Abstract
The European Bifurcation Club (EBC) was initiated in 2004 to support a continuous overview of the field of coronary artery bifurcation interventions and aims to facilitate a scientific discussion and an exchange of ideas on the management of bifurcation disease. The EBC hosts an annual, two-day compact meeting, dedicated to bifurcations, which brings together physicians, pathologists, engineers, biologists, physicists, mathematicians, epidemiologists and statisticians for detailed discussions. Every meeting is finalised with a consensus statement that reflects the unique opportunity of combining the opinion of interventional cardiologists with the opinion of a large variety of other scientists on bifurcation management. A series of consensus sessions dedicated to specific topics, to strengthen the consensus debates and focus the discussions, was introduced at this year’s meeting. The sessions comprise an intensive overview of the present literature, a pro and con debate and a voting system, to guide the consensus-building process. The present document represents the summary of the up-to-date EBC consensus and recommendations from the 12th annual EBC meeting in 2016 in Rotterdam.
Introduction
“You never know what is enough unless you know what is more than enough”.
William Blake (1757-1827)
BACKGROUND
The EBC has held 12 annual meetings since 2004, published eight general consensus statements1-8, and a number of consensus documents dedicated to specific topics4,9,10, and has edited two EuroIntervention supplements on bifurcation treatment11,12.
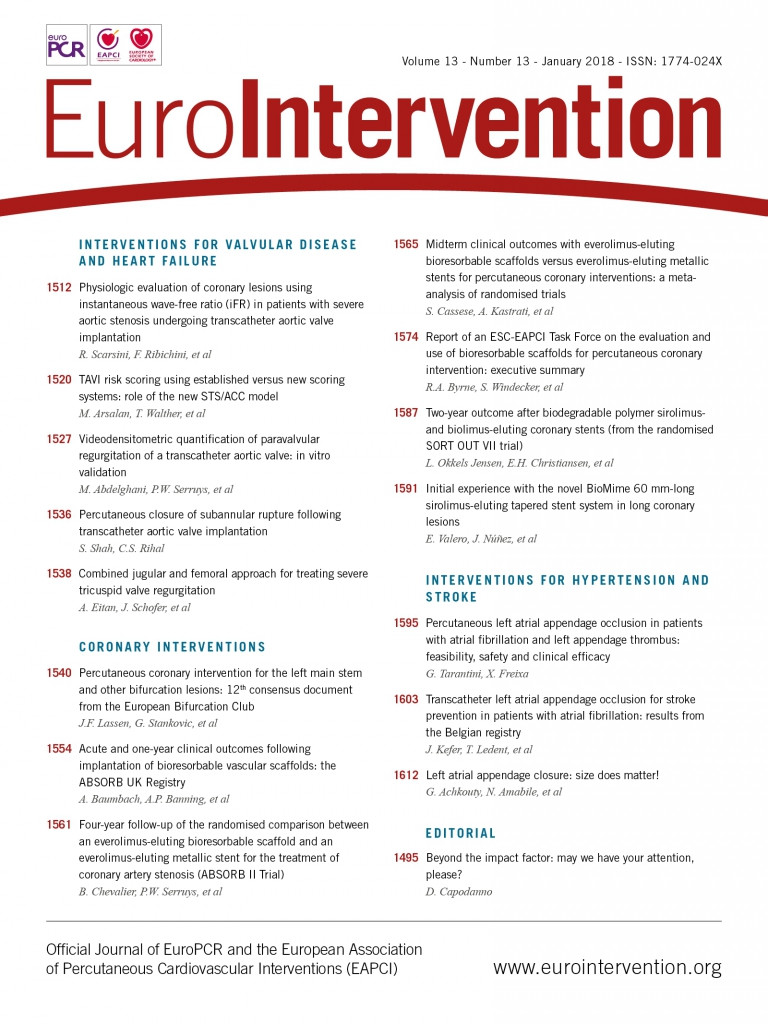
A simple description of bifurcation lesions, stenosis quantification, vessel calcification and PCI techniques is not straightforward. The first consensus document reflects how consensus was achieved by discussion of the definitions of a bifurcation and of a significant side branch (SB)1. Over the years which followed, EBC consensus was reached by promoting a simplified yet universal classification of bifurcation lesions, the Medina classification13, and an accurate definition of each of the various techniques used in bifurcation stenting combined with a precise classification system to facilitate the description, the MADS classification4. The two classifications have provided a valuable opportunity to standardise reports, to allow comparisons between studies and to facilitate interpretation of published results in the evolving literature within the field. For all of these reasons, systematic use of these classifications is still strongly recommended by the EBC7,8. It became evident that the understanding of the coronary bifurcation anatomy and physiology, as well as that of the interaction between interventional devices (stents, balloons) and bifurcated vessels, was crucial in order to comprehend the technical issues and long-term results of bifurcation intervention. A series of EBC-promoted studies helped to characterise the geometric relations linking the main branch (MB) and SB. Several mathematical models (Murray’s, Finet’s, Huo-Kassab’s and “area-preservation”) have been reported14-16 (Figure 1). They confirm that coronary bifurcation anatomy may basically be regarded as a complex vessel/function structure where three different vessel segments (proximal MB, distal MB and SB) are interpolated through the bifurcation core segment where the distinction between MB and SB is merely virtual8. The fractal nature of the coronary tree was also described, pointing to the fact that a coronary MB tapers after the take-off of an SB8 (Figure 2). This understanding led to development of the proximal optimisation technique (POT)17, that changed the tubular stent to a tapered device fitting both distal and proximal diameters of the MB and opened stent struts towards the SB respecting the anatomy of the bifurcation core segment8. Over the years, technical and anatomical discussion became more and more complex. The theoretical considerations were further tested by bench testing, intravascular imaging, and flow evaluations by mathematic model building, pushing the overall understanding of coronary bifurcation disease forward11. These achievements and the evolution of ideas in the EBC have formed the foundation for this year’s consensus discussion and have led the 12th EBC meeting to the refined recommendations in the present document.
