to this article.

