Abstract
Coronary bifurcations are involved in 15-20% of all percutaneous coronary interventions (PCI) and remain one of the most challenging lesions in interventional cardiology in terms of procedural success rate as well as long-term cardiac events. The optimal management of bifurcation lesions is, despite a fast growing body of scientific literature, the subject of considerable debate. The European Bifurcation Club (EBC) was initiated in 2004 to support a continuous overview of the field, and aims to facilitate a scientific discussion and an exchange of ideas on the management of bifurcation disease. The EBC hosts an annual, compact meeting, dedicated to bifurcations, which brings together physicians, engineers, biologists, physicists, epidemiologists and statisticians for detailed discussions. Every meeting is finalised with a consensus statement which reflects the unique opportunity of combining the opinions of interventional cardiologists with the opinions of a large variety of other scientists on bifurcation management. The present 11th EBC consensus document represents the summary of the up-to-date EBC consensus and recommendations. It points to the fact that there is a multitude of strategies and approaches to bifurcation stenting within the provisional strategy and in the different two-stent strategies. The main EBC recommendation for PCI of bifurcation lesions remains to use main vessel (MV) stenting with a proximal optimisation technique (POT) and provisional side branch (SB) stenting as a preferred approach. The consensus document covers a moving target. Much more scientific work is needed in non-left main (LM) and LM bifurcation lesions for continuous improvement of the outcome of our patients.
“Which way you ought to go depends on where you want to get to”.
The Cheshire Cat, Alice’s Adventures in Wonderland,
Lewis Carroll (1865)
Introduction
A bifurcation coronary lesion is a lesion occurring at, or adjacent to, a significant division of a major epicardial coronary artery1,2. A “significant” side branch (SB) is most often arbitrarily defined based upon the subjective judgement of the operator. In practice, this implies that a significant SB is a branch that the operator does not want to lose after evaluating the individual patient in a global context, i.e., patient symptoms, patient comorbidity, diameter and length of side branch, plaque burden and localisation in the bifurcation area, angle between main branch (MB) and SB, size of the myocardial mass supplied by the SB, location of ischaemia, viability of the supplied myocardium, collateralising vessel, left ventricular function, and the results of functional tests1-3.
The dilemma of bifurcation treatment
The first step in bifurcation treatment is to evaluate whether or not the SB will cause clinical problems if it is lost during the procedure. Thus, if it is known beforehand that there is a high risk of SB closure, it is possible to choose a technique that protects the SB up front, i.e., often a two-stent technique or the use of a dedicated device. A more complex technique such as this may, however, have a higher risk of periprocedural biomarker leaks (myocardial infarction) and may also be burdened with a higher risk of long-term adverse effects (restenosis, stent thrombosis, myocardial infarction, etc.)2,3. On the other hand, if the risk of SB closure is low, it is possible to choose a simpler strategy (provisional approach), with lower periprocedural risk and lower long-term event rates. This technique carries an inborn risk of losing the SB if, despite the pre-treatment risk evaluation, it closes during the procedure. As a consequence, the optimal management of bifurcation lesions is still, despite a fast growing body of scientific literature in the field, the subject of considerable debate1. The way forward calls for more long-term follow-up data in the already finalised studies to gain more knowledge of the long-term effects of the different techniques and devices. Furthermore, studies on stent techniques with the new-generation DES as well as with dedicated devices should be encouraged to define their role in the treatment of coronary bifurcations. Finally, the role of biodegradable stents and optimal implantation techniques for bifurcation treatment needs to be defined3.
Definitions
A simple description of bifurcation lesions, stenosis quantification, and PCI techniques is not straightforward. Consensus was reached by promoting a simplified and universal classification of bifurcation lesions, the Medina classification1 (Figure 1) and an accurate definition of each of the various techniques used in bifurcation stenting combined with a precise classification system to facilitate the description, the MADS classification (Figure 2)2. The two classifications have provided the valuable opportunity to standardise reports, to allow comparisons between studies and to facilitate interpretation of published results. For all these reasons, systematic use of these classifications is still strongly recommended by the EBC3.
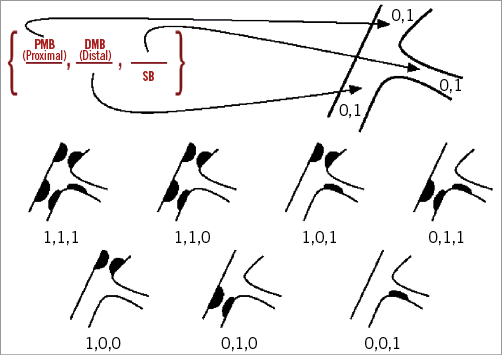
Figure 1. The Medina classification for bifurcation lesions. The ciphers describe, in order, the proximal main vessel, the distal main vessel and the side branch. The segments are termed “1” if the segment has a diameter stenosis ≥50% by visual estimation; otherwise, they are “0”.
