Abstract
The 15th European Bifurcation Club (EBC) meeting was held in Barcelona in October 2019. It facilitated a renewed consensus on coronary bifurcation lesions (CBL) and unprotected left main (LM) percutaneous interventions. Bifurcation stenting techniques continue to be refined, developed and tested. It remains evident that a provisional approach with optional side branch treatment utilising T, T and small protrusion (TAP) or culotte continues to provide flexible options for the majority of CBL patients. Debate persists regarding the optimal treatment of side branches, including assessment of clinical significance and thresholds for bail-out treatment. In more complex CBL, especially those involving the LM, adoption of dedicated two-stent techniques should be considered. Operators using such techniques have to be fully familiar with their procedural steps and should acknowledge associated limitations and challenges. When using two-stent techniques, failure to perform a final kissing inflation is regarded as a technical failure, since it may jeopardise clinical outcome. The development of novel technical tools and drug regimens deserves attention. In particular, intracoronary imaging, bifurcation simulation, drug-eluting balloon technology and tailored antiplatelet therapy have been identified as promising tools to enhance clinical outcomes. In conclusion, the evolution of a broad spectrum of bifurcation PCI components has resulted from studies extending from bench testing to randomised controlled trials. However, further advances are still needed to achieve the ambitious goal of optimising the clinical outcomes for every patient undergoing PCI on a CBL.
Visual summary. 15th consensus document from the European Bifurcation Club.
Introduction
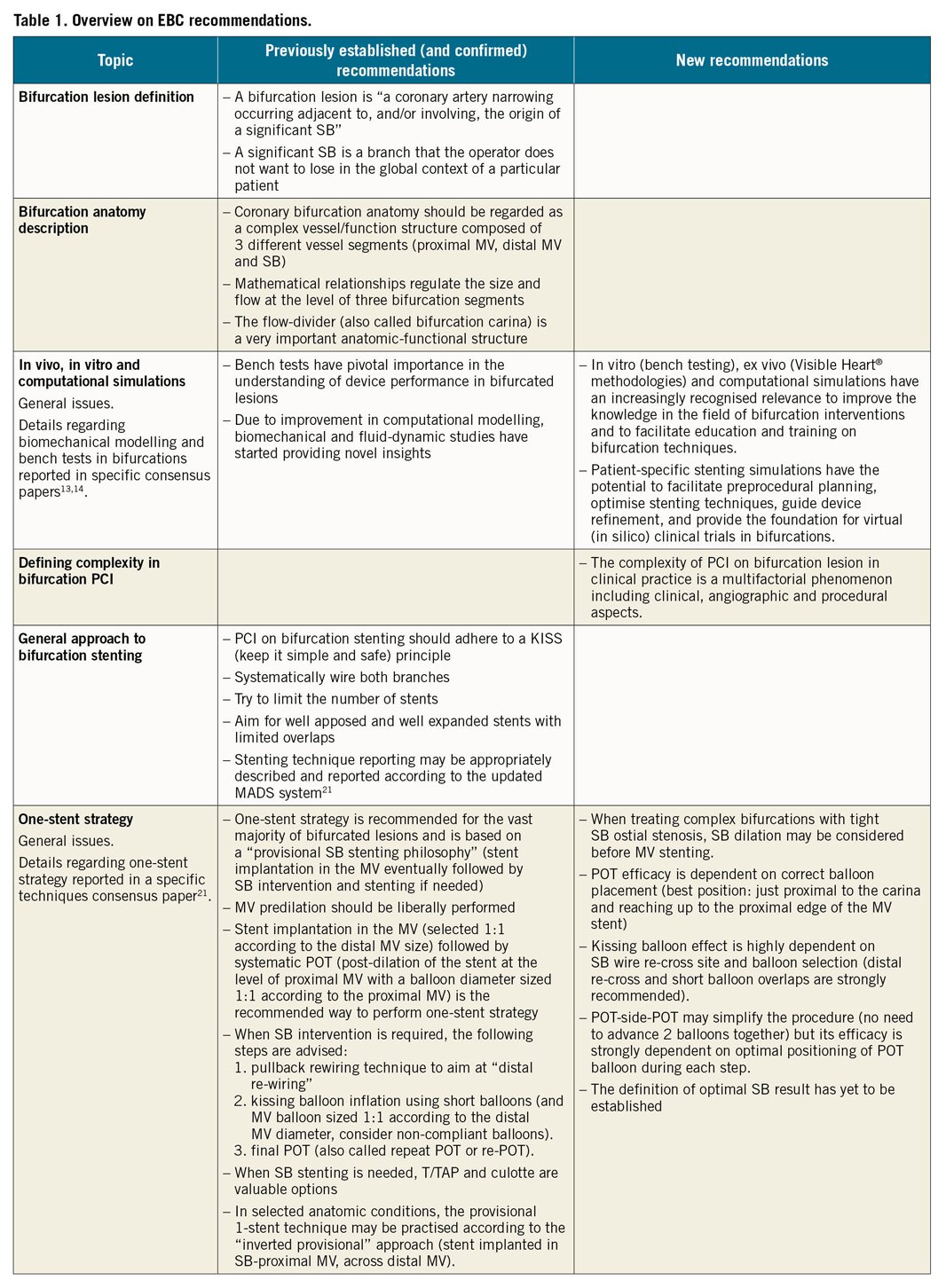
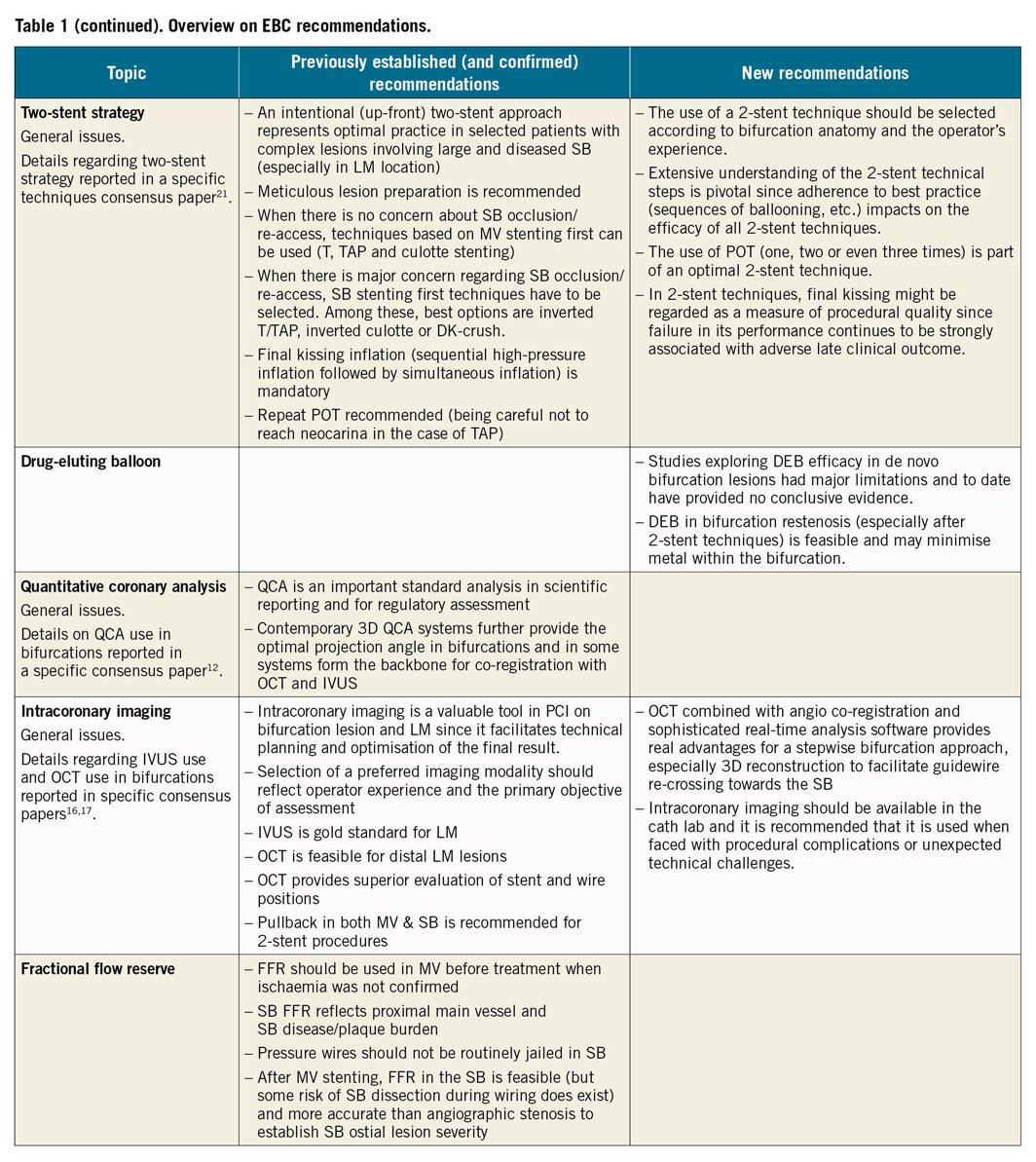
Since 2004, the European Bifurcation Club (EBC) has continuously promoted the improvement and standardisation of percutaneous coronary intervention (PCI) for coronary bifurcation lesions (CBL) and left main (LM). The annual meeting constitutes a unique opportunity for a comprehensive overview of the available data and incorporates “pro et con” debates (that are followed by electronic voting sessions involving all attendees) to facilitate generation of consensus statements. The 15th EBC meeting was held in Barcelona on 18-19 October 2019 and all presentations are freely accessible on the EBC website (https://bifurc.eu/). The present document reports the updated EBC consensus. Table 1 summarises the recommendations (established and new as compared with the previous documents1,2,3).
IMAGING IN BIFURCATIONS: LATEST EFFORTS ARE GOING TO PROVIDE NOVEL INSIGHTS
