Abstract
The European Bifurcation Club (EBC) is an independent, non-political and informal “think tank” of scientists with a particular interest in clinical, technical and fundamental aspects of the management of coronary artery bifurcation disease.
Bifurcations account for 15-20% of all percutaneous coronary interventions (PCI) and remain one of the most challenging lesions in interventional cardiology in terms of procedural success rate as well as long-term cardiac events. The optimal management is, despite a fast growing scientific literature, still the subject of considerable debate, one of the main concerns being the potential increased risk of late stent thrombosis associated with treatment complexity.
The EBC was initiated in 2004 and aims to facilitate an exchange of ideas on management of bifurcation disease. The EBC hosts an annual, compact meeting dedicated to bifurcations which brings together physicians, engineers, biologists, physicists, epidemiologists and statisticians for detailed discussions. Every meeting is finalised with a consensus statement which reflects the unique opportunity of combining the opinion of interventional cardiologists with the opinion of a large variety of other scientists on bifurcation management.
This year the EBC celebrates its 10-year anniversary. This consensus document represents the summary of the consensus from the last ten years of the annual EBC meetings.
“Life can only be understood backwards; but it must be lived forwards.”
Søren Aabye Kierkegaard (1813-1855), Danish philosopher
Introduction
A bifurcation coronary lesion is a lesion occurring at, or adjacent to, a significant division of a major epicardial coronary artery1. A “significant” side branch is most often arbitrarily defined and based upon a subjective judgement of the operator. In practice this implies that a significant side branch is a branch that the operator does not want to lose after evaluating the individual patient in a global context, i.e., patient symptoms, patient comorbidity, diameter and length of side branch, size of the myocardial mass supplied by the side branch, location of ischaemia, viability of the supplied myocardium, collateralising vessel, left ventricular function, results of functional tests, and so forth.
Coronary bifurcations account for 15-20% of all percutaneous coronary interventions (PCI) and remain one of the most challenging lesions in interventional cardiology in terms of procedural success rate as well as long-term cardiac events. The optimal management of bifurcation lesions is still, despite a fast growing scientific literature in the field, the subject of considerable debate, where one of the concerns is the potential increased risk of late stent thrombosis associated with treatment complexity1.
The European Bifurcation Club (EBC)
The EBC was founded in 2004 and the first of its annual meetings was held in Bordeaux in 2005. The aims of the EBC were to devise a common terminology for the description and treatment of bifurcation lesions and to exchange ideas on the clinical, technical and fundamental aspects of the management of bifurcation disease. The club was originally created as an independent, non-political and informal “think tank” of cardiologists, with particular interest in bifurcations with a main agenda of promoting open discussions, exchange of ideas and development of collaborative research within the field of coronary bifurcations. EBC hosts an annual, compact meeting dedicated to bifurcations bringing together physicians, engineers, biologists, physicists, epidemiologists and statisticians for detailed discussions. Every meeting is finalised with a consensus statement on management of coronary bifurcation lesions which reflects the unique opportunity of combining the opinion of interventional cardiologists with the opinion of a large variety of other scientists on bifurcation management.
The present consensus document covers the management of bifurcation lesions including the treatment of the unprotected left main coronary artery, and represents a summary of the consensus from the last ten years of annual meetings of the EBC1-7. Long-term results of larger randomised trials on bifurcation stenting are now available but, due to limited clinical data characterising a number of techniques and individual steps in bifurcation stenting, some of the recommendations provided are based on level of evidence “C”.
Definitions
A simple description of bifurcation lesions, stenosis quantification and PCI techniques is not straightforward, as seen in the introduction of this consensus document. As a consequence, a large part of the first two annual meetings of the EBC was dedicated to the discussion of classification of coronary artery bifurcation lesions and their treatments. The final consensus was reached by promoting a simplified and universal classification of bifurcation lesions, the Medina classification8 (Figure 1), and an accurate definition of each of the various techniques used in bifurcation stenting combined with a precise classification system to facilitate the description, the MADS classification (Figure 2)3. An international consensus on using these simple classifications when reporting studies on bifurcation treatment will considerably improve the interpretation of the published results and are strongly recommended by the EBC.
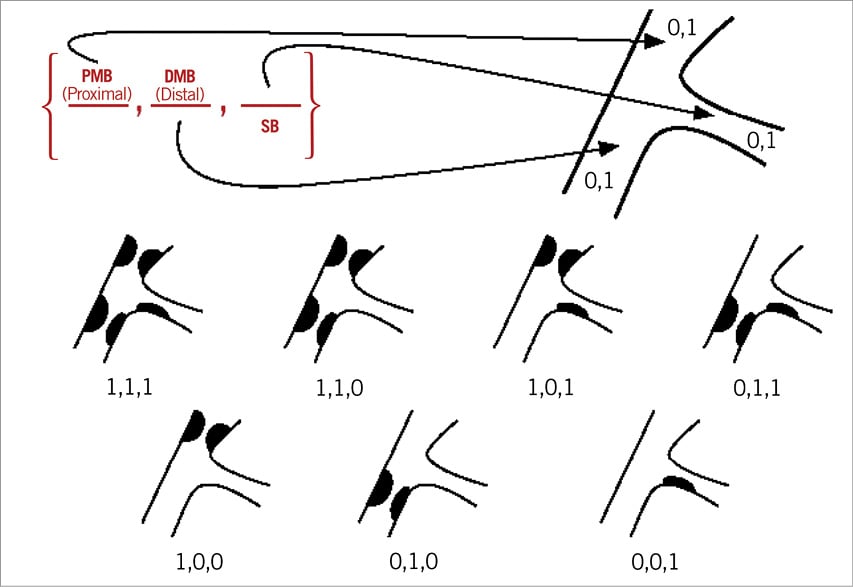
Figure 1. The Medina classification for bifurcation lesions. The ciphers describe, in order, the proximal main vessel, the distal main vessel, and the side branch. The segments are termed “1” if the segment has a diameter stenosis ≥50% by visual estimation, otherwise they are “0”.