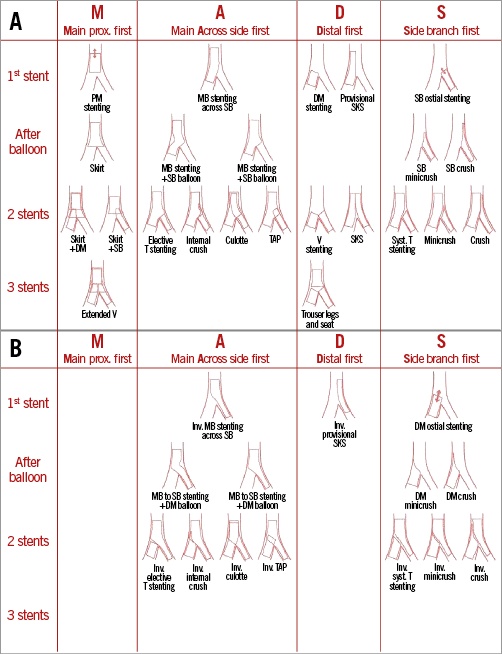
Figure 2. MADS classification. The MADS classification is a systematic description of bifurcation stenting techniques grouped in families. It is based on two principles: 1) the final position of the stent(s) (one to three stents) in the bifurcation, and 2) the implantation order. The position of the first implanted stent in a bifurcation corresponds to a given strategy out of four (MADS): M begins with a stent in the proximal part of the MV, A with a stent in the MV Across the SB, D defines a Double stent implantation, whether simultaneously or not, and S consists of a stent implantation in the SB first. A) Description of the MADS classification of bifurcation treatment. B) MADS classification of “inverted” techniques.
Anatomy
The coronary bifurcation anatomy and physiology as well as the interaction between interventional devices (stents, balloons) and bifurcated vessel walls are promising, evolving fields of research.
In recent years, coronary bifurcation anatomy has been the subject of a series of studies, which have helped to characterise the geometric relations linking MB and SB. Several mathematical models (Murray’s4, Finet’s5, Huo-Kassab’s6 and “area preservation”) have been reported and are based on different assumptions. All together such models, besides some differences in estimated coefficients, confirm that coronary bifurcation anatomy may basically be regarded as a complex vessel/function structure where three different vessel segments (proximal MV, distal MV and SB) are interpolated through the bifurcation core segment where the distinction between MV and SB is merely virtual. A recently reported experimental setting (with ex vivo angioscopy evaluation in beating hearts) for the first time allowed the visual appreciation of such complex geometry directly7. Full description of each individual bifurcation should incorporate both vessel diameters and the angles created in the three dimensions of the space by the main axes of the tree segments. Yet, major bifurcations, such as the distal LM or left anterior descending artery-diagonal tend to have different anatomic peculiarities calling for computer tomography-based atlases providing realistic bifurcation models8. Such comprehensive three-dimensional anatomic description is pivotal for future studies on the local coronary flow through bifurcated segments. Furthermore, since coronary circulation is tree-like, the flow reconstructions are expected to be influenced by the eventual presence of different SBs of different sizes9. On such bases, a series of investigations based on the flow reconstruction obtained by computer simulations before, during and after PCI in bifurcations has started to provide novel insights in the field. Of note, attempts to understand the clinical impact of bifurcation anatomy by assessing just a single geometric parameter such as bifurcation angle have so far provided inconclusive results.
Provisional stent strategy
The provisional SB stent implantation strategy should be considered the standard approach for treatment of bifurcation lesions. Although there are bifurcation lesions where a provisional approach is not the optimal initial approach, the need for an alternative approach is unusual in the majority of lesions. The EBC recommends the KISSS principle (Keep It Simple, Swift and Safe). Initially, the MV needs to be identified. The intention will be to stent this vessel first; then the SB should be treated in case of significant flow limitation, very difficult SB access or SB with a large myocardial territory (Figure 3). Specific strategies for the LM bifurcation may evolve with time and are discussed separately within this document. It is increasingly clear that long-term clinical outcomes are determined mostly by the status of the main branch (MB) after bifurcation stenting. Ensuring optimal results in the MB may be more important than optimising the angiographic appearance of the SB.
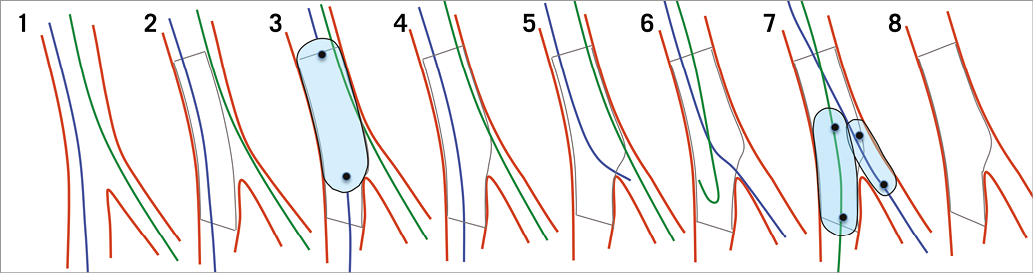
Figure 3. Provisional side branch (SB) stenting approach. From 1 to 8: wiring both branches. Main branch (MB) stenting using a stent diameter according to the distal MB reference. Proximal optimisation technique (POT). After 4, the procedure can be stopped. If SB needs attention, wire exchange, wiring the SB through the MB distal strut. Kissing balloon inflation with short non-compliant balloons in order to avoid SB dissection and stent distortion proximal to the polygon of confluence.