Intracoronary imaging use represents an important and promising aspect of CBL PCI. The EBC recently released documents on the specific issues related to intravascular ultrasound (IVUS)4 and optical coherence tomography (OCT)5.
Selection of a preferred imaging modality should reflect operator experience and the primary objective of the assessment. It is acknowledged that many operators have greater IVUS experience, and IVUS is favoured for ostial LM and large-vessel evaluation. However, the superior resolution of OCT provides potential advantages for specific steps of bifurcation interventions, including visualisation of the site of guidewire crossing and stent optimisation tools. Finally, the recently released high-definition IVUS is an attractive evolution of IVUS technology that combines high-resolution imaging with image depth; its utility in bifurcation stenting has still to be established.
Calcium, a key determinant of stent optimisation, is easily recognised by IVUS and OCT. Novel OCT criteria predicting stent underexpansion have been recognised: circumferential calcium (>180°), longitudinal extension >5 mm and calcium thickness >0.5 mm6. Algorithms to guide the selection of calcium modification tools have started to be developed7 but deserve clinical validation. Of note, data regarding best management of calcification in the setting of CBL are lacking, so that calcium recognition and lesion preparation should not differ from non-CB and may include debulking techniques such as rotablation and balloon lithotripsy.
Advances in OCT imaging processing now facilitate real-time analysis of stent-vessel interactions and precise location of guidewire crossing through stent side cells into the side branch (SB). In particular, a recent study documented that the position of “link” struts across SB ostia, a phenomenon that cannot be controlled by the operator during stent implantation, is associated with incomplete stent apposition after kissing8. After stenting, the assessment of adequate stent expansion and “landing”, together with the recognition of edge dissections, may guide further PCI optimisation5.
Two independent trials are assessing the impact of OCT guidance in bifurcation PCI. The ongoing OCT optimised bifurcation event reduction (OCTOBER) study is a large randomised trial aimed at assessing clinical superiority (two-year major adverse cardiac events) of OCT-guided stent implantation compared to standard angiography-guided implantation in bifurcation lesions9. The online three-dimensional optical frequency domain imaging to optimise bifurcation stenting using Ultimaster stent (OPTIMUM) study is a proof-of-concept randomised trial (endpoint: malapposed struts) comparing online three-dimensional OCT-guided PCI to angiography-guided PCI in bifurcation lesions treated by provisional stenting with kissing inflation10.