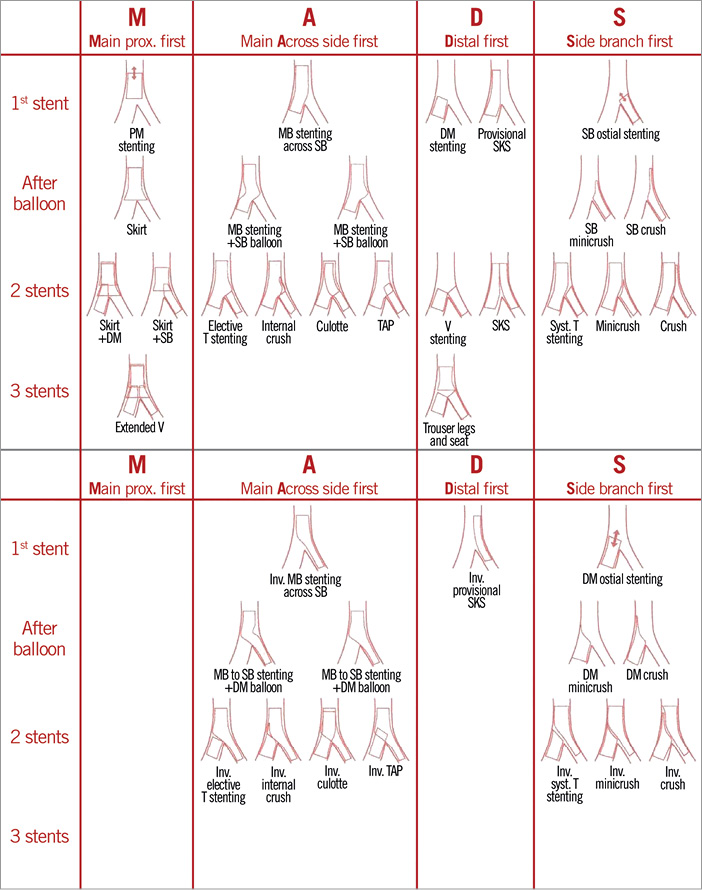
Figure 2. The MADS classification is a systematic description of bifurcation stenting techniques grouped in families.
The Medina classifications may need some refinements to be more descriptive, but the resulting increased complexity was feared to hamper the global adoption of the system and was therefore omitted.
A more precise lesion description might be attained by taking into consideration the angle between the two branches, the side branch (SB) lesion length, the observed/expected diameter, the TIMI flow, and presence of calcification, plaque distribution, as well as ulcerations. Also, more objective measures become increasingly available through physiological assessment, quantitative coronary analysis and use of adjunctive imaging, which may aid the description further.
Bifurcation treatment strategy
Bifurcation treatment techniques should be considered when SB patency might affect prognosis or a side branch stenosis may cause symptoms. A quantitative relation between SB diameter and length and the size of supplied myocardium has been established in swine9,10.
EBC consensus:
– SB diameter and length can both be used visually as surrogates for volume of muscle at risk.
– Wiring of the SB before MV stenting is recommended when the SB is deemed important by the operator.
Relations between vessel diameters
The Murray, Finet, and Huo and Kassab (HK) relations should be kept in mind when evaluating reference sizes of bifurcating vessels11-13. An implication of these relations is that there is always a step down in reference diameter from the proximal MV to the distal MV in bifurcations. The HK model has been found to be in agreement with all bifurcation types13 and is recommended. Table 1 shows a practical scheme of branch size relations, or calculations can be performed using http://www.et.iupui.edu/cnc/refdiacalculation.aspx#sthash.DAK3zn93.dpuf
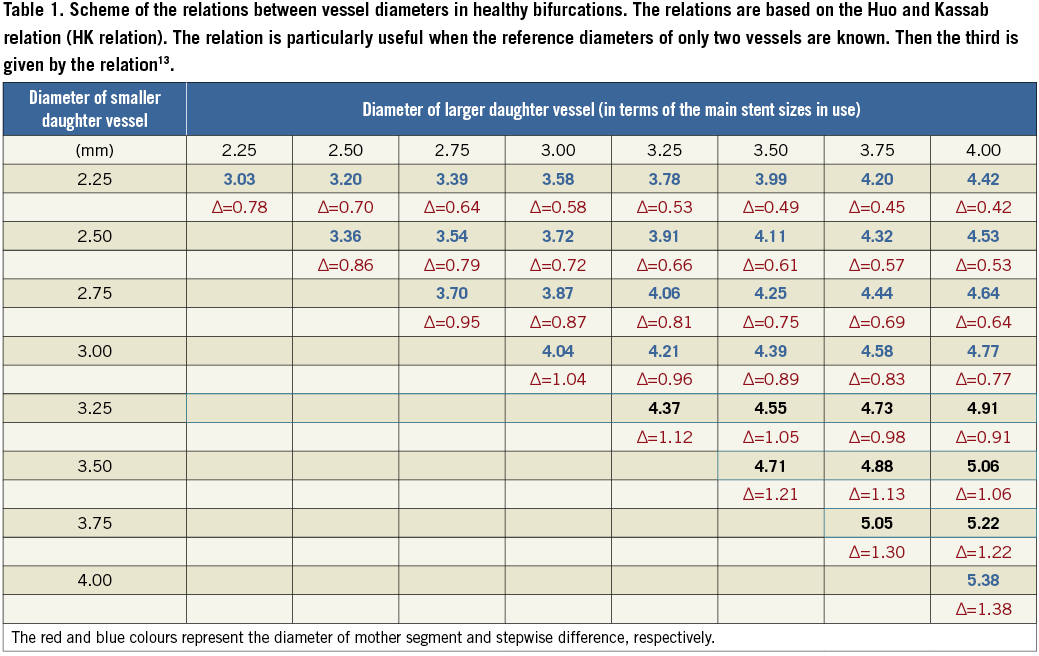
The relation between the bifurcation vessel segments may be used for estimating optimal reference sizing for a vessel, knowing the size of the two other vessels. This is of particular value when the reference diameter for one vessel cannot be estimated directly.