Initial steps
Almost all bifurcation lesions, including the distal LM bifurcation, can be safely treated by radial artery access using a 6 Fr guiding catheter. When considering stenting large vessels using adjunctive technology such as rotablation or using a strategy that requires simultaneous use of two stents, a balloon and stent, or three balloons, a larger guiding catheter may be required.
Wiring the SB should be considered the standard approach unless the SB is so small that, in the opinion of the operator, its loss would be irrelevant. As this decision can be difficult to make when flow may be compromised by stenosis, an attempt to wire the SB should always be actively considered. A narrow angle bifurcation, bifurcations with ostial SB disease, and bifurcations with smaller SB reference diameters are most likely to occlude after MB stenting. Factors increasing complexity in SB wiring include severe proximal MV stenosis, ostial SB stenosis, steep angulation and
Predilation and stenting
Predilatation of the MB prior to stenting is the usual approach in patients with stable angina. Oversizing of the balloon should be avoided but it is important to observe optimal balloon expansion of the MV before stenting. When this does not occur, further lesion preparation and/or debulking is required before stent deployment. Routine SB dilation is unnecessary but in the presence of severe ostial stenosis of the SB it should be considered. Potential advantages of SB predilatation may include increased ostial SB lumen, facilitated rewiring of the SB after stenting and avoiding rewiring and post-dilatation of the SB after implantation of the MV stent12.
Disadvantages of SB predilatation include the risk of dissection with a potential increase in the requirement for SB stenting. Also, if the dilated SB ostium is not scaffolded by the MV stent, the risk of restenosis may be increased. Factors favouring SB predilatation include suboptimal SB flow after wiring, extensive calcification and extensive SB disease extending beyond the ostium.
Stent type and sizing
Permanent DES are recommended for bifurcation treatment. The principal mechanism of SB distortion and narrowing after MB stenting is shifting of the flow divider/carina. This can be minimised with careful stent sizing. Permanent DES should be sized according to the distal MV reference diameter. Choosing a stent where the platform accommodates expansion to the reference diameter of the proximal MV segment is required.
The proximal optimisation technique
Adequate apposition in the proximal MV is achieved by the proximal optimisation technique (POT). POT is performed by dilating the proximal MV stent from the proximal stent edge to just proximal to the carina, using a short oversized balloon. Appropriately sized non-compliant balloons may be selected for POT, but recent data suggest that semi-compliant balloons are able to expand contemporary stents and appose stent struts to the proximal vessel lumen in the absence of relevant atherosclerosis. POT facilitates SB access, reduces risk of accidental abluminal rewiring, lowers risk of stent distortion by catheter collision, and enhances scaffolding at the SB ostium. Thus, POT should be considered a standard step in bifurcation treatment (Figure 3).
Difficult SB rewiring after MV stenting
After stenting the MV, rewiring may be necessary if there is impaired SB flow. Difficult SB rewiring may be facilitated by modifying the distal guidewire tip, using a CTO wire such as the Fielder FC, Sion, or Fielder XT (all ASAHI Intecc, Aichi, Japan), or performing a new POT with higher pressure or a larger balloon if the first POT was inadequate. If SB rewiring is not possible, a bail-out technique is performed by leaving an uninflated balloon in the MV and advancing a low-profile 1.0 to 1.5 mm balloon catheter on the jailed wire (Figure 4). A “tunnel” can then be created to allow passage of an SB balloon. It is essential to ensure final re-expansion of the proximal MV stent. Re-crossing into the SB in the distal portion of the stent promotes better ostial SB stent coverage and apposition. This can be achieved by “pullback rewiring” by advancing the guidewire with a bent tip into the distal MV and then carefully retracting the wire while turning and directing it towards the SB. The position of the wire re-crossing may be verified by OCT13.
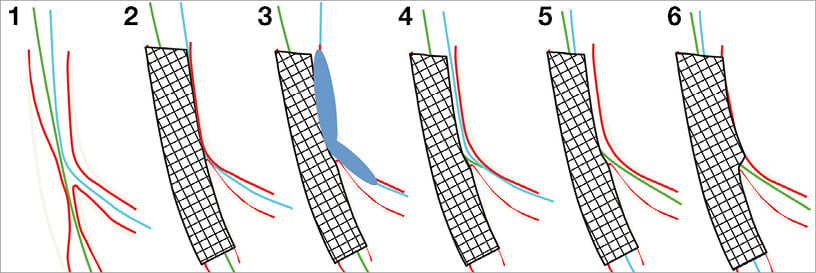
Figure 4. “Jailed wire” technique in case of impossible side branch (SB) access after main branch (MB) stenting. 1) Medina 1,1,0 lesion. 2) SB occlusion after MB stenting (stent too large leading to carina shifting). 3) Dilatation with a small balloon on the “jailed wire”, restoring the SB flow. 4) & 5) SB wiring from the MB stent and guidewire exchange. 6) Proximal optimisation technique (POT) and final kissing balloon inflation or POT followed by side branch dilatation and finalised with POT (POT-side-POT).