IN VITRO, EX VIVO AND COMPUTATIONAL SIMULATIONS
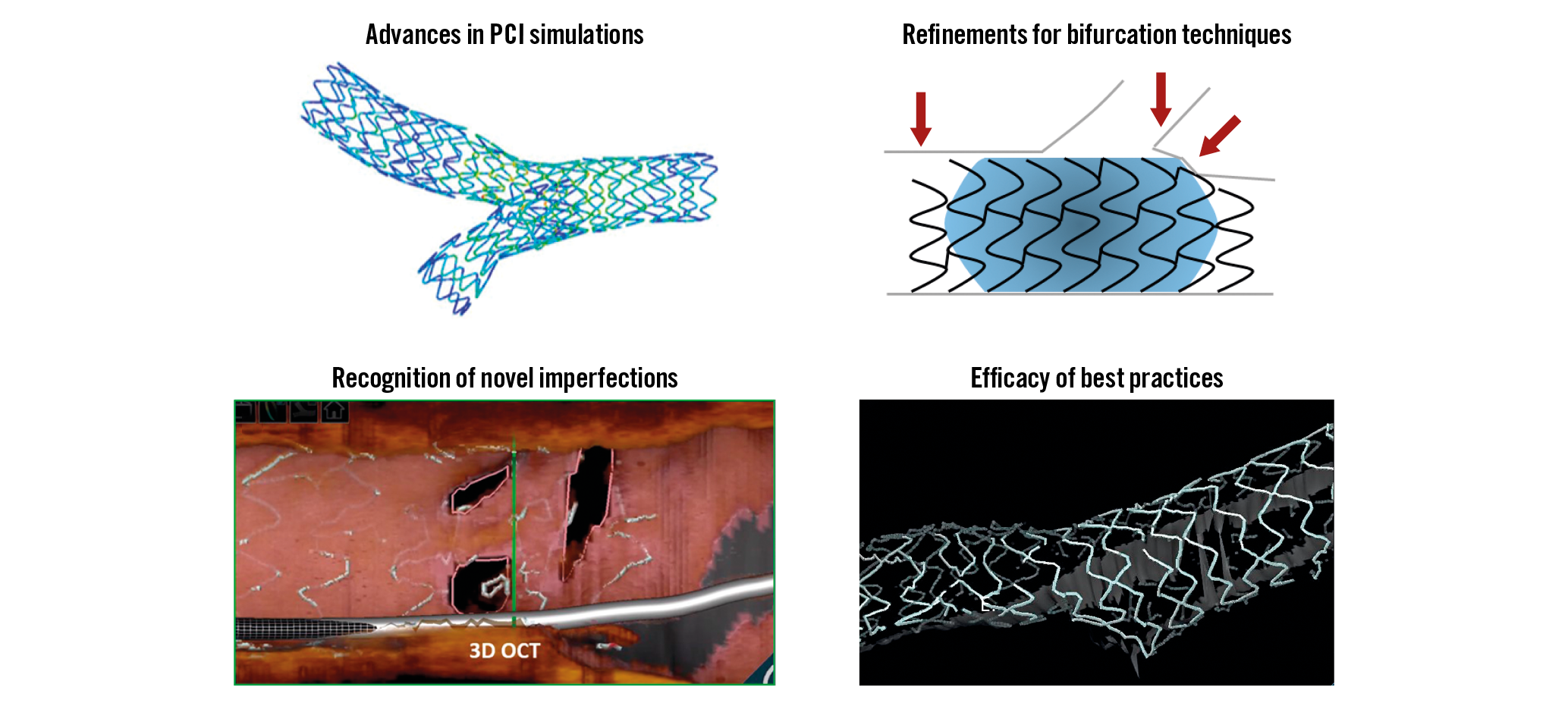
The last EBC meeting placed special emphasis on bifurcation stenting simulations and the use of advanced technologies, including artificial intelligence, machine and deep learning, and extended reality (virtual, augmented and mixed), to facilitate precision and planning of bifurcation interventions11,12.
Three types of stent simulation were discussed - in vitro (bench), ex vivo (Visible Heart® methodologies) and computational.
In vitro simulations represent bench testing of bifurcation stenting using patient-specific silicone-based bifurcation anatomies coupled with experimental flow dynamics and imaging (micro CT)13. There is potential to explore how flow changes in different coronary anatomies, and to explore how stent designs and deployment techniques may optimise flow.
Ex vivo simulations represent experimental stenting of porcine or cadaveric human donor hearts14 in a sophisticated perfusion circuit (Visible Heart® methodologies; http://www.vhlab.umn.edu/) eventually combined with invasive (OCT) or non-invasive (micro CT) imaging.
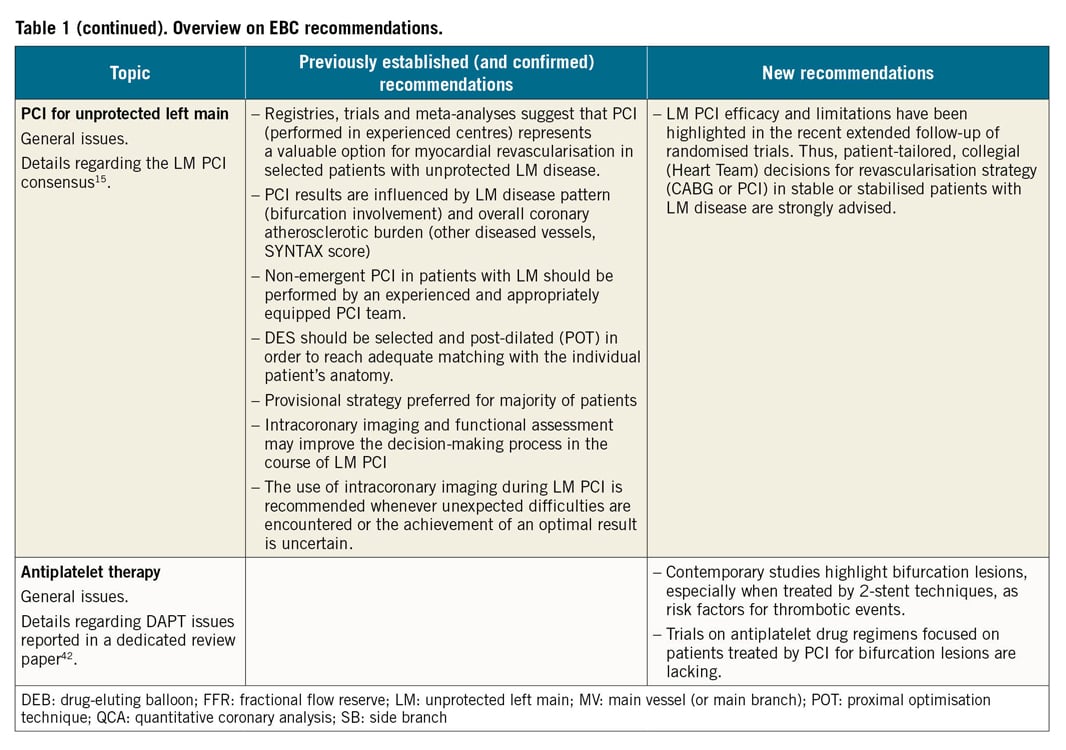
Computational simulations involve computational (virtual) stenting using patient-specific bifurcation anatomies, and realistic plaque, stent and balloon geometries and material properties coupled with computational fluid dynamics and solid mechanics15 (Figure 1). Computational simulations run in computer clusters. They are feasible, widely applicable, accurate, time-effective, and potentially cost-effective. Accordingly, patient-specific stenting simulations are anticipated to shift the future evolution of coronary bifurcation interventions and to offer valuable tools for education and training.