Planning the procedure. One, or two-stent technique?
Based on multiple randomised trials and registries of one versus two-stent techniques in coronary bifurcation lesions, and based on the KISSS principle (Keep it simple, swift and safe)14-18, the EBC recommends the provisional stenting technique as the preferred technique for the majority of bifurcation lesions. In this technique the main vessel (MV) is stented first and the side branch (SB) is only stented in case of severe restenosis or flow limitations to the side branch (provisional SB stenting) after MV stenting. Most of the available literature comparing one versus two-stent techniques is burdened with a design dilemma. The populations in most of the published studies favour the provisional technique, because of inclusion of non-true bifurcations, and inclusion of bifurcations with SB diameter below 2.5 mm. The recently presented randomised Nordic-Baltic IV trial (TCT 2013) showed a trend towards improved midterm outcome when using a two-stent technique compared to provisional stenting in bifurcations with large SBs (≥2.75 mm) having more than 50% diameter stenosis in the SB. A similar signal was supported by the DKCRUSH II trial19 and by a subgroup analysis of the Tryton IDE study (EuroPCR 2014). The EBC II trial on provisional technique vs. culotte two-stent technique in bifurcation lesions (SBs ≥2.50 mm and more than 50% SB diameter stenosis) may provide further information on the role of two-stent techniques in this subset of bifurcations. Until then, a two-stent technique may be considered up-front for bifurcations with large SB (ref. diameter ≥2.75 mm) and significant disease extending into the SB.
Another design dilemma was the inclusion of non-prognostic periprocedural biomarker release in composite primary endpoints favouring provisional stenting. Periprocedural myocardial infarctions may be prognostic when baseline markers are normal and CK-MB is increased at least to 8-10 times the upper limit of the 99% confidence interval or ECG indicates Q-wave infarction20.
From a technical point of view, it is important to decide beforehand whether to use two stents. When using the provisional T strategy, the operator is restricted in all cases to using a technique where the SB is stented through the MV stent. This technique has an inborn risk of missing coverage of the SB or protruding into the MV. This problem can only be solved by using a provisional culotte technique, which, however, is more technically demanding. The technical result might be better in a two-stent technique if the SB is stented first, resulting in a satisfying result in the MV, but also in a more complex procedure than a provisional approach where SB stenting is not needed. The problem of choosing between a one and a two-stent technique before the start of the procedure is that it is difficult to predict the need for SB stenting before the main branch stent is placed. If the SB needs to be secured with a stent first (because of difficult wiring or because it supplies a large territory), the procedure will most likely end with a two-stent technique. These considerations constitute the true dilemma of bifurcation treatment (as Kierkegaard states: “Life can only be understood backwards; but it must be lived forwards”).
EBC consensus:
– Main vessel (MV) stenting with provisional SB treatment, if needed, is recommended as the preferred technique for the majority of bifurcation lesions.
– Large SBs with significant ostial disease extending further into the SB are likely to require a two-stent strategy.
– Larger SBs whose access is particularly challenging should be secured by stenting once accessed.
The provisional technique
Predilatation of the SB before MV stenting has been intensively discussed and until recently there were no firm data available to clarify the topic. Potential advantages of SB predilatation include increased ostial SB lumen, and furthermore it might be the definitive SB treatment avoiding rewiring and post-dilatation of the SB. In case rewiring is needed, it might be facilitated by the SB predilatation. Disadvantages might include the risk of inflicting dissections and thus increasing the risk of rewiring a dissection. A dissection might also lead to increased SB stenting. Further, if subsequent kissing balloon dilatation is not performed, the SB ostium is not scaffolded by the MV stent and this potentially increases the risk of restenosis. An observational study with a propensity-matched analysis indicated increased risk of target lesion failure if the SB was predilated21. However, when tested in a randomised trial of patients treated with provisional T-stenting, including only true bifurcation lesions, it was found that SB predilatation was associated with improved TIMI flow, less indication to treat the SB, a similar low rate of SB stenting and similar clinical midterm outcome. Furthermore, this strategy has technical advantages by reducing the different steps needed in the treatment and thereby simplifying the stenting procedure22.
Drug-eluting stents are recommended for bifurcation treatment23. The MV stent should be sized according to the distal MV reference diameter24,25. Adequate apposition in the proximal MB should be achieved by the proximal optimisation technique (see opposite). It is important to choose a stent where the platform in that particular nominal diameter accommodates expansion to the reference diameter of the proximal MV segment26 (Figure 3).