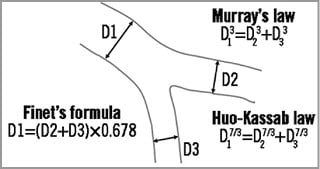
Figure 1. The fractal and tapering nature of coronary vessels. Different main structure-function scaling laws of the coronary vascular tree.
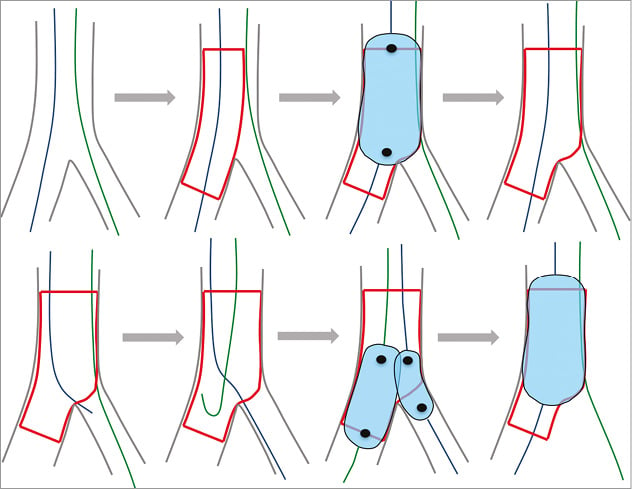
Figure 2. Summary of the provisional approach. Upper panel from left to right: two wires in place, main branch stent sized according to the distal reference, POT, keep it open. Lower panel: access towards the distal strut, guidewire exchange, kissing balloon inflation with short non-compliant balloons (not proximal to the polygon of confluence to avoid dilating the distal part of the stent too much towards the side branch). A final POT should be carried out if the two balloons are proximal to the polygon of confluence.
THE EBC UPDATE ON PROVISIONAL BIFURCATION STENTING STRATEGY
The provisional side branch (SB) stenting strategy is currently considered the “standard” approach for treatment of the vast majority of bifurcation lesions8,18,19. Provisional SB stenting is a treatment philosophy rather than a technique. Indeed, once the MB has been identified, it is stented first4 after wiring both branches of the bifurcation. The SB may (or may not) be treated after optimisation of MB treatment using the POT (Figure 2). If the SB needs attention, guidewires are exchanged and kissing balloon inflation or POT/side/POT (re-POT) is performed20-24 (Figure 3). In the presence of significant SB flow limitation or poor angiographic results in an SB supplying a significant myocardial territory25, subsequent SB stenting can be performed (T, T and protrusion [TAP] or culotte), with systematic final kissing balloon inflation (KBI) and a finalising POT (Figure 4). The long-term clinical outcomes are determined by the status of the MB after bifurcation stenting. Ensuring optimal results in the MB should be given priority over optimising the appearance in the SB if there is a need for a choice between the two.
Figure 3. The philosophy of the provisional bifurcation stenting approach. From left to right: main branch stenting with stent implantation that respects the distal main branch diameter, finalised with POT to respect the original tapering anatomy and to open the struts towards the side branch. If the side branch is compromised, continue to dilatation of the side branch. If still compromised, an escalation to side branch stenting is facilitated. Always finalise a procedure with POT.
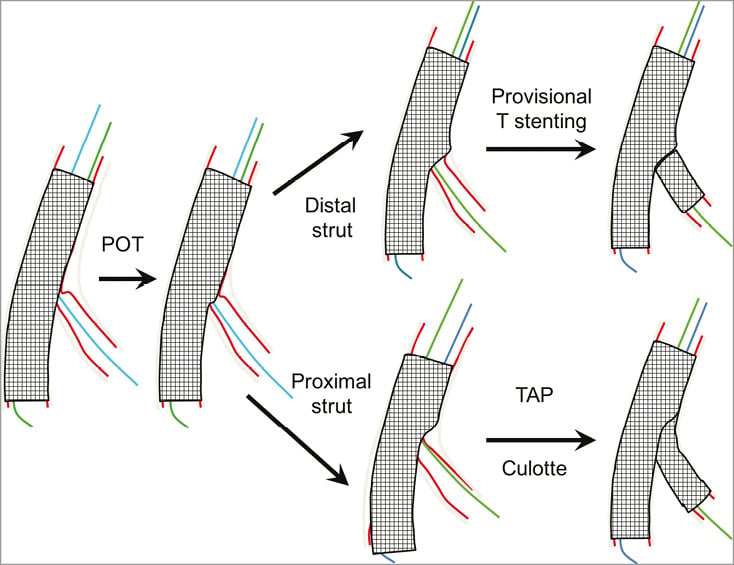
Figure 4. Different options in stepwise escalation to side branch stenting in the provisional stenting approach.