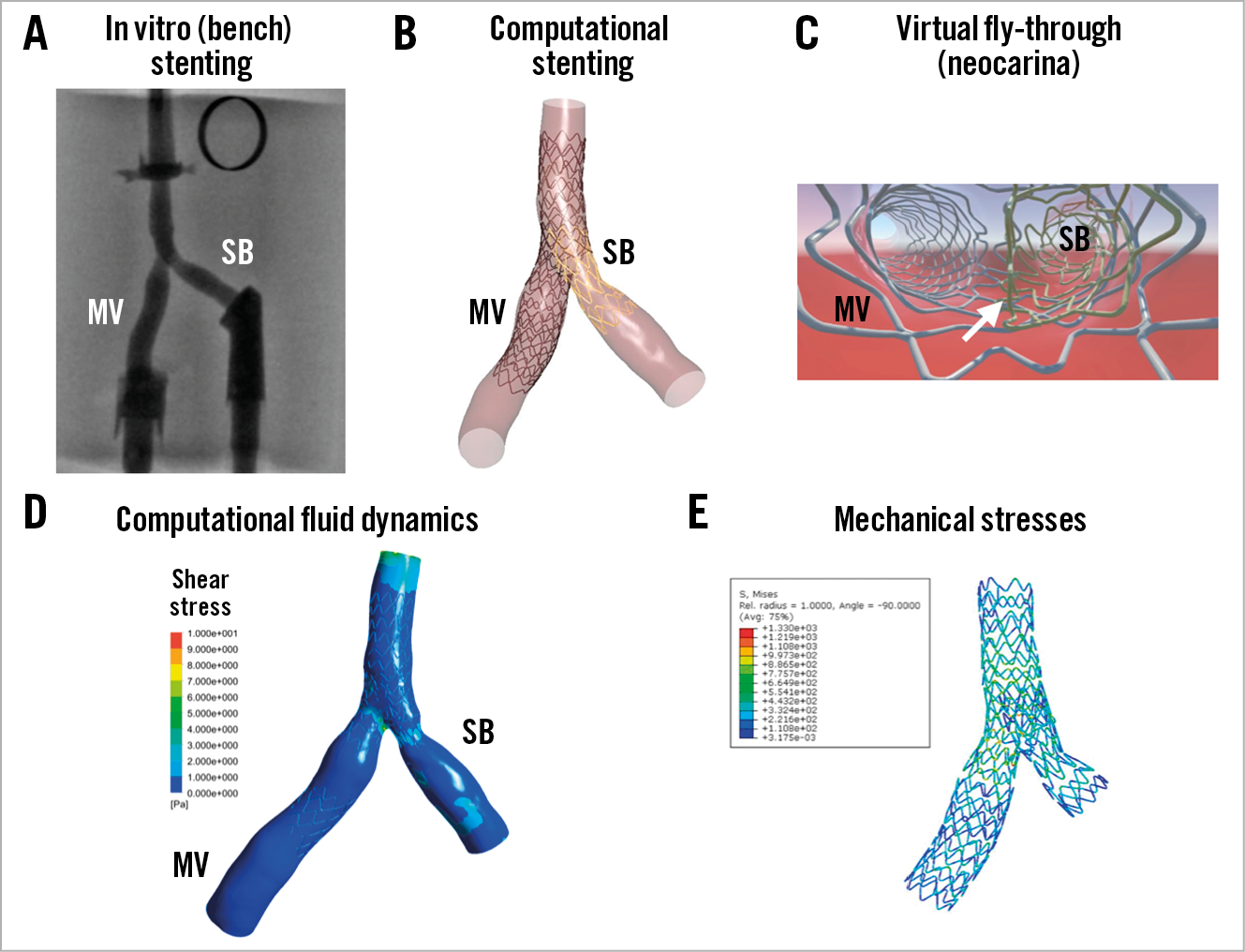
Figure 1. Example of in vitro and computational stenting simulations using a patient-specific coronary bifurcation anatomy. A) In vitro stenting of a patient-specific coronary artery bifurcation (TAP with a long neocarina denoted by the white arrow in panel C)). B) Computational simulation of the same stenting technique in the same bifurcation anatomy. C) Virtual fly-through view of the neocarina. D) Computational fluid dynamics of the stented bifurcation. E) Von-Mises stress distribution.
WHAT DEFINES A COMPLEX BIFURCATION LESION?
To date, no unique definition for a “complex” CBL exists within the literature. The historical “Medina” bifurcation classification, endorsed by the EBC, allows easy description of the angiographic plaque distribution and is known to influence the occurrence of procedural complications and adverse clinical events16. Medina 1,1,1 and Medina 0,1,1 have been regarded as complex CBL subsets in some studies. However, SB lesion length17, SB take-off angle and plaque composition (calcification, thrombus) are important modulators of CBL PCI complexity. In keeping with such a perspective, the definitions and impact of complex bifurcation lesions on clinical outcomes after PCI using drug-eluting stents (DEFINITION) registry18 generated a multi-parametric system where major criteria and minor criteria have been combined to categorise simple and complex CBL. This classification has recently been used for patient selection in the two-stent vs. provisional stenting techniques for patients with complex coronary bifurcation lesions (DEFINITION II) trial19.
Overall, a series of clinical, anatomic and procedural factors might combine to determine the technical difficulties and complication risk in an individual patient (Figure 2).