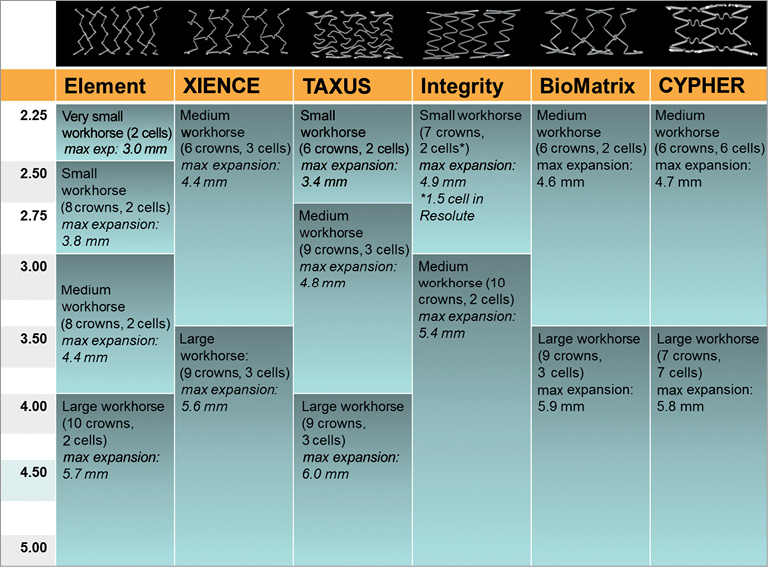
Figure 3. Maximum expansion capacity of stents and the size-dependent platforms. In sizing the stent according to the distal main vessel, it is important that the chosen stent and size allow for adequate expansion in the proximal main vessel segment26.
EBC consensus:
– The MV stent should be sized according to the distal MV reference diameter.
– The MV stent should allow for expansion to the reference diameter of the proximal main vessel.
– Predilatation of the SB is in most cases probably not needed, but may be considered.
– Predilatation of the SB is recommended in some circumstances (extensive ostial SB involvement, heavy calcification, etc.), even with a provisional SB stenting approach.
The proximal optimisation technique
The proximal optimisation technique (POT) was described by Darremont as a method of expanding the stent from the proximal stent edge to just proximal to the carina, using a short oversized balloon6 (Figure 4). Based on in vitro and virtual bench tests, it has been shown that POT might be used to ensure adequate stent apposition in the proximal MV, especially in the case of large reference vessel diameter differences between the proximal and distal MV. Furthermore, in the case of difficult SB rewiring, the POT might be used to facilitate easier SB access due to the oblique take-off in the direction of the SB27. Opinion remains divided as to whether POT should be a part of the routine approach to bifurcation lesions.
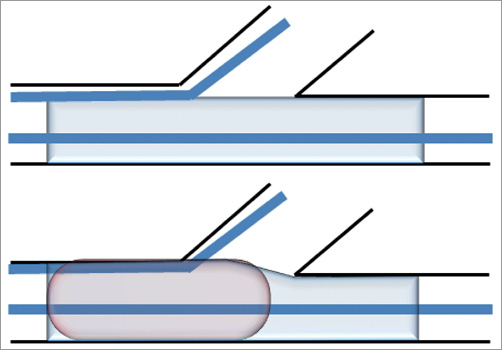
Figure 4. The POT in provisional stenting. After implantation of the main vessel stent, sized according to the distal reference diameter (proximal panel), the proximal main vessel is post-dilated using a non-compliant balloon (distal panel). The balloon size matches the proximal main vessel reference diameter.
EBC consensus:
– The POT may be used in cases with large differences in reference diameter between proximal and distal MV.
– The POT might be used to aid difficult recrossing into a SB with either a wire or a balloon.
Difficult side branch access
Specific tools and techniques have been devised for SB wiring when difficult. Factors affecting wiring of SBs include severe proximal MV stenosis, ostial stenosis, steep angulation and lower than TIMI 3 flow28. Wiring techniques include wire selection, use of hydrophilic wires29 that might pass more easily but might also increase the risk of dissections. Mastering the “reverse wire technique” may be of particular value28 (Figure 5), as would be the use of microcatheters29. It was agreed that, in difficult cases, plaque modification by balloon dilatations or rotablation of appropriate lesions might aid primary wiring.
EBC consensus:
– Techniques for difficult SB access include lesion preparation, wire selection, the “reverse wire technique” and use of microcatheters.
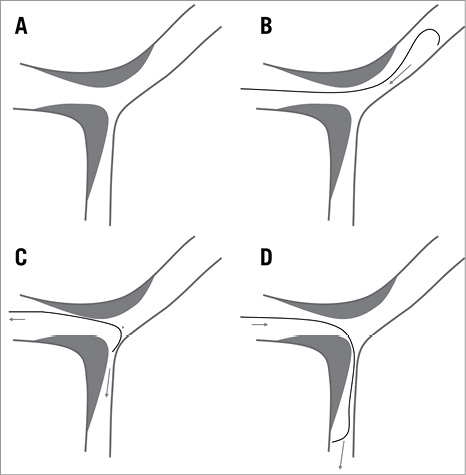
Figure 5. The reverse wire technique. (A) A Medina 1,1,1 bifurcation with an unfavourable 90° angle. A smoothly curved guidewire is advanced to the distal main vessel making a hook-like bend (B). Then retract the wire towards the bifurcation to engage the side branch (C). Turning the wire advances the guidewire in the side branch (D)28.