The provisional SB stenting strategy (MB stenting first, followed by POT, and only finalised with SB stenting if needed – provisional SB stenting) is recommended for most bifurcation lesions.
INITIAL APPROACH
Almost all bifurcation lesions –including the distal left main coronary artery (LMCA)– can be safely treated via the radial artery approach with a large lumen 6 Fr guiding catheter. A 7 Fr guiding catheter may be required if the planned strategy involves complex double stenting techniques or three balloons for trifurcations. In very large vessels, 7 Fr guides are also helpful when a kissing inflation using balloons larger than 3.5 mm in diameter is needed.
OPTIMAL ANGIOGRAPHIC VIEW
Given the tri-dimensional structure of bifurcations, it is impossible to avoid a foreshortening effect when trying to obtain a plane image of the three bifurcation segments. Consequently, it is necessary to record several views from various angles to obtain a comprehensive picture of the lesion characteristics, in order to carry out the technical procedure appropriately and assess the procedural outcome. The SB take-off is the crucial point, which is rarely visualised adequately from two orthogonal views and may be explored from a single angle called “the working view”. This view allows the visualisation of branch division as well as the measurement of angles and assessment of the degree of ostial SB stenosis. This is generally an RAO or LAO view with caudal inclination for the left main (LM) coronary artery, an anterior-posterior projection with marked cranial angulation for left anterior descending coronary artery (LAD)-diagonal bifurcations, a slight RAO or LAO projection with caudal angulation for circumflex-proximal marginal bifurcations or cranial angulation for dominant distal circumflex (Cx) coronary arteries, and an anteroposterior projection with cranial angulation for distal right coronary arteries. An optimal view of the Cx ostium, however, is not fully obtainable in up to 40% of cases due to the constraints of the C-arm, which cannot reach sufficient caudal projection. Intravascular imaging can provide additional important information in these situations26.
– Multiple angiographic views are required for full assessment of a bifurcation.
– Optimal views include projections perpendicular to the SB ostium.
– An optimal view of the Cx ostium is not fully achievable in 40% of cases.
THE JAILING WIRE TECHNIQUE
The jailing wire technique consists of leaving a wire in the SB while implanting a stent in the MB. This manoeuvre has been recommended in previous EBC consensus documents2,7,8 due to the following potential advantages: 1) the technique helps to keep the SB open and, in case of occlusion, the guidewire is the only marker of the SB position; 2) it facilitates the access to the SB by favourably changing the angle of the bifurcation; 3) the jailed wire is a modality of anchoring that facilitates the intubation of the guiding catheter, providing a firmer support for the balloon to cross the origin of the SB; and 4) in extreme situations, it can be used as a rescue procedure, to pass a low-profile balloon and dilate the SB (Figure 5)27-29. The jailed wire technique is not free from complications. The trapped wire may suffer a fracture during the removal manoeuvre. The calcification of the vessel wall, the length of the trapped wire, and high pressures used at the MB stent deployment have been suggested as predictors of jailed wire rupture. In a recent study30, polymer-coated wires seemed to be more resistant to retrieval damage than non-polymer-coated wires. There is concern regarding embolisation of hydrophilic coating in patients with PCI. This complication has been described in histological samples after using polymer-coated wires31. Despite this, polymer-coated wires are widely used around the world and myocardial damage in terms of post-procedure troponin elevation has been similar among patients in whom polymer-coated or non-polymer-coated wires were used30. Microcatheters, especially those with dual lumen, as well as the Venture™ catheter (Vascular Solutions, Minneapolis, MN, USA) with its deflectable tip, can prove useful in wiring the SB in difficult cases. Plaque modification, with balloon dilatation, cutting balloon or rotablation of the MB, may facilitate SB wiring when access is difficult. The shape of the guidewire tip should be prepared manually in accordance with the angle, the MB diameter and the anatomical take-off of the SB. It is recommended that the most difficult lesion should be wired first in order to avoid wire wrap. It is also very important to shape the distal tip of the MB guidewire in order subsequently to recross the distal strut of the MB stent. Pushing the MB wire too distally should be avoided not only because of the risk of distal dissection or perforation, but also to maintain the shape of the wire tip which will serve to wire the SB through the MB stent by means of a gentle pullback technique from the distal MB to the SB.
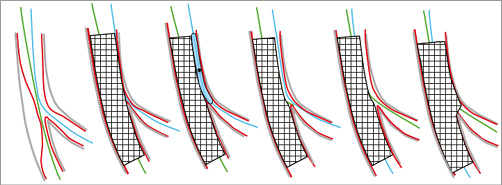
Figure 5. Side branch salvage using the jailed wire technique.
– Always wire both the MB and SB if it is important to maintain the SB patent.
– Jailing the SB wire is safe, maintains SB access, and facilitates SB rewiring.
– Microcatheters can facilitate difficult SB access.
– Rewiring of the SB by the pullback technique is encouraged.