Kissing balloon inflations in simple stenting
Isolated dilation of the SB after MV stenting may cause partial or complete jailing of the MV and is inadvisable. Historically, a routine double balloon kissing strategy in single-stent treatment was considered. However, it is now clear that this routine approach has no clinical advantage despite the theoretical improvements in the restoration of bifurcation anatomy, expansion of the proximal MV, apposition of jailing struts and balloon dilation of ostial SB lesions. This lack of evidence of benefit of routine kissing balloon inflation probably reflects the increased procedural complexity, the risk of SB dissection and the potential for accidental stent crush by proximal abluminal rewiring distortion. Kissing is necessary and recommended when antegrade flow is impaired (TIMI flow <3), but, when flow is normal, discrete ostial SB pinching may not require further intervention and, prior to deployment of a further stent, use of a pressure wire can be considered. When SB pinching is discrete with normal flow, FFR measurement will usually reassure the operator that an SB stent is unnecessary. Often the acute ostial SB pinching will be caused by transient obstruction, speculated to be thrombus, plaque debris or vessel wall oedema, that may disappear over time.
Distortion of the MV stent after kissing inflations is common and might result in a suboptimal outcome. An optimised sequence including a final POT (rePOT) has shown favourable results compared to finalising with kissing balloon only in bench testing and modelling (Figure 5).
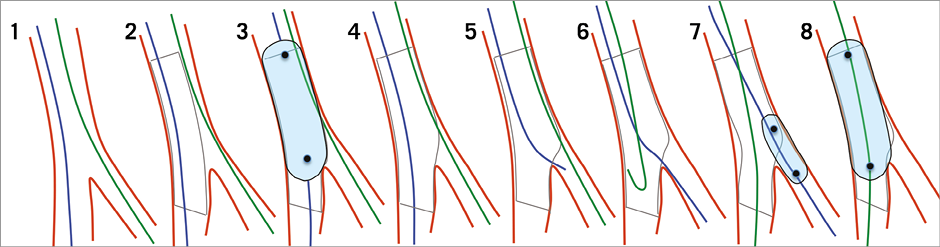
Figure 5. RePOT strategy. From 1 to 8: wiring both branches. Main branch (MB) stenting using a stent diameter according to the distal MB reference. Proximal optimisation technique (POT). After 4, the procedure can be stopped. If the side branch (SB) needs attention, wire exchange, wiring the SB through the MB distal strut. SB opening using a short non-compliant balloon in order to avoid SB dissection. Final POT in order to restore stent distortion opposite the SB.
Side branch stent implantation technique in provisional strategy
Stenting of the SB is indicated during the provisional approach: 1) when SB flow is compromised, 2) in the presence of a major SB dissection, or 3) when the SB is significantly diseased and large enough to lead to significant residual ischaemia. Occasionally, FFR interrogation may suggest whether SB stenting is desirable. The aspect of the SB ostial residual lesion may guide procedural technique (Figure 4, Figure 5).
SB T-stenting can be used in the majority of cases when SB dilatation is done properly through a distal strut, and ostial scaffolding with the MB stent is adequate for the conventional T technique without any overlap between the SB and the MV stent. Therefore, after SB ballooning, it is very important to assess the result at the SB ostium by a good angiogram with an optimal view, and, when in doubt, to use a stent enhancement technique or OCT in order to check SB ostium scaffolding. When the angulation is near 90 degrees, T-stenting should always be considered, as other techniques are associated with a high risk of stent malapposition. Precise deployment of the SB stent at the ostium requires an optimal view to avoid protrusion inside the MV stent or a gap between the two stents. If the SB ostium is not properly covered by the MV stent, an overlapping technique is necessary (T-and-protrusion [TAP], culotte or internal crush). When TAP is used, the SB stent is deployed with minimal protrusion into the MV while maintaining an uninflated balloon in the MV. After retraction of the SB stent balloon, kissing balloon dilatation is readily performed. This TAP technique eliminates the need for a second SB rewiring, but may produce a long metal carina in narrow angle bifurcations. More protrusion of the SB stent inside the MV stent represents the base for an internal mini-crush technique. This internal crush is fast and theoretically easier to rewire than classic and mini-crush, owing to the single jailing strut layer, but is limited by the maximum cell size of the main vessel stent, the risk of rewiring the true lumen of the SB stent again due to incomplete crush, and by the resulting triple strut layer often present in the proximal MV. The clinical outcome for patients treated by internal crush is unknown. Provisional culotte, with proximal overlap of two stents, can be used when a DES that accommodates the proximal MV size is available. Short stent overlap in the proximal MV and rewiring of the MV near the carina are recommended.