Difficult SB rewiring
If treating the SB after MV stenting is important (≥75% or TIMI flow <3) but recrossing the wire into the SB is not possible, SB access may be performed by: 1) leaving an uninflated balloon in the MV, 2) then advancing a low-profile 1.25 mm balloon catheter on the jailed wire, 3) dilating a tunnel for an appropriately sized SB balloon to be advanced, and 4) advancing an appropriately sized SB balloon and dilating the SB. The procedure can be finalised in multiple ways (T-stenting, TAP stenting, internal crush30 and more, or just kissing balloon dilatation). Ensure re-expansion of the proximal MV stent and evaluate wire positions at all times.
EBC consensus:
– SB rewiring might be facilitated by POT.
If SB rewiring is not possible, SB dilatation after MV stenting might be performed by jailed wire SB access.
Kissing balloon inflations in simple stenting
No clinical advantage of a routine kissing strategy in single-stent treatment has been shown31-34. Theoretical advantages of kissing balloon inflation after single-stent treatment include restoration of anatomy35,36, expansion of the proximal MV, apposition of jailing struts and balloon treatment of ostial SB lesions. Disadvantages include increased procedural complexity31, risk of SB dissection, risk of creating a metal carina37, stent distortion and accidental stent crush by proximal abluminal rewiring.
Routine kissing inflations using the provisional technique have caused significant debate during the EBC meetings. It was agreed that, in the absence of an angiographically tight lesion at the ostium of the SB after MV stenting, kissing balloon inflations are not routinely required. When a tight lesion (>75% DS or TIMI flow <3) is present in the SB after MV stenting, it is known that kissing balloon inflation will reduce the physiologically significant proportion of SBs from 30% to 5%38. Therefore, kissing balloon dilatation may be performed in angiographically significant (>75% DS or TIMI flow <3) ostial SB lesions as there appears to be no overall penalty for doing so31. It is unknown if FFR-guided SB intervention in non-LMCA bifurcations provides improved clinical outcome compared to angiographically guided SB intervention (see section on FFR).
EBC consensus:
– Kissing balloon inflations may be used when an angiographically significant (>75% DS or TIMI flow <3) ostial SB lesion remains after MV stenting.
Optimising kissing balloon inflation in single-stent techniques
An MV stent becomes distorted after SB balloon inflation, and this may not be fully corrected by kissing balloon inflation35,39. The degree of distortion, and particularly the size of the metallic carina made up of struts, partly jailing the distal MV, is dictated mainly by the SB crossing point. Distal recrossing promotes better ostial SB stent coverage and apposition, whereas proximal recrossing offers less optimal SB coverage and causes metal overhang into the MV36,37,40,41 (Figure 6). Distal recrossing may be achieved by “pullback rewiring”: advancing the guidewire with bended tip into the distal MV and then carefully retracting the wire while turning and directing it towards the SB. Wire position may be verified by OCT41-43. Sequential inflations in the SB and MV compared to final KBD caused higher rates of TIMI flow <3 in a small clinical series44, but an optimised sequence including POT showed favourable results compared to KBD in bench testing and modelling35. The optimal inflation sequence is still uncertain but deflation should be performed by simultaneous deflation of the balloons to avoid distorting the MV stent40.
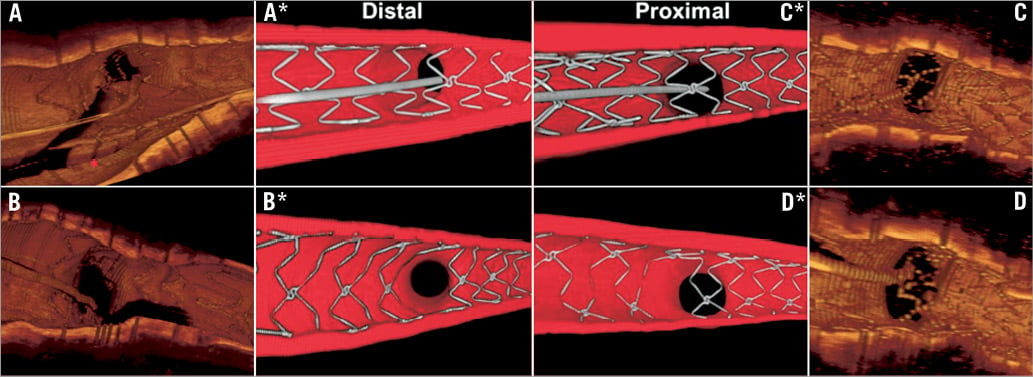
Figure 6. Evaluation of wire position using 3D OCT. Recrossing into the SB via distal stent cell (A and A*). Result in same patient after kissing balloon inflation (B and B*). Proximal recrossing (C and C*) and the result with struts extending proximal from the carina, “metallic carina”. (D and D*) Images with * are from a representative coronary bifurcation bench model78.
When rewiring an SB, efforts should be made to cross the MV stent distally, thereby limiting the formation of a metal carina and ensuring stent coverage of the proximal part of the ostium of the SB.
Use of non-compliant balloons for kissing
Non-compliant balloons allow high-pressure individual inflations and, if necessary, kissing inflations following bifurcation stenting. In single-vessel stenting, high pressure ostial SB dilatation is not usually required and carries a risk of SB dissection. Higher pressures can be achieved with non-compliant balloons without overdilating the vessel45. In stenting both vessels, high-pressure ostial and MV dilatation is mandatory to achieve full stent expansion at both ostia, preferably by inflating the balloon in the SB first followed by the balloon in the MB, finalised by a lower pressure kissing inflation for carina optimisation35,46.
EBC consensus:
– Non-compliant balloons are recommended for kissing inflations.
– Individual non-compliant high-pressure “ostial” post-inflations are mandatory in complex stenting techniques to achieve full cell opening and stent expansion.