PREDILATATION
MB preparation is a crucial step and should be considered routine practice in stable patients. It facilitates MB sizing and post-stenting treatment of the proximal MB segment, which may influence the long-term results of bifurcation stenting. Predilatation of the SB remains a subject of controversy. It is generally preferable not to predilate the SB ostium given that the occurrence of dissection inherent in the enlargement of the lumen of the SB ostium could increase the likelihood of unintended access to the SB through a proximal strut. This is based on the fact that plaque is most often distributed opposite the flow divider in the SB ostium, thus increasing the chance that the stent cell covering the small opening is actually a distal cell11,12. Access through a distal strut is the only possibility for projecting struts in the SB in order to treat both the MB and the SB ostium with only one stent. Song et al20 assessed the effect of SB predilatation on outcomes for true bifurcation lesions using a provisional approach. After propensity score-matched population analysis, they observed that SB predilatation could be associated with an increased risk of repeat revascularisation. However, Pan et al32 reported that, after randomisation to either SB predilatation or no SB predilatation, the rate of SB rewiring failure, the time of rewiring, the number of wires used, and the incidence of major events were similar in both groups of patients. The only difference was a higher TIMI flow rate in the SB after MB stenting in the SB predilatation group, but final SB TIMI flow and clinical outcomes were similar in both groups at the end of the procedure. We recommend that SB predilatation should be performed when SB access is difficult or in cases of severe diffuse and/or calcified SB lesion or compromised SB flow after wiring.
When carrying out SB predilatation, it is very important to assess the angiographic result carefully before MB stenting and to be ready to switch to another strategy (reverse provisional stenting strategy or DK-crush) in cases of dissection or difficult SB access.
– Predilatation of the MB is recommended.
– Predilatation of the SB is only recommended when access is difficult, in cases of severe diffuse and/or calcified SB lesion or compromised SB flow after wiring.
– Consider a stenting strategy (reverse provisional or two-stent up front) allowing stenting of the SB first in case of dissection or difficult SB access.
MAIN BRANCH STENTING
Second-generation drug-eluting stents (DES) are recommended for bifurcation treatment. Selection of the most appropriate stent platform is essential and should be made according to the maximal expansion ability of the stent, in order to allow stent apposition both on the MB wall and on the SB ostium22,33-36. The maximal opening diameter of the MB stent at the SB ostium is also an important criterion for the most proximal bifurcations such as the LM. The choice of stent diameter for MB stenting is crucial37-41: when too large (stent diameter selected according to the proximal MB reference diameter), it may significantly increase the risk of SB occlusion caused by carina shifting, or create a dissection in the distal segment. Stent diameter should be selected according to the reference diameter of the MB distal segment in accordance with the fractal law, the potential drawback being inadequate apposition of the stent on the proximal MB segment. However, this can be easily corrected by POT and/or KBI.
– Second-generation DES should be the first choice in bifurcation treatment.
– Select nominal stent diameter of the MB according to the reference size distal to the SB take-off.
PROXIMAL OPTIMISATION TECHNIQUE
Workhorse stents can be adapted to the fractal anatomy of bifurcation lesions, simply by using POT, especially in bifurcation lesions with a large SB where there is a greater difference between the proximal and distal MB diameters42.
POT is carried out after MB stenting by inflating a short balloon just proximal to the carina24. This parameter needs to be taken into account before choosing the MB stent length, in order to leave at least 6 to 10 mm of stent length proximal to the carina (the smallest length of commonly available balloons). Careful positioning of the balloon for POT is crucial and may influence the final result: if too distal, it increases the risk of SB occlusion; if too proximal, it has no effect on the stent strut towards the SB. Ideally, the distal shoulder of the balloon should be positioned just proximal to the carina while the proximal part is still in the stent in order to avoid geographical miss. The main problem is that the positioning of the distal marker compared to the distal shoulder varies among the different balloons currently available (Figure 6); this should be clearly specified by the manufacturers. If the balloon does not span the entire stented proximal MB stent segment, the balloon should be repositioned and re-inflated to ensure that the most proximal part of the stent is also sufficiently expanded. The diameter ratio between the balloon and the proximal MB reference segment should be 1/1. Thus, compliant or non-compliant balloons can be used, depending on the diameter the operator wants to achieve. Inflation is performed at nominal pressure or higher in order to reach the appropriate diameter. As a result, the original anatomical configuration of the bifurcation is restored in compliance with the branching law.
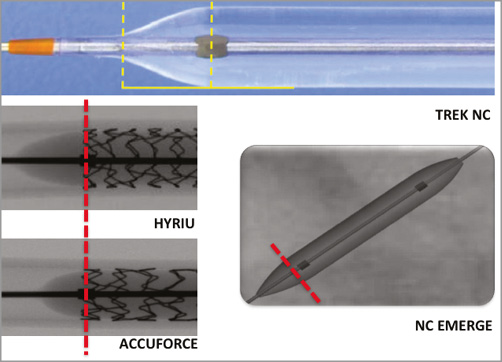
Figure 6. Balloon positioning for optimal POT may be different according to balloon shape.