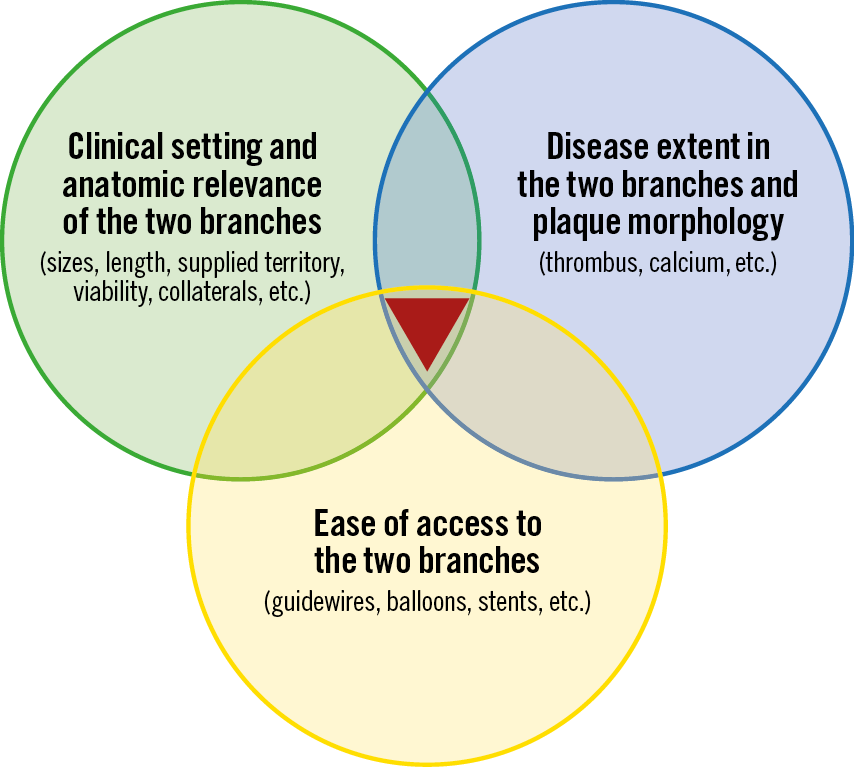
Figure 2. Main determinants of bifurcation PCI complexity.
MAJOR CONTROVERSIES REGARDING DECISION MAKING IN THE CONTEXT OF A ONE-STENT STRATEGY
Implantation of a main vessel (MV) stent (sized according to the distal MV diameter) across the SB ostium (“crossover” stenting) followed by the proximal optimisation technique (POT) is the minimal recommendation for a one-stent strategy in CBL. Of note, bench tests demonstrated that superior results from POT are obtained when the balloon is positioned immediately proximal to the carina20. Incorrect placement of the POT balloon too proximal or distal is associated with suboptimal results, as shown in Figure 3. Details regarding the technical aspects of the one-stent technique have been provided elsewhere21. During the last EBC meeting, the following key issues regarding a one-stent strategy were debated.
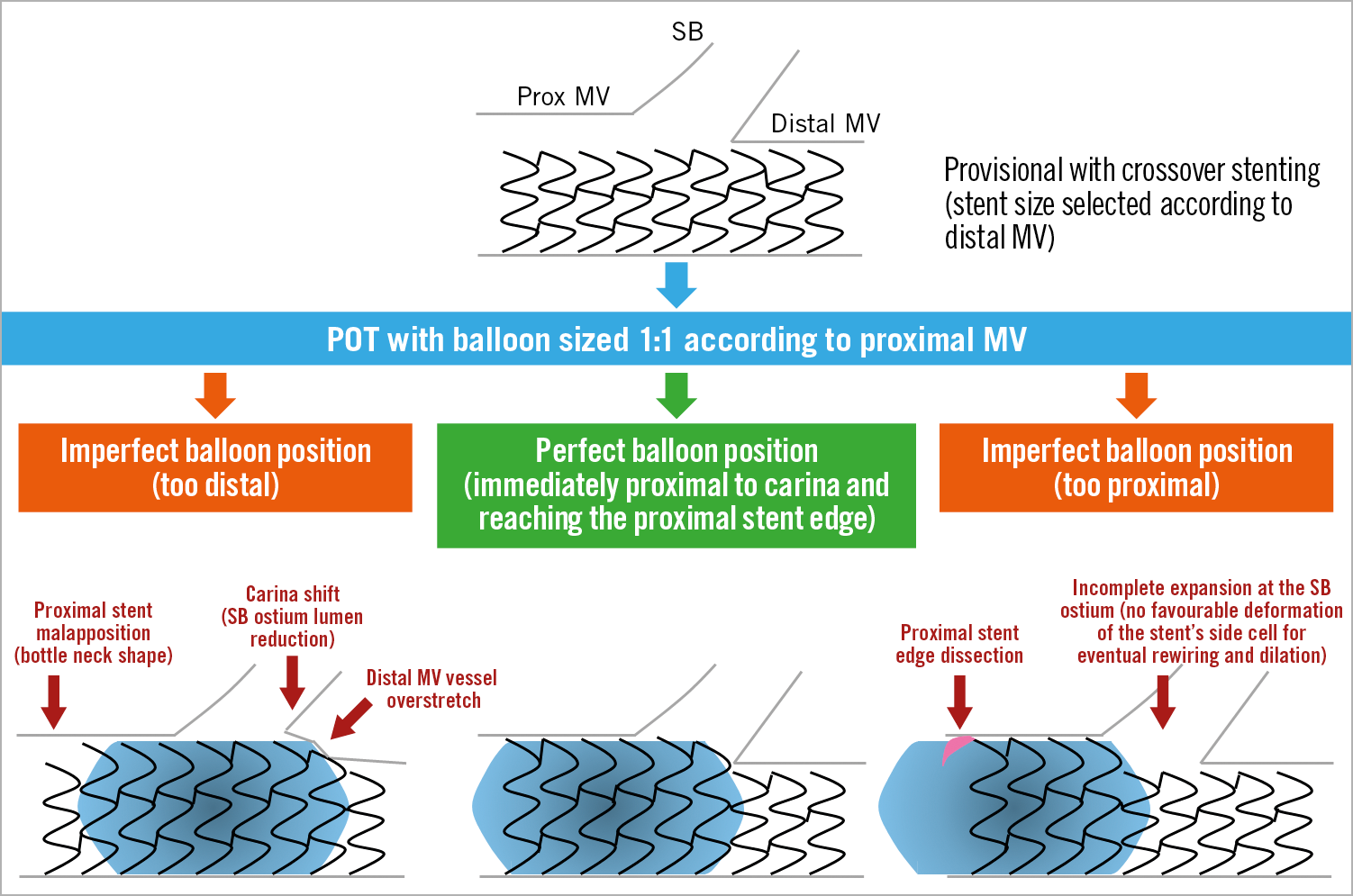
Figure 3. Possible consequences of incorrect balloon position during POT.