Provisional stenting of the side branch
Using the provisional strategy, stenting of the SB is indicated by major SB dissections or compromised SB flow after kissing balloon dilatation. The SB is first predilated after rewiring the SB through the main vessel stent. Depending on the angulation of the SB offspring (i.e., the potential SB stent protrusion inside the MV stent when ensuring complete ostial coverage), the following techniques are proposed. 1) The SB stent may be deployed as T-stenting when the angulation is near 90 degrees. Precise deployment of the SB stent at the ostium is crucial (without protrusion inside the MV stent). 2) T-and-protrusion (TAP) stenting is a very simple approach for bail-out SB stenting where the SB stent is deployed with minimal protrusion while maintaining an uninflated balloon in the MV. Retract the SB stent balloon slightly and perform kissing balloon dilatation47. The TAP technique eliminates the need for a second SB rewiring but might produce a longer metal carina in narrow angle bifurcations. 3) More protrusion of the SB stent inside the MV stent represents an internal mini-crush technique and may also be used in less angulated bifurcations36,40. Internal crush is fast and theoretically easier to rewire than classic and mini-crush, owing to the single jailing strut layer, but is limited by the maximum cell size of the main vessel stent and by the resulting triple strut layer often present in the proximal MV. 4) Finally, provisional culotte, with proximal overlap of two stents, might be used in cases with limited difference in reference diameters between SB and MV. The technique still requires rewiring of the MV, which might be an undesirable step in the bail-out situation.
EBC consensus:
– When an SB stent becomes necessary in provisional stenting, T-stenting, TAP-stenting, internal mini-crush and culotte stenting are recommended. Optimal choice depends mainly on angulation.
– Internal crush and culotte require a second SB or MV rewiring compared to T and TAP.
Planned two-stent techniques
Predilatation of both MV and SB is recommended. Only areas to be covered by stents should be predilated. Each two-stent technique has specific properties and it is advisable to master more than one technique. Still, operator preferences and skills may be important in performing a two-stent technique. Two-stent techniques with treatment of the MV first may be performed in large SBs (≥2.75 mm) with >5 mm SB lesion extending from the ostium (Nordic-Baltic IV, TCT 2013). SB first two-stent techniques should be considered if the SB has difficult access, dissections, high risk of closure or need for multiple stents to cover downstream SB lesions. Final KBD in two-stent techniques has not been evaluated in randomised clinical studies but patients without final KBD had consistently worse outcome in Nordic II46 (crush vs. culotte two-stent techniques) and in registries33,48,49.
EBC consensus:
– Operator experience may be important when choosing a two-stent technique.
– Two-stent techniques with deployment of the MV stent first are recommended.
– SB first two-stent techniques may be considered when the SB has particularly difficult access, dissections after predilatation or downstream stenoses to be stented.
– Final kissing balloon dilatation is mandatory in any two-stent technique.
Culotte technique
Culotte has been thoroughly described and evaluated in randomised studies with similar clinical results compared to mini-crush and favourably compares with T-stenting46,50, but also has higher repeat revascularisation after angiographic FU compared to DK-crush51. In contemporary culotte stenting, proximal optimisation (POT) is recommended after first and second stent deployment, as well as a final POT after kissing balloon inflation. It is advisable to avoid a long overlap of stents in the proximal MV whenever possible.
EBC consensus:
– Culotte is recommended for two-stent treatment of bifurcation lesions.
– When using the culotte technique, “mini-culotte” with as less proximal a double layer of stent struts as possible is recommended.
Crush techniques
The crush technique has multiple modifications. The mini-crush technique is recommended over classic crush to avoid the large area of three strut layers in the proximal MV52. The location of recrossing may affect the acute results of crush stenting, with potential gap formation at the SB ostium if recrossing is too proximal or too distal52. Rates of successful kissing balloon inflation in crush stenting are 75-90%16,46, thus lower than for culotte stenting. The double kissing modification (DK-crush) may aid recrossing into the SB after MV stenting19,51,53. DK-crush also increases the expanded stent cell area in front of the SB detectable at follow-up54.
EBC consensus:
– Crush should be performed as mini-crush to reduce the extent of multiple strut layers in the MV.
– The DK-crush modification may aid rewiring the SB after MV stenting.
T-stenting techniques
T-stenting is appropriate for near 90 degree bifurcations. It is important to deploy the SB stent at the ostium to avoid uncovered areas17. The T-and-protrusion (TAP) technique is optimal for provisional SB stenting if the angle is less than 90 degrees47,55.
EBC consensus:
– T-stenting is appropriate for near 90 degree bifurcations.
– TAP stenting may also be used in smaller angles.
V-stent technique
The V-stenting technique has theoretical advantages in narrow angle bifurcations but can be technically demanding to get an optimal result and requires three stents for a Medina 1,1,1 lesion.
EBC consensus:
– V-stent technique might be used in appropriate narrow angle bifurcations.
SKS technique
The simultaneous kissing stents technique is very fast using simultaneous deployment of the MV and the SB stent. The potential risk of the resulting long metal carina is debated and according to the present evidence level56,57 the SKS technique is not recommended for routine two-stent treatment.
EBC consensus:
– SKS stenting is not recommended as a routine two-stent technique.