Computer simulations and in vivo application have shown the other advantages of using POT in bifurcation lesion treatment11,12. First, by apposing the stent strut to the proximal MB wall, POT prevents the guidewire from recrossing into the SB between the arterial wall and the stent. Second, POT induces a constant increase in cell size area and modifies the orientation of the SB ostium. This phenomenon facilitates access towards the SB, and may also facilitate the distal recrossing (close to the carina) by reducing the possibility of recrossing through the MB stent. Consequently, POT is particularly helpful in instances of crossing failure with the wire. This also facilitates the recrossing of the balloon and sometimes the stent by reducing the friction towards the enlarged strut. The clinical relevance of POT is very difficult to assess, but recently, during the last EBC meeting, H.C. Gwon communicated the preliminary data of the COBIS II registry, analysing a subgroup of a propensity score-matched population with a large SB (≥2.5 mm), comparing 665 patients without POT and 204 patients with POT. There was a significant difference in terms of a combined endpoint (MACCE) at 36-month follow-up in favour of the POT group. POT should therefore become a systematic part of the standard approach to bifurcation lesion treatment.
– POT is recommended in bifurcation stenting.
– POT should be performed before SB rewiring to facilitate access and reduce the risk of accidental abluminal rewiring.
– Ensure dilatation from just proximal to the carina to the proximal stent edge.
SB TREATMENT
The fundamental advantage of the provisional SB stenting approach is that SB treatment remains an open option throughout the procedure. When the SB is small, a “keep it open strategy” (Figure 3) is probably the best approach, starting by wiring both branches and stenting the MB. The same strategy can be applied when the SB needs attention regardless of the possibility that the operator may decide not to open the struts towards the SB, based on the POT results. If the operator considers that the MB stent struts should be opened, then the MB wire (or a third wire) can be used to enter the SB through the most distal strut and perform subsequent SB ostium dilatation followed by KBI and a final POT. If SB stenting is necessary, it should be followed by KBI, and the procedure should be finalised with a second POT.
– SB treatment is indicated if the ostium is pinched or the flow is limited after POT.
– If SB treatment is required, rewire and dilate the SB and finalise with KBI and POT.
– SB stenting is indicated if the SB is occluded, dissected, or has limited flow despite KBI.
SIDE BRANCH OPENING
Opening the distal strut (close to the carina) of the MB stent towards the SB improves SB ostium scaffolding and decreases the need for SB stenting. In order to increase the odds of crossing the distal strut, the recommended technique is to have a perpendicular view of the SB ostium and to enter the SB by pulling back the MB wire (or a third wire in the direction of the SB ostium). If there is any doubt, the jailed SB wire can be removed, and a second attempt can be made using this wire or another wire to enter the SB as close as possible to the carina. The wire position can be verified by optical coherence tomography (OCT). Reports have shown that using a non-compliant (NC) balloon is associated with a lower risk of SB dissection and better clinical outcomes43,44. After opening the SB ostium, it is strongly recommended that final POT or KBI should be performed, preferably with two short NC balloons sized according to the actual reference size of the vessels or 0.5 mm below. In order to avoid proximal MB stent distortion, it is recommended that the balloons should not be positioned proximal to the bifurcation core segment (Figure 1).
– Rewiring of the SB should aim to recross a distal stent cell.
– KBI should be performed using two NC balloons.
– The procedure should be finalised by POT after kissing to correct the proximal MB stent distortion.
WHEN TWO STENTS ARE CONSIDERED
In 5 to 25% of cases, a second stent may be needed depending on the lesion characteristics, SB importance, access towards the most distal strut and level of residual SB stenosis tolerated by the operator19,45,46. When the SB ostium appearance is optimal but the SB lesion is longer than 5 mm, a second stent can be used in a T-shape configuration without protrusion into the MB and a KBI should be performed (Figure 4). When the SB ostium appearance is not clearly visible or not optimal (usually access through a proximal strut) and the SB lesion is longer than 5 mm, T-stenting with minor protrusion in the MB can be performed (TAP) or the culotte technique according to operator preference47. Final KBI followed by POT should be systematically carried out at the end of the procedure when two stents have been implanted.
– Bail-out SB stenting after MB stenting is performed with T-stenting, TAP or culotte.
– Implantation technique is selected according to angulations, reference size differences and operator capabilities.
– Always perform final KBI followed by POT in two-stent techniques.
EBC RECOMMENDATIONS ON UPFRONT USE OF TWO-STENT TECHNIQUES
There are basically two situations in which the operator has to select a two-stent bifurcation technique: 1) the bail-out treatment of an SB during the provisional stenting strategy, and 2) the elective treatment of bifurcated lesions with complex anatomy and diffuse atherosclerotic involvement of both the MB and the SB. These two settings are not identical; each mandates specific considerations. The technique in the first situation is covered above.
ELECTIVE TWO-STENT TREATMENT
Upfront use of two stents may basically only be needed in very complex lesions with large calcified side branches with ostial disease extending >5 mm from the carina and in bifurcations with side branches whose access is particularly challenging and where the SB should be secured by stenting once accessed. Accordingly, two technical issues are critical for the clinical outcome of patients where elective double stenting is needed: 1) lesion preparation before bifurcation stenting, and 2) kissing balloon inflation followed by POT afterwards. Complete stent expansion will facilitate optimal scaffolding of atherosclerotic lesions in order to achieve the best acute vessel lumen gain. Similarly, malapposed or underexpanded stent struts may affect prognosis by triggering both restenosis and stent thrombosis. Accordingly, extensive post-dilatation is needed.
In selection of a specific two-stent technique, operators have a wide range of theoretical options well summarised by the MADS classification4. Only some of the techniques have been tested in trials. Some of the techniques have been refined with the aim of overcoming the problems that emerged during clinical practice. Both elective T-stenting and simultaneous kissing stenting (SKS technique) have important limitations that include the lack of predictable results in terms of stent distortion and vessel wall coverage with elective T, and major concerns regarding safety with the long, double-layer neocarina by SKS47-50.