WHAT ABOUT DISEASED SIDE BRANCH PREDILATION?
When applying a provisional approach to CBL with extensive atherosclerosis involving both the MV and SB take-off, the question of optimal lesion preparation represents a major issue since the SB may occlude after MV stenting. A prospective randomised study on “true” CBL by Pan et al documented that SB predilation results in improved flow after MB stenting and less need to treat the SB subsequently22.
The standard practice for CBL dilation in complex lesions is sequential dilation of the MV and SB. However, simultaneous dilation (“pre-kissing” technique) has the potential to avoid bifurcation carina displacement during predilation at the risk of proximal MV overstretch and dissection. The pre-kissing technique with undersized balloons (to limit dissections) was recently reported to be associated with a lower incidence of SB-associated complications in a small observational study23. However, these findings are regarded as inconclusive.
WHAT IS THE BEST TREATMENT OF OSTIAL LEFT ANTERIOR DESCENDING OR CIRCUMFLEX ARTERY LESIONS?
The optimal management of ostial left anterior descending (LAD) or ostial left circumflex artery (LCX) lesions (also called Medina 0,1,0 and 0,0,1 LM bifurcations) is an unresolved issue. Of note, angiography is known to underestimate LM bifurcation atherosclerosis extension4,5, so that IVUS or OCT confirmation of isolated LAD/LCX stenosis is advisable before ostial stenting is considered.
A recent study compared treatment with one stent positioned precisely at the LAD ostium with crossover stenting, showing the feasibility of ostial stenting24. However, higher restenosis as compared with crossover stenting24 was documented. Thus, ostial stenting might be considered in order to avoid LM stenting when the anatomy is particularly favourable (rectangular angle between LAD-LCX, perfect visualisation of SB take-off, non-diseased LM). In all other situations, crossover stenting (covering the involved ostial LAD or ostial LCX and the diseased segment of LM) followed by POT and eventual kissing (according to either provisional or “inverted” provisional21) represents a preferable option.
WHEN TO PERFORM SIDE BRANCH DILATION DURING ONE-STENT STRATEGY FOR DISTAL LEFT MAIN?
Whether to perform SB dilation after crossover stenting in an unprotected LM is a challenge in daily practice. According to the “provisional” strategy, SB intervention is recommended whenever the result in the SB is considered suboptimal. However, defining a “suboptimal” result for the LCX ostium is difficult and not standardised (Supplementary Table 1 for overview of suboptimal SB result criteria adopted in recent studies).
Even in the absence of a suboptimal SB result, the need to clear stent struts from the SB ostium, facilitating access to the LCX, continues to be debated. Indeed, “floating” struts across the ostium may support the development of an LCX ostial “fenestrated” restenosis (Figure 4). Contrary to this concern, a large registry of patients treated with crossover stenting from the left main coronary artery (LMCA) to the LAD has demonstrated that the cumulative five-year incidence of target lesion revascularisation was not significantly different between the kissing and non-kissing balloon groups25.
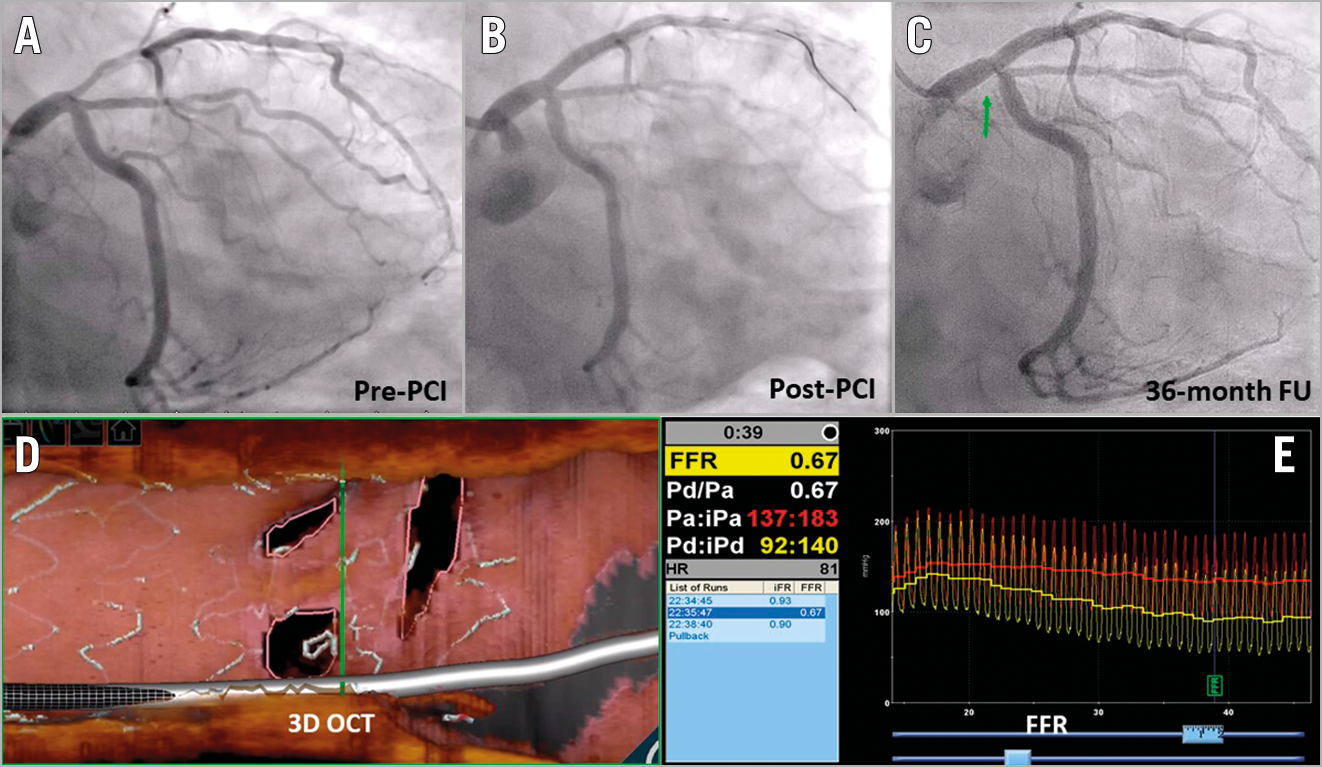
Figure 4. “Fenestrated” restenosis after crossover stenting. A) Pre-PCI angiography. B) Result after stent implantation into the LM-LAD followed by POT. C) 36-month follow-up with short restenosis at LCX ostium. D) Three-dimensional OCT assessment showing neointima growth over the stent struts splitting the LCX ostium in three different, small orifices. E) Fractional flow reserve assessment documenting the haemodynamic significance of the multi-hole restenosis. (Case presented at EBC 2019 by Dr Rony Mathew Kadavil).