Optimising kissing balloon inflation in two-stent techniques
Using the crush technique, rewiring the SB through a proximal stent cell may increase SB restenosis58. It is unknown if recrossing a distal stent cell when rewiring the SB offsets the potential risk of abluminal rewiring of a malapposed SB stent59. Thus, it might be advisable to avoid far distal recrossing and aim for a middle to distal position. Rewiring the MV in culotte, a crossing position near the carina may limit the length of a “metal carina”. Verification of wire positions by OCT might be considered. The reconstruction of the carina by kissing balloon inflation in two-stent techniques often results in oval-shaped distortion of the proximal part of the stents. Final proximal MV high-pressure inflation using a non-compliant balloon can correct proximal distortion, although the clinical importance of this step is unknown27.
EBC consensus:
– Kissing balloon inflation for carina reconstruction is mandatory in two-stent techniques.
– Final post-dilatation of the proximal MV segment may be considered for reducing malapposition of multiple strut layers and for correction of proximal stent distortion after kissing balloon inflation.
PCI or CABG for distal left main bifurcation lesions
Coronary artery bypass grafting (CABG) is the treatment for LMCA lesions with the highest level of guideline recommendations. Percutaneous coronary intervention (PCI) has increased in evidence level, now class IIa for ostial and trunk LMCA lesions and IIb for distal LMCA bifurcation treatment60,61. These lesion-specific recommendations need to be integrated with other lesion and clinical information, and a Heart Team evaluation of patients with LMCA lesions is recommended61. Awaiting the dedicated randomised trials (NOBLE, EXCEL) comparing PCI and CABG for LMCA stenoses, a meta-analysis indicates that PCI may have similar clinical outcome compared to CABG when PCI is deemed feasible by the operator62. Differences in outcome include higher rates of repeat intervention after PCI and higher rates of cerebral infarction after CABG63. PCI of LMCA bifurcation lesions has been associated with worse outcome than PCI of ostial and shaft lesions64.
EBC consensus:
– LMCA treatment by PCI and CABG may have similar safety outcome. PCI has a lower risk of stroke but a higher risk of repeat intervention.
– LMCA bifurcation treatment is associated with worse prognosis than ostial and shaft LMCA treatment.
– Heart Team evaluation is recommended in the decision between CABG and PCI for LMCA treatment.
PCI of the unprotected distal left main coronary artery bifurcation
The provisional strategy is preferred in most LMCA bifurcation lesions as in non-LMCA bifurcations. The above recommendations for bifurcation treatment apply also to LMCA treatment with the following modifications. The circumflex artery (Cx) is almost always considered a major SB thus favouring a two-stent technique in case of significant and extended proximal Cx disease. In patients with stable coronary artery disease, FFR may be used for evaluation of physiological significance of both MV and side branch65. Intravascular imaging (IVUS or OCT) is recommended for sizing bifurcation stents and may also be used for evaluating lesion significance in cases where FFR is not possible or difficult to interpret due to downstream stenoses. Various cut-off values for determining physiological significance have been proposed. The most robust is that in isolated LMCA disease an MLA <4.8 mm2 is a predictor of FFR <0.8066.
EBC consensus:
– FFR may be used for evaluating LMCA bifurcation lesions in stable patients.
– Intracoronary imaging may be used for evaluating significance and lesion distribution, and is recommended for the sizing of stents.
– Provisional stenting is the preferred strategy in LMCA bifurcation lesions.
POT may be of particular importance after MV implantation to avoid collision of the guiding catheter and the unsupported stent as well as to avoid abluminal rewiring by a second wire. It is important to know the maximum expansion capacity of stents planned for extending into the LMCA (MV stents, culotte)26.
EBC consensus:
– POT may be of particular importance in LMCA bifurcation treatment.
Two-stent techniques for LMCA bifurcation treatment
T-stenting, TAP, DK-crush and culotte may be used according to the bifurcation angle.
Expansion according to the reference size of the individual segments is recommended. Cut-off values for MLA after stenting in the LMCA bifurcation segments predicting in-stent restenosis are: ostial Cx - 5.0 mm2, ostial LAD - 6.3 mm2, LMCA bifurcation segment - 7.2 mm2, and LMCA - 8.2 mm2 67. These numbers have been derived from an Asian population and thus might be slightly higher for a Caucasian population.
EBC consensus:
– Intracoronary imaging is recommended to ensure adequate stent and vessel expansion in all LMCA bifurcation segments.
Dedicated bifurcation stent systems
The aim of dedicated bifurcation stent systems is to provide simple and safe treatment of bifurcations without the need to fit a straight tube-shaped structure to the bifurcation and work through the stent strut cells of a workhorse stent. None of the currently available systems can challenge the excellent results offered by the provisional T-stent strategy using workhorse drug-eluting stents.
EBC consensus:
– Dedicated bifurcation stent systems remain limited, but use of optimal systems in bifurcations needing a two-stent technique may prove of value.
Adjunctive intracoronary imaging in bifurcation treatment
Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) may provide crucial information in guiding bifurcation treatment. Both modalities are feasible with the provisos that present IVUS catheters have a higher crossing profile and provide lower resolution compared to OCT, and that OCT may increase use of contrast and does not allow for aorto-ostial assessments68. At present, crossing into a jailed SB using IVUS or OCT wires is not advised, as they might distort or fracture69 the stent. Both modalities may be used for assessment of lesion composition and distribution, results of predilatation, reference sizing and evaluation of adequate vessel expansion after stenting70-72. Before stenting, the deeper tissue penetration by IVUS may aid reference sizing in diffusely diseased vessels73,74, whereas OCT often allows for assessment of the thickness of calcium to conquer, detection of thin-cap fibroatheromas, thrombus and small dissections71. After stenting, both IVUS and OCT may be used to evaluate vessel expansion, stent distortion and detection of malapposition. OCT is capable of detecting lower grades of malapposition than IVUS75-77. Evaluation of wire positions is of particular value in bifurcation treatment and is readily performed by OCT, especially 3D OCT41-43,78 (Figure 6). Unintended abluminal rewiring may also be detected using OCT (Holm, EBC 2013). Very careful IVUS examination might also reveal wire positions.