Kissing balloon inflation in two-stent techniques
In two-stent techniques, high-pressure ostial and MV dilatation is mandatory to achieve full stent expansion at both ostia, preferably by inflating the balloon in the SB first, followed by the balloon in the MV. Subsequently, a lower-pressure kissing inflation facilitates carina optimisation and a final POT should be considered. When performing kissing balloon dilation, it is clear that simultaneous deflation of both balloons is important to avoid distorting the MV stent. Use of short NC balloons for kissing balloon inflation in order to avoid stent distortion, obtain full expansion and avoid SB dissection is also recommended.
When is the provisional approach not appropriate?
The recent EBC II trial provides insight into the provisional technique vs. culotte two-stent technique in bifurcation lesions (SB ≥2.50 mm and more than 50% SB diameter stenosis): it confirms that a minority of bifurcation lesions requires a “two-stent strategy”. However, lesions with difficult wiring or large SB with extensive disease extending >5-10 mm beyond the bifurcation may be best approached electively with a two-stent technique14.
Planned two-stent techniques
Extensive experience by interventional cardiologists practising bifurcation interventions supports the concept that implanting DES in both the MV and the SB may safely treat a subgroup of bifurcated lesions. A wide (and growing) series of techniques to implant two stents in coronary bifurcation is available. Adequate procedural control, e.g., by meticulous use of imaging modalities and experience of the operator in effectively practising a particular double-stenting technique is probably more relevant as compared with the specific technique selection. Indeed, the final aim of a safe double-stenting strategy is to cover the diseased bifurcated vessel segments entirely by stent to warrant good scaffolding at critical areas including the side branch ostium using kissing balloon inflation (i.e., kissing inflation with documented appropriate expansion of the balloons) to limit stent overlap and avoid stent distortion. Due to the angiographic ambiguity and complexity of two-stent procedures, invasive imaging modalities such as IVUS and OCT may provide crucial information during procedure planning to ascertain anatomy and lesion preparation strategy, to check wire positions and lesion coverage after stent implantation, and to evaluate ascertained final stent and vessel expansion. As previously reported, various double-stenting techniques are available. Some of them have gained greater acceptance among the interventional community and are regarded as more conventional. Culotte, crush, and T/TAP are gaining popularity on the basis of either increasing scientific data or widespread clinical experience, whereas the extended number of non-apposed struts and the creation of permanent, double barrels in the proximal MV suggest reserving simultaneous kissing stent (SKS) techniques for rare conditions, e.g., emergency management of suitable bifurcation anatomies.
Culotte is a long-lasting technique whose efficacy has been documented in trials (NORDIC I, II, IV and BBC ONE) but has been questioned for distal LM bifurcation treatment15. Culotte may be practised in both intentional double-stenting procedures and in provisional procedures requiring SB stenting as a bail-out. In the case of intended double stenting, the first stent is usually implanted from the distal SB into the MV followed by distal MV rewiring and stent implantation from distal to the proximal MV. On the other hand, in the setting of provisional stenting, the SB stent is the second stent to be implanted after MV stenting and kissing ballooning. The main limitation of culotte stenting is the possible presence of major mismatch between the size of the proximal MV and SB. Thus, two aspects are recognised as critical, the stent platform selection and the application of POT during the procedural flow. Indeed, stent selection should require full awareness of the specific expansion potential in order to avoid major malapposition in the MV. Furthermore, since relevant degrees of malapposition are expected to occur during the procedure at the level of the proximal MV, early correction by POT may facilitate the procedure course and prevent technical troubles.
Crush has evolved over time. After its first description by Colombo, a series of improvements was reported. Its clinical performance is now recognised to be highly dependent on technical factors such as the success in ending up with a final kissing inflation. According to the results of recent Chinese trials conducted by highly experienced crush-dedicated operators, excellent clinical performance for the so-called DK crush technique was reported16. Expert operators agree that a “modern” way to perform crush is based on the following combination of technical refinements: 1) limiting the length of the crushed stent segment (mini-crush) during stent implantation in the SB, 2) the use of an MV balloon (instead of directly implanting the MV stent) to crush the SB stent (step-crush), and 3) the performance of a first kissing balloon inflation after stent crush in order to push away the first layer of stent struts from the SB orifice and fully appose the struts on the carina side (securing wire re-crossing towards the SB), thus increasing the rate and success of final kissing inflation (DK crush).
The TAP technique represents an emerging refinement of T stenting aimed at ensuring both full ostium coverage and final kissing inflation17. Ease of practice, full compatibility with 6 Fr guiding catheters, suitability for both bail-out SB stenting and elective double stenting, and “inverted” TAP by implanting the first stent from the SB into the proximal MV are factors likely to increase TAP popularity. However, a recognised limitation of the TAP technique is the creation of a single layer neocarina which may be more pronounced in the case of acute-angled bifurcations. Such a metallic neocarina is an unnatural structure in the bifurcation core segment with the risk of late endothelialisation and jailing of the MV. For such reasons, dedication to limit protrusion while implanting the SB stent is critical, as well as kissing balloon inflation as a final step in branch post-dilation or treatment of TAP restenosis. Selection of the technique should be influenced by the angle, as culotte and crush techniques are associated with stent distortion in T-shape angulations while TAP is associated with a long carina in Y-shape angulations (Figure 6).