HOW AND WHY TO PERFORM KISSING
Over the years, it has clearly emerged that the efficacy of strut clearance from the SB by kissing balloon inflation is dependent on the location of the wire re-cross and that kissing balloon inflation may induce a major oval distortion in the proximal MV. Thus, POT, distal SB rewiring followed by kissing balloon inflation (eventually conducted with short non-compliant balloons) and repeat POT are recommended21 in order to minimise proximal MV distortion and to restore an ideal bifurcation anatomy (Figure 5). To date, clinical data do not support the use of routine kissing balloon inflation26. However, the results of a recent multicentre registry on CBL, treated by ultra-thin stents, suggested that kissing inflation performed with short balloon overlap may reduce target lesion revascularisations27.
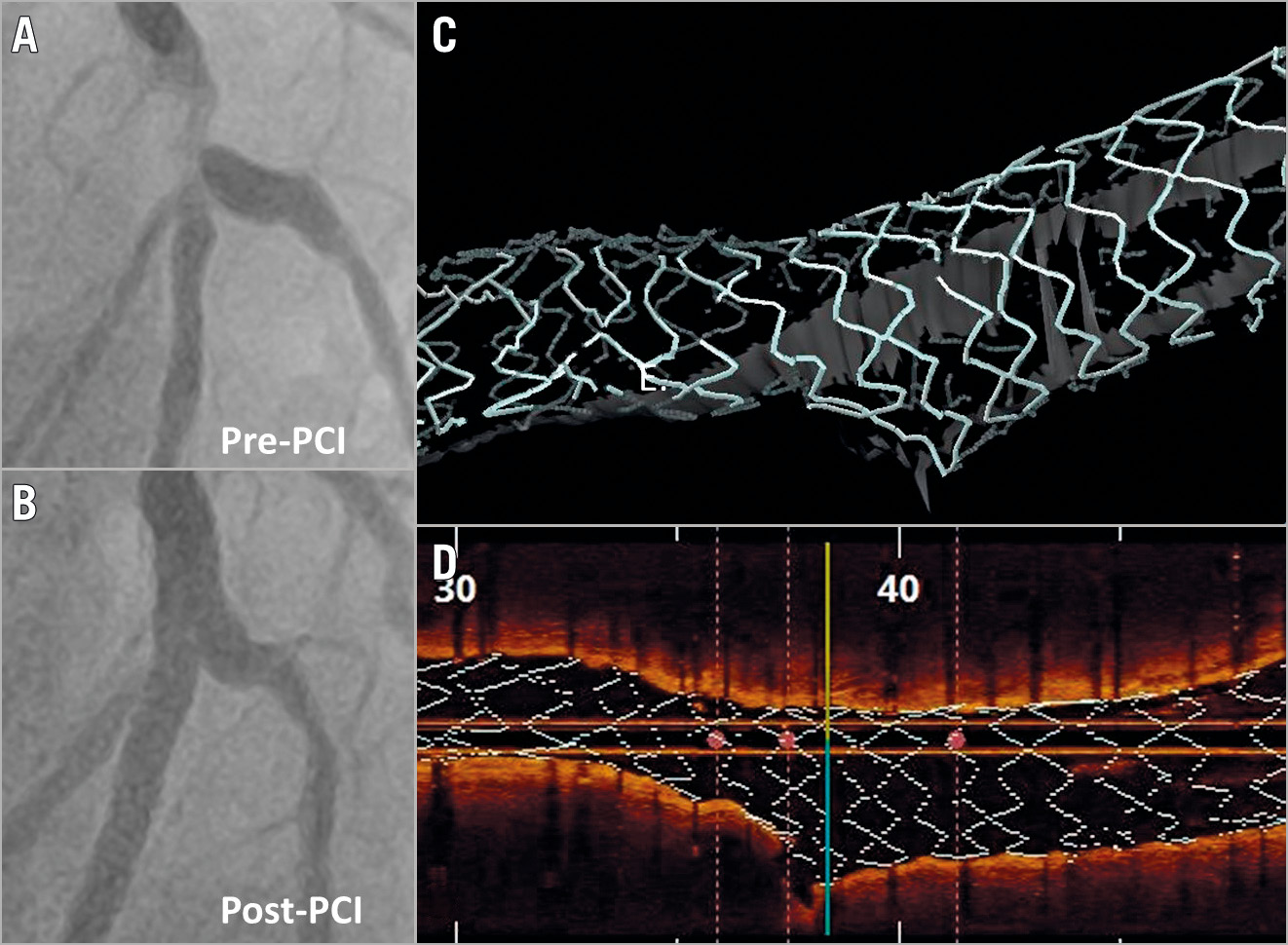
Figure 5. Efficacy of provisional technique in modifying the stent platform allowing the achievement of a good result in a patient with a complex bifurcation lesion. A) Pre-PCI angiography. B) Result after LAD stent implantation followed by POT, distal rewiring, kissing balloon inflation with short balloon overlap and re-POT. C) & D) Three-dimensional OCT reconstructions of the final result achieved.
WHAT ABOUT THE POT-SIDE-POT STRATEGY?
The sequential application of single balloon dilation in the proximal MV, SB and proximal MV (POT-side-POT) is appealing due to its simplicity and efficacy in bench tests. Of note, recent data documented that this technique is probably less simple than theorised. In particular, SB ballooning induces a distortion in the MV stent deserving appropriate correction and it is able to clear SB stent struts only when performed after distal rewiring (similar to kissing). Furthermore, the position of the final (re-)POT balloon (a factor that can be challenging to control in clinical practice) impacts significantly on final SB obstruction28.