The crush technique reported by Colombo et al51 has gained popularity since it has the benefit of allowing stenting both the MB and SB without rewiring through the stent struts. However, due to the low success rate in finalising the procedures with KBI and suboptimal long-term outcome in the absence of KBI, this procedure is not recommended anymore. Chen and colleagues modified the original crush technique as the DK-crush technique52. This modification made the procedure more complex (since it requires the systematic performance of two kissing balloon inflations), but has been shown to reduce dramatically the risk of failures in performing kissing balloon inflation and to be clinically effective and safe in the long term in trials conducted by operators dedicated to the technique50. Culotte stenting has a widespread use and has been tested in several trials. One limitation of the technique is the need for the two stents to accommodate the potential diameter mismatch between SB and proximal MB53,54 (Figure 4). Finally, it should be emphasised that successful elective double stenting may be achieved using an “inverted” provisional approach55 by simply stenting the side branch first, placing the stent from the proximal MB to the SB, jailing the distal main branch. Use POT in the proximal MB followed by distal MB rewiring and dilation and implanting the second stent, only if needed.
– A planned two-stent technique may be indicated for bifurcations with long SB lesions, difficult SB access or high risk of SB compromise.
– Vessel anatomy, vessel sizes, a need for stenting the SB first and operator proficiency affect the choice of strategy.
– Recommended techniques include reverse provisional stenting, T-stenting, culotte and DK-crush.
– POT is recommended and ensures optimal stent expansion in both the MB and SB.
– Always finalise a double stent procedure with KBI, followed by POT.
ROLE OF FRACTIONAL FLOW RESERVE (FFR) IN BIFURCATIONS
The use of a pressure wire to measure iFR/FFR has become a standard part of interventional practice. In patients with stable angina when no other objective evidence of ischaemia is available, a pressure wire can be used in either the MB and/or SB to determine whether PCI is indicated. However, use of a pressure wire to determine whether a single-stent or two-stent approach is required is not recommended. When using the provisional bifurcation approach, a pressure wire has been used after MB stent implantation, when there is good MB and SB flow but focal ostial “pinching” of the SB on the angiogram. Under these circumstances, this approach can be used for additional reassurance that a second stent to the SB is unnecessary. The evaluation is, however, difficult since the pinching could be temporary, due to vascular wall oedema, minor intramural haematomas and plaque shift, prone to remodelling. Accordingly, management of an abnormal FFR in the SB after MB stenting is more complex and controversial, but ostial SB balloon dilation and careful POT are usually the initial approaches.
– An SB FFR value above 0.80 before MB stenting does not exclude a subsequent need for treating the SB.
– An FFR value above 0.80 in a jailed SB indicates that further SB treatment may be safely deferred.
INTRACORONARY IMAGING
Angiographic ambiguity is frequent during bifurcation stenting26. Adjunctive intravascular imaging with intravascular ultrasound (IVUS) or OCT may provide crucial information in planning and optimising treatment. Angiographic evaluation is often limited in assessment of the SB ostium, overlapping stent segments, lesion coverage, wire positions, stent expansion and strut apposition. IVUS and OCT both enable lesion assessment, evaluation of predilatation, reference sizing and evaluation of adequate vessel and stent expansion after stenting56-60. Compared to IVUS, OCT provides superior images of the lumen surface, calcified plaques, predilatation results, stent positions, wire positions and the SB ostium from both MB and SB pullbacks. However, OCT may increase the use of contrast and limit aorto-ostial assessment in some cases. IVUS allows better characterisation of plaque burden and does not require vessel flushing during acquisition. Advancing an imaging catheter into a jailed SB is not recommended, as distortion or fracture of the stent can occur or the wire could be trapped61. The main focus points for guiding bifurcation stenting using intravascular imaging are the following. Before stent implantation, consider: 1) risk of SB compromise (lesions proximal or distal to the SB and ostial stenosis have been shown to affect this risk of SB compromise after MB stenting62,63), 2) planning of stent length to limit residual stenosis and fibroatheroma in adjoining segments64, 3) assessment of segmental stent diameters based on proximal and distal reference size estimations, 4) planning the size and length of the balloon for POT to ensure it fits within the stent from carina to the proximal stent edge. After stent implantation, post-dilatation, POT and rewiring, a scan may be performed to: 1) rule out a higher degree of residual edge stenosis, 2) evaluate stent expansion and apposition, 3) verify wire position in SB recrossing65-67, 4) rule out accidental abluminal rewiring68, and 5) perform a final scan after KBI to evaluate the SB ostium. If an SB stent is implanted, it is recommended to scan the stented SB and evaluate stent expansion and apposition. In two-stent techniques, evaluation after each rewiring may be indicated. Use of OCT after bifurcation stenting can, due to the high resolution, reveal imperfections which are often not noticed by angiography alone. The clinical significance of these findings has not yet been established; some may resolve spontaneously while others may be related to impaired outcome69.
– Intravascular imaging is a valuable supplement in bifurcation treatment and is especially useful in complex lesions due to the limitations of angiography alone.
– IVUS is recommended for LMCA bifurcation treatment but OCT may provide more detailed information and can be used with the provision that aorto-ostial evaluation is often not possible.