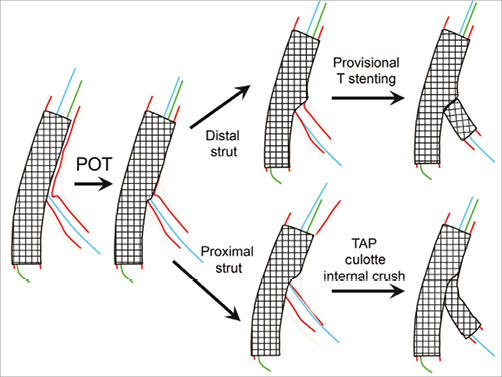
Figure 6. Proximal vs. distal strut side branch rewiring in provisional double-stent techniques. When the angulation between the main vessel and the side branch approaches 90 degrees, provisional T-stenting is recommended and might be best supported by rewiring through the distal struts (upper right). In lesser angle bifurcations, provisional culotte, TAP or internal crush techniques may be preferred. These techniques are better supported by rewiring through the proximal struts (lower right).
0,0,1 treatment
Treatment of Medina 0,0,1 lesions has not been well investigated. A true isolated lesion located at the SB ostium is relatively rare and is even less common if such angiographic lesions are investigated by: 1) invasive imaging such as IVUS or OCT, since extension of atherosclerotic disease to the MV is often disclosed, or 2) FFR, as short ostial non-Cx lesions are often FFR negative. Due to the risk of impairing the MV during PCI for 0,0,1 lesions, the absence of significant ischaemia or symptoms may indicate a conservative management with optimal medical therapy. Different technical options have been suggested for PCI of 0,0,1 lesions. Promising preliminary results have been reported by treating such lesions with an “inverted” provisional technique based on DES implantation from the proximal MV towards the SB with final kissing balloon to provide full distal MV patency18. Other technical options adopted so far include the use of the Tryton stent (Tryton Medical, Durham, NC, USA) alone19, cutting or scoring balloon, drug-eluting balloons or, more recently, BRS. Nevertheless, the absence of head-to-head comparisons and the limited number of reports make the treatment of Medina 0,0,1 an ideal topic for future investigations.
PCI or CABG for distal left main bifurcation lesions
There is increasing evidence that percutaneous coronary intervention (PCI) with drug-eluting stents (DES) is an equal revascularisation alternative to coronary artery bypass surgery (CABG) in patients with significant left main (LM) disease20-25. The recently published guidelines on myocardial revascularisation from the European Society of Cardiology/European Association for Cardio-Thoracic Surgery26 have upgraded the indication for PCI in patients with a low SYNTAX score and significant LM disease to a class Ib indication. The level of evidence for PCI for LM disease in patients with a SYNTAX score of 22-33 is class IIa. For a SYNTAX score ≥33 the recommendation is still class III.
The ongoing EXCEL (Evaluation of XIENCE Everolimus Eluting Stent Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization [ClinicalTrials.gov identifier: NCT01205776]) and NOBLE (coronary artery bypass grafting vs. drug eluting stent percutaneous coronary angioplasty in the treatment of unprotected left main stenosis [ClinicalTrials.gov identifier: NCT01496651]) trials may strengthen the level of evidence further by clarifying the role of the latest generation of DES in the treatment of LM disease27. Accordingly, an increasing number of patients, especially those with a low or intermediate complexity score, or those at high surgical risk, are expected to be treated by PCI for LM disease in the near future.
Differences between the LM and other bifurcations
The LM is the largest bifurcation of the coronary tree and has a number of unique features, which may demand different technical approaches from non-left main bifurcations28. The most important differences are the following. 1) The myocardium supplied by the LM generally accounts for considerably more than 50% of the total myocardial mass. 2) The SB is most often the circumflex artery (Cx) which generally has a large diameter, and is not always easy to access. Occlusion of the Cx is not acceptable since it often results in ischaemia of a large myocardial territory and may induce acute ischaemic mitral regurgitation. 3) The LM is the only bifurcation where the proximal MB originates directly from the aorta. 4) The proximal reference diameter generally measures between 4.5 and 5.5 mm - close to, or above, the dilatation limit of most currently available coronary stents. 5) Trifurcations are encountered in about 10% of cases29,30 and may require specific treatment strategies. 6) The bifurcation angle is generally T-shaped, which may have an impact both on technique and on prognosis after stenting31,32 (Figure 6).