NOVELTIES IN AN ELECTIVE TWO-STENT STRATEGY
CBL with extensive atherosclerosis involving a large and significantly diseased SB may benefit from an elective two-stent bifurcation technique. Different technical options are available and should be selected according to the specific lesion anatomy and the operator’s experience. T, T and small protrusion (TAP), culotte and double-kissing (DK) crush represent the most popular two-stent techniques. Their recommended steps have been summarised previously21. In all two-stent techniques, repeated POT manoeuvres21 before any branch rewiring are pivotal since malapposed stent struts in the proximal MV or around the carina may easily be displaced during device (balloon/stent) advancement, causing metallic strut accumulation. Observational data on patients treated by two-stent techniques are continuing to report better clinical outcomes with final kissing balloon inflation27, so that its performance can be regarded as a measure of procedural success.
The culotte technique represents a very “flexible” technique, offering the opportunity for liberal selection of the first treated branch between the distal MV and SB. Among possible technical improvements, the minimisation of stent overlap in the MV and the addition of a further kissing balloon inflation after first stent implantation are notable. These modifications add technical complexity during the practice, but the resulting “DK-mini-culotte” has the potential for outstanding stent configuration29.
Regarding the DK-crush technique, a further increase in its popularity is expected after the outstanding results recently reported in the DK-CRUSH V trial30 and the DEFINITION II trial18. However, the complexity of the technique continues to pose specific challenges, and high-volume DK-crush operators continue to develop technical refinements with the potential addition of further steps. Among these, the immediate high-pressure post-dilation of the SB stent (“proximal SB optimisation”) proposed by Lavarra31 has been recognised by the EBC as useful21. Other operators are suggesting that the selection of ultra-thin strut biodegradable polymer-coated stents may minimise stent overlap thickness and enhance healing after stent crushing32.
DRUG-ELUTING BALLOON FOR BIFURCATION: WHERE ARE WE?
Drug-eluting balloon (DEB) technology incorporates devices with known heterogeneity (no class effect) and potential interest in the setting of bifurcation PCI.
In de novo CBL, DEB use in the SB is an attractive approach. The PEPCAD BIF trial showed that SB lesions without both major dissections and significant early vessel recoil have a very acceptable late lumen loss33. A meta-analysis including 349 patients compared the SB result using standard balloon versus DEB angioplasty34. At nine months, DEB use was associated with lower SB late lumen loss compared with balloon angioplasty; however, SB binary restenosis was not reduced significantly. Overall, the data are inconclusive, with many unanswered questions including the appropriate SB selection, technique (DEB with or without final kissing ballooning or repeat POT) and actual impact on meaningful clinical endpoints.
DEB usage in restenosis has been more extensively tested and clearly provides an advantage of minimising multiple stent layers in patients presenting with CBL restenosis, especially where the index PCI involved two-stent techniques35.
CERTAINTIES AND EMERGING DOUBTS ON UNPROTECTED LM PCI EFFICACY
Within the last year, long-term clinical follow-up results have been published from important landmark studies comparing PCI and coronary artery bypass grafting (CABG) for patients with unprotected LM disease.
In the extended 10-year follow-up of mortality within the SYNTAX trial36, all-cause death was not significantly different between PCI and CABG. Of note, CABG provided a significant survival benefit in patients with three-vessel disease, but not in those with LM disease.
The recently published five-year results from the EXCEL and NOBLE trials37,38 have generated vigorous debate regarding contemporary PCI versus CABG in the treatment of LM disease. Repeat revascularisation was higher in the PCI arm in both trials. Total mortality differed significantly in EXCEL but not in the NOBLE trial.
A very recent meta-analysis39 of five randomised trials (including NOBLE and EXCEL) on a total of 4,612 unprotected LM patients with a weighted mean follow-up duration of 67 months allowed derivation of the data summarised in Supplementary Table 2.
These novel data reinforce the need for tailored patient selection and PCI improvements. The role of a multidisciplinary Heart Team in the treatment decision for stable or stabilised patients with unprotected LM disease is emphasised. The key issues (anatomical assessment, team organisation) that might be critical for successful LM PCI programmes were extensively reviewed in the previous EBC consensus documents2,3.
DUAL ANTIPLATELET THERAPY IN BIFURCATION LESION PCI PATIENTS
The ESC guidelines highlight coronary bifurcation as a risk factor for coronary ischaemic events, suggesting that a longer duration (≥12 months) of dual antiplatelet therapy (DAPT) may be considered40. This recommendation is based mainly on a meta-analysis41 comprising 9,577 patients, showing that two-stent bifurcation stenting was the strongest risk factor for adverse events.
In the recent EBC registry41 including 5,036 patients undergoing bifurcation PCI, the risk of adverse events was significantly increased among patients who discontinued DAPT prematurely (<6 months in stable CAD, <12 months in ACS). Also, as compared with one-stent techniques, two-stent techniques were associated with significantly increased major adverse events.
Given the trade-off between ischaemic and bleeding risks for any DAPT duration, a careful patient risk stratification seems of utmost relevance. An EBC-promoted study group has recently revised available DAPT selection options42.
Conclusions
Devices, techniques and imaging modalities are evolving at an incredible pace and their use in bifurcated lesions and unprotected left main needs to be updated. Bifurcation stenting techniques, intracoronary imaging, bifurcation simulation, drug-eluting balloon technology and tailored antiplatelet therapy are identified as pivotal to enhance clinical outcomes.
Conflict of interest statement
F. Burzotta has received speaker fees from Medtronic, Abiomed, and Abbott. J.F. Lassen has received speaker fees from Medtronic, Boston Scientific, Biotronik, Abbott and Biosensors. A.P. Banning has received institutional funding of a fellowship from Boston Scientific and speaker fees from Boston, Abbott, Medtronic, Philips/Volcano and Miracor. T.W. Johnson has received speaker fees from Abbott, Boston Scientific, Medtronic, and Terumo, and institutional funding for fellowships from Boston Scientific and Terumo. D. Hildick-Smith has received advisory board/consultancy/research funding from Terumo, Medtronic, Abbott, and Boston Scientific. R. Albiero has received speaker fees from Medtronic and Abbott. M. Pan has received speaker fees from Abbott, Terumo and Volcano. A. Chieffo has received speaker fees from Abiomed and GADA. O. Darremont has received speaker fees from Edwards. Y.S. Chatzizisis has received speaker fees, consultation fees and research grant from Boston Scientific, and research support from Medtronic. T. Lefèvre has received speaker fees from Abbott, Medtronic and Terumo. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.