– OCT may be superior and may be more easy to interpret compared to IVUS in the evaluation of the SB ostium, stent positions, malapposition, wire positions, and in the detection of thrombus.
– Wire positions in stent recrossing can be evaluated by OCT as the position affects scaffolding of the ostium and the formation of a metallic carina.
– Accidental abluminal rewiring of stents and accidental stent crush can be ruled out by OCT.
– Scanning of both MB and SB are recommended when guiding two-stent treatment by intravascular imaging.
QUANTITATIVE CORONARY ANALYSIS (QCA) – DEDICATED QCA SYSTEMS FOR BIFURCATIONS
QCA is an important standard analysis in scientific reporting and for regulatory assessment. Analysis of bifurcations by 2D QCA requires dedicated bifurcation software9,10,70-73. Use of 3D bifurcation QCA improves the accuracy of quantitative measurements including bifurcation angulations26,74-76. Present 3D QCA systems further provide the optimal projection angle in bifurcations26 and, in some systems, form the backbone for co-registration to OCT and IVUS77,78 and for virtual FFR computation without the use of a pressure wire, including the quantitative flow ratio (QFR) technology78-80.
– QCA software dedicated to bifurcations is recommended.
– 3D QCA improves quantitative measurements compared to 2D QCA.
– QCA may aid stent sizing during intervention but its clinical value remains unknown.
THE LEFT MAIN
PCI OR CABG FOR DISTAL LEFT MAIN BIFURCATION LESIONS
Guidelines on myocardial revascularisation from the European Society of Cardiology/European Association for Cardio-Thoracic Surgery, give a class 1B indication for PCI in patients with a low SYNTAX score and significant LM disease. The level of evidence for PCI for LM disease in patients with a SYNTAX score of 22-33 is class IIa. For a SYNTAX score ≥33, the recommendation is class III81. The recent EXCEL82 and NOBLE trials83,84 (PCI versus coronary artery bypass grafting [CABG] in LM) have strengthened the level of evidence for use of PCI with latest-generation DES in the treatment of LM disease. Notably, CABG had no prognostic advantage compared to PCI in terms of mortality or stroke in either trial and, accordingly, an increasing number of patients, especially those with a low or intermediate complexity score or those at high surgical risk, will be treated by PCI for LM disease. Patient preference and PCI of high surgical risk patients may now increase the volume of LM PCI.
DIFFERENCES BETWEEN THE LM AND OTHER BIFURCATIONS
The LM is the largest bifurcation of the coronary tree and it provides blood supply to considerably more than 50% of the total myocardial mass. It has a number of unique features, which demand different technical approaches compared with non-LM bifurcations.
These include the following:
– The SB is usually the Cx which most often has a large reference diameter and is angulated, making it difficult to access with guidewires. Acute occlusion of the Cx usually results in considerable ischaemia and may induce acute ischaemic mitral regurgitation. The T-shaped bifurcation angle of the LMS may also affect implantation technique and a highly angulated Cx take-off may impact on prognosis after LM stenting.
– The LM is the only bifurcation where the proximal MB originates directly from the aorta. This increases complexity because of the interaction with the guide catheter and the potential for guidewires to go behind LM stent struts or for stent longitudinal compression.
– The proximal reference diameter may reach >5 mm – which is close to the dilatation limit of many coronary stents.
– Left main trifurcations are encountered in about 10% of LM cases and may require specific treatment strategies.
EBC CONSENSUS ON LM TREATMENT AND TECHNIQUES
A provisional SB stenting approach is recommended for LM treatment in most cases. However, there are occasions where a two-stent strategy is required from the outset of the LM procedure. Initial wiring of the SB is recommended and a careful single-stent approach with POT is particularly applicable because of the changes in vessel calibre proximal and distal to the LM bifurcation.
PCI in the LM should always be regarded as a challenging procedure. Operators and their teams need to be experienced and proficient in rapidly responding to a sudden unplanned deterioration and the requirement for bail-out stenting strategies.
– LM PCI remains challenging and the entire team should be able to manage serious complications.
LESION PREPARATION
Coronary calcification is especially common, and it is likely that adjunctive plaque modification will be required to facilitate optimal stent implantation. This is achieved with either rotational atherectomy, orbital atherectomy and/or cutting/scoring devices. When plaque modification is felt to be unnecessary, either invasive imaging or careful predilation with an appropriately large balloon is recommended to ensure that subsequent stent expansion is possible.
LEFT MAIN STRATEGIES FOR STENTING
LM involvement of the distal bifurcation was noted in 88% of PCI cases in NOBLE; 36% of these were treated with a two-stent technique. Distal LM bifurcation or trifurcation disease was noted in 81% of EXCEL patients. Therefore, operators must have practised for managing the distal LM bifurcation and be intimately familiar with bifurcation stent techniques. Compared with non-LM bifurcations, operators should have a lower threshold for placement of a second stent in the SB. The EBC MAIN study is one of the first randomised clinical trials to compare single versus dual stenting strategies for the treatment of true bifurcation distal LM coronary artery lesions. The first study (DKCRUSH-V) will be presented at TCT 2017.