EBC consensus of LM treatment and techniques
As for all bifurcation lesions, a provisional SB stenting approach is recommended in most cases. Specific technical problems unique to the LM can be solved by systematic use of two or three wires at the beginning of the procedure, by proper stent selection and positioning, and by liberal use of the POT technique. Distal bifurcation disease can be treated by either a one-stent (provisional strategy) or a two-stent technique. Data from observational non-randomised studies suggest that the provisional strategy, when feasible, is superior to a two-stent technique with regard to the rate of target lesion revascularisation (TLR) in two-stent procedures. Because of the T-shape angulation, the T or TAP technique is recommended in the majority of double-stenting cases (Figure 6).
The European Bifurcation Club Left Main (EBC MAIN) Study
EBC MAIN is the first randomised clinical trial to compare single versus dual stenting strategies for the treatment of true bifurcation distal LM coronary artery lesions. It is a prospective, multinational, randomised clinical study of LM stem true bifurcation lesions (type 1,1,1 or 0,1,1: both left anterior descending and circumflex artery >2.75 mm diameter) promoted by the EBC group. The study hypothesis is that LM coronary bifurcation lesions are best treated with a planned single-stent strategy rather than a planned dual-stent strategy, with respect to death, TLR and myocardial infarction at one year. A total of 450 patients will be enrolled and treated with either a planned single or a planned dual zotarolimus-eluting stent strategy according to randomisation. The primary study endpoint is a composite of death, myocardial infarction and TLR at 12 months. Secondary endpoints are death, myocardial infarction, and TLR, each at 12 months, and angina status, stent thrombosis, death, myocardial infarction, TLR at three- and five-year clinical follow-up.
Intracoronary imaging in bifurcations
Angiographic assessment of bifurcations has several limitations calling for a low threshold for use of intravascular ultrasound (IVUS) or optical coherence tomography (OCT). When treatment complexity increases so does angiographic ambiguity, as overlapping stents, some bioresorbable stents, wire positions, the SB ostium and thrombus are not readily assessed by angiography. OCT provides superior images of the lumen surface, calcium, predilatation results, stent positions, wires and the SB ostium from both MV and SB pullbacks, but OCT may increase the use of contrast and does not allow aorto-ostial assessments33. IVUS allows better characterisation of plaque burden and does not require optimal vessel flushing during acquisition. The feasibility and role of HD IVUS in bifurcation assessment has not yet been determined. Re-crossing a jailed SB with IVUS or OCT wires is not recommended, as the high profiled and rather stiff wires might distort or fracture the stent34 or could be trapped. IVUS and OCT enable lesion assessment, evaluation of predilatation, reference sizing and evaluation of adequate vessel and stent expansion after stenting35-39. Lesions proximal or distal to the SB have been shown to affect the risk of SB compromise after MV stenting40,41. Careful evaluation of wire positions after stent rewiring is beneficial to ensure optimal SB re-crossing42-44 and to exclude accidental abluminal rewiring. The feasibility of IVUS in evaluation of wire positions is unknown. As the constraints of the C-arm of the angiographic system prevent optimal assessment of the Cx ostium in about 40% of cases, careful evaluation of the Cx ostium by intravascular imaging may be of clinical importance in such cases. IVUS has been shown not to enable precise SB evaluation from MV pullbacks whereas OCT capabilities in this regard are promising.
– OCT and IVUS may be of particular value in guiding bifurcation treatment due to high degree of angiographic ambiguity.
– IVUS is recommended for LM bifurcation treatment and OCT may be used with the provision that aorto-ostial assessment is most often not possible.
– OCT may be superior to IVUS in evaluation of the SB ostium, stent positions, stent strut malapposition, wire position, and detection of thrombus.
– Wire positions in stent re-crossing affect stent appositions and can be evaluated by OCT.
– Accidental abluminal stent rewiring is a concern and may be ruled out by OCT.
– Pullbacks in both MV and SB are recommended when guiding two-stent treatment by intravascular imaging.
Quantitative coronary analysis (QCA) for bifurcations
QCA is an important standard analysis in scientific reporting and for regulatory assessment. Analysis of bifurcations by 2D QCA requires dedicated bifurcation software45-49. Use of 3D bifurcation QCA improves the accuracy of quantitative measurements including bifurcation angulations50-53. Present 3D QCA systems further provide the optimal projection angle in bifurcations54 and form the backbone for co-registration to OCT and IVUS55 and for virtual FFR computation without the use of pressure wires56-58, such as the presented QFR technology (Hans Reiber, EBC 2015).
QCA software dedicated to bifurcations is recommended.
3D QCA improves quantitative measurements compared to 2D QCA.
QCA may aid stent sizing during intervention but clinical value remains unknown.
Role of fractional flow reserve (FFR) in bifurcations
MV FFR is recommended in stable patients when no other objective evidence of ischaemia is available59.
FFR in large SBs before intervention may be used to support choice of treatment strategy but careful interpretation of measurements is required.
SB FFR after MV stent implantation remains controversial due to potential safety concerns60,61 and due to unknown validity when performed after MV stenting60,62. Cx evaluation by FFR after MV implantation was however shown to reduce SB intervention without increasing subsequent revascularisation.