EBC consensus:
– IVUS and OCT may be of particular value in guiding bifurcation treatment and are recommended for left main bifurcation treatment.
– Wiring of jailed SBs with imaging wires should be avoided due to the risk of distorting the stent.
– Segments overlapping on angiography (often the SB ostium) can be evaluated by intracoronary imaging. OCT may be superior to IVUS in evaluation of the SB ostium by MV pullback.
– Evaluation of wire positions may be of importance whenever crossing stents in single and double stenting.
– Intracoronary evaluation of optimal vessel and stent expansion is superior to angiographic assessment.
– Pullbacks in both SB and MV are recommended in evaluation of two-stent techniques if intracoronary imaging is used.
Quantitative coronary analysis (QCA) of bifurcations
QCA in the evaluation of bifurcations has been widely utilised for guiding treatment and for scientific work-up. Dedicated bifurcation 2D QCA software is recommended4, being superior to straight vessel QCA applied in bifurcations79,80. Dedicated software enables integrated assessment of the reference function including the MV step-down, measurement of angulations between vessels and reporting in segmental models81,82. Application of 3D bifurcation QCA increases the accuracy of lumen measurements and assessment of angulations83-86. Furthermore, 3D QCA enables calculation of the optimal projection angle in bifurcations87. Uses of 3D QCA for multiple purposes that may be of future relevance for bifurcation assessment and treatment include co-registration to OCT and IVUS88, a roadmap for centreline-adjusted OCT in bifurcations89 and for computing FFR without the use of a pressure wire90-92. Use of on-line QCA for improving clinical outcome after bifurcation treatment has yet to be investigated.
EBC consensus:
– QCA software dedicated to bifurcations is recommended over straight vessel QCA software.
– 3D QCA provides more accurate measurements than 2D QCA.
– QCA may aid sizing of coronary stents but clinical value is unknown.
Use of fractional flow reserve (FFR) in bifurcations
Main vessel assessment is recommended according to ESC guidelines - in patients with stable angina pectoris when other objective evidence of ischaemia is not available61. SB evaluation by FFR has provided valuable information on the relation between physiological and angiographic evaluation38,76,93. Routine SB FFR, before or after MV stenting, is debated, as safety concerns remain and also because of the difficulties in using FFR in bifurcations if the proximal MV is involved (Medina 1,1,1, 1,0,1, 1,0,0)94,95. Further, the validity of SB FFR after MV stenting may be controversial due to local oedema, thrombus and debris in the ostium, and distal embolisation94,96.
EBC consensus:
– MV FFR is recommended in stable patients when no other objective evidence of ischaemia is available.
– Routine SB FFR is debated due to safety concerns and due to unknown validity when performed after MV stenting. Primary Cx FFR evaluation carries no known increased safety concerns.
Bioresorbable scaffolds (BRS) in bifurcation lesions
The bioresorbable everolimus-eluting stent (the Absorb™ BRS; Abbott Vascular, Santa Clara, CA, USA) has a bioabsorbable polymer backbone made of poly-L-lactic acid (PLLA) and a polymer coating of poly-D,L-lactide that releases everolimus. Although the available randomised trials evaluating BRS technology have excluded bifurcation lesions with SB exceeding or equal to 2 mm diameter, in vitro testing and the limited clinical data available on BRS use in bifurcation lesions (case reports and small case series) were presented and discussed during the 9th European Bifurcation Club (EBC) meeting. The general recommendation was that implantation of BRS in bifurcations with SB diameter larger than 2 mm should preferably only be done in randomised trials until firm data on efficacy and safety were present. For SBs with a diameter of less than 2 mm, the consensus reached represents a modification of the EBC recommendations for metallic stent deployment7 and could be applied to treatment of coronary bifurcations with a side branch diameter less than 2 mm. Further confirmation is needed in standardised bench-testing models and appropriately designed clinical studies (both observational and randomised) before applying these techniques to treat coronary bifurcations with side branches ≥2.0 mm.
Provisional strategy utilising BRS
The provisional approach remains the default technique with BRS. A few specific caveats must be considered.
Stent selection is still intensely debated and it seems to be a real dilemma as to which strategy should be recommended in different anatomies. One approach is to select the stent according to distal reference in the MV, similar to the recommendation with metallic stents. This strategy, however, may have restrictions when post-dilating the proximal MV due to the mechanical limitations of expanding the stent. In suitable anatomies, another strategy could be to select the stent according to proximal MV diameter and to deploy at low pressure in order to avoid damaging the distal vessel, followed by adequate post-dilatation of the proximal segment97. In conclusion, the decision on sizing the stent according to the proximal or distal reference diameter depends on the individual coronary anatomy of the patient and is, in the end, the decision of the operator.
Deployment strategy:
increase balloon pressure progressively (2 atm every 5 seconds) up to nominal pressure. Inflation duration of 30 seconds or more is recommended.
Optimisation strategy:
based on Murray’s law, POT is recommended with BRS but restricted to non-compliant (NC) balloon 0.5 mm larger than the reference using the Absorb BRS, as stretching with larger diameter balloon may cause BRS strut fracture in the proximal vessel.
If no SB compromise, procedure is finished.
If SB is compromised, open a cell with an undersized NC balloon (≤2.5 mm) and use POT with a larger balloon in the proximal MV to correct scaffold malapposition (