EBC MAIN is a prospective, multinational, randomised clinical study of LM stem true bifurcation lesions (type 1,1,1 or 0,1,1; both LAD and Cx arteries >2.75 mm diameter) promoted by the EBC group. The study hypothesis is that LM coronary bifurcation lesions are best treated with a planned single-stent strategy rather than a planned dual stent strategy, with respect to death, target lesion revascularisation and myocardial infarction at one year. A total of 450 patients are being enrolled and treated either with a planned single or a planned dual zotarolimus-eluting stent strategy. The decision to “bail out” from a provisional approach to a two-stent strategy will be determined by significant dissection of the SB, especially when it is associated with impaired antegrade flow. Passage of stents around the tortuosity of the Cx can be challenging; this may be a particular consideration when planning an LM procedure. Ensuring that an ostial lesion is covered, without an excessive length of stent protruding into the aorta, is important. This requires imaging in multiple angiographic views and may need further confirmation by IVUS. There is a broad variation of anatomy of the LM between individual patients. The usual dedicated two-stent approaches are T, culotte and TAP, but DK-crush has been demonstrated to have excellent results in expert hands50 (Figure 7).
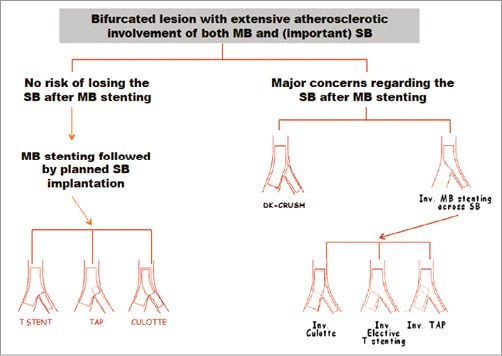
Figure 7. Technical options when two stents are needed.
– Stent implantation involves the bifurcation in 80-90% of LM stenting cases.
– Provisional stenting is the recommended strategy in most distal LM bifurcation lesions.
– Planned two-stent techniques may be indicated in cases with long Cx lesions, high risk of Cx compromise or difficult access.
USE OF OCT AND IVUS IN LM
Angiographic assessment of the LM has several limitations. This calls for a low threshold for use of IVUS or OCT since imaging may influence lesion preparation, as detection of confluent arcs of calcium will usually require the use of adjunctive technology rather than just conventional balloon predilation85,86. Stent malapposition, distortion of stents during rewiring and catheter/guide manipulations in the LM as well as stent undersizing contribute to the long-term risk of stent thrombosis which is potentially catastrophic in the LM.
As a consequence:
– It is strongly recommended to have access to intravascular imaging modalities (IVUS/OCT/optical frequency domain imaging [OFDI]) during elective PCI of the LM.
– It is strongly recommended to use intravascular imaging during LM intervention when the passage of devices during the procedure does not proceed in a predictable way.
FFR IN LM
In the pre-fractional flow reserve era, IVUS was used to assess angiographically intermediate LM disease. Minimal lumen area (MLA) was adopted as a parameter to define whether intervention to the LM could be safely deferred. The currently accepted MLA value of 6 mm2 has been validated against FFR87 and then clinically assessed in a recent study, showing no difference in two-year mortality in patients with deferred LM PCI compared to patients successfully revascularised88. Currently, FFR is probably a better way of determining whether treatment of the LM is required. Importantly, equalisation of the two pressures (Pa: guiding catheter pressure, Pd: pressure by wire transducer) should be performed with the guiding catheter disengaged, especially in the presence of ostial lesions or catheter damping. Pressure wire measurement in either the LAD or LCx should be performed by inducing maximal hyperaemia with intravenous rather than intracoronary adenosine (140 μg/kg/min in infusion). Assessment of the LM by FFR should include measurements of both the LAD and the Cx, including a pullback measurement, to confirm LM disease.
– FFR may be used to determine the indication for LM treatment.
– FFR may be used for safe deferral of Cx treatment if measured after stenting across the Cx ostium85,86.
STENT CHOICE CONSIDERATIONS
Outcomes with modern-generation metallic DES in all-comer PCI demonstrate broadly comparable performance in the short and medium term. However, when stenting the LM, knowing the maximal achievable dimensions with the particular stent platform is especially important8.
Forthcoming studies may inform whether one stent platform offers advantages over another and/or on dual antiplatelet therapy regimens that are specific to LM PCI. Given the lack of specific data and differing mechanical properties of existing BRS, especially with respect to overexpansion, radial strength, and outcomes in two-stent bifurcation treatment, metallic DES are recommended for LM PCI.
Conclusions
The present document from the 12th EBC meeting represents highlights of the current consensus and clinical recommendations of the EBC. It points to the fact that there are a multitude of strategies and approaches to bifurcation stenting within the provisional strategy as well as in all the different two-stent strategies. The decision on which technique to use in a specific lesion is not only a matter of the best fit of a given technique to the anatomy and physiology but, maybe even more importantly, also the technical skills and experience of the operator.
– Keep it simple and safe.
– Limit the numbers of stents.
– Respect the original bifurcation anatomy and try to reproduce it.
– Aim for well apposed and well expanded stents with limited overlap.
The main EBC focus for the years to come is interventional treatment of the LM. Much has already been learned, but the EBC recommendations continue to track a moving target. Much more scientific work is needed to support the improvement of the treatment of bifurcation lesions in coronary artery disease.
Conflict of interest statement
The authors have no conflicts of interest to declare.