Dedicated devices
During the last decade, devices dedicated to bifurcation lesion PCI have been developed but most of them did not enter routine clinical practice. Yet, several devices raised the interest of some operators: a series of interesting experiences has been presented and discussed at the EBC meetings. Of note, during 2015, the first large multicentre randomised trial on a dedicated device was published. In the TRYTON trial, 704 patients with non-LM, true coronary bifurcation lesions (recruited in 30 European and 28 US centres) were randomised to a Tryton-facilitated culotte technique or to a provisional technique with an everolimus-eluting stent63. At nine months, the primary endpoint (target vessel failure) was 17.4% in the Tryton group compared with 12.8% in the provisional group. Such a primary endpoint difference was not within the pre-specified non-inferiority margin; it was concluded that provisional stenting should remain the preferred strategy for treatment of non-LM true coronary bifurcation lesions. Such disappointing results of this first trial suggest that the impressive safety and efficacy reached by provisional stenting with latest-generation DES make the role of dedicated stents for non-LM lesions quite limited. Based on this, the EBC consensus was in favour of highlighting the treatment of LM bifurcation, due to its specific anatomic complexity, as the main field, which may theoretically benefit from technical improvements of dedicated devices. Early experiences with some dedicated devices with different principles of action have been reported64-66. However, carefully designed studies of dedicated devices for LM lesions are advocated.
Bioresorbable stents (BRS) in bifurcation lesions
The use of bioresorbable stents (BRS) may offer potential advantages compared with metallic DES for bifurcation PCI. However, intrinsic limitations of currently available devices, such as the strut thickness and limited expansion capacity, as well as the signals for increased early and late BRS thrombosis, are influencing the adoption of BRS as a standard treatment option.
Bench studies have indicated that the DESolve® BRS (Elixir Medical, Sunnyvale, CA, USA) could be more suitable for bifurcation treatment compared with the Absorb BRS (Abbott Vascular, Santa Clara, CA, USA), but clinical experience in bifurcation is only available using the Absorb BRS. As the randomised trials on Absorb excluded bifurcations with side branches ≥2 mm diameter, the EBC consensus statements are based on bench-testing data and initial clinical results from non-randomised registries and represent a revision of the EBC recommendations for metallic DES3,67-69.
Provisional strategy using BRS
The provisional strategy remains the default technique for bifurcation treatment using BRS2. Careful MV predilatation is required. Verification by fully expanded 1:1 sized non-compliant balloon is recommended.
STENT SELECTION
The expansion capacity of the Absorb BRS allows post-dilatation up to 0.5 mm above the nominal diameter according to the instructions for use, and, in bench-testing, the MV post-dilatation safe threshold without fracture for Absorb was 3.8 mm at 20 atm for the 3 mm BRS3,6. Thus, to permit post-dilatation of the proximal MV segment, the nominal size should preferably be 0 to 0.5 mm below the proximal MV reference size3,55. It is unknown whether Absorb allows large, abrupt diameter changes between the proximal and distal MV, so caution is recommended in such cases. The BRS deployment sequence should follow the instructions for use.
PROXIMAL OPTIMISATION
POT is recommended, with non-compliant (NC) or semi-compliant balloons not exceeding a maximal size of 3.8 mm for the 3.0 Absorb BRS according to the chart of the balloon and 4.2 mm for the 3.5 mm Absorb BRS6. For side branch dilatation of a 3.0 mm Absorb BRS by a 3.0 mm NC balloon, the threshold before the Absorb BRS fractured was 10 atm in bench-testing70,71. Final POT with an adequately sized NC or semi-compliant balloon should be performed by the sequential strategy: POT+SB opening+final POT5.
Traditional kissing balloon dilatation (FKBD) is not recommended. BRS distortion could be corrected by final POT or by mini-kissing balloon post-dilatation (mini-KBPD or snuggle balloon dilatation, depending on the length of SB balloon protrusion) and low-pressure inflation (safe threshold at or below 5 atm)5. Intravascular imaging, preferably OCT, is recommended for procedural guidance3.
Two-stent techniques using Absorb BRS
Bench studies and anecdotal cases demonstrated the feasibility of various two-stent techniques utilising either two BRS or a combination of BRS and DES3. With the present level of evidence, it is not recommended to perform routine two-stent techniques using BRS outside carefully protocolled studies.
When SB stenting is required as a crossover from provisional, metallic DES or BRS implantation on the SB should be considered utilising preferentially the T-stenting technique3.
Due to the major differences in platform properties, strut thickness, radial strength and resorption time, it is unknown whether the above-described recommendations apply to other BRS to be introduced shortly.
Conclusion
The present 11th EBC consensus document represents the summary of the current consensus and clinical recommendations of the EBC. It points to the fact that there is a multitude of strategies and approaches to bifurcation stenting within the provisional strategy as well as in all the different two-stent strategies. The recommendations cover a moving target. Much more scientific work is needed to support the continuous improvement of the treatment of bifurcation lesions in coronary artery disease.
Conflict of interest statement
The authors have no conflicts of interest to declare, but all the authors are core members of the European Bifurcation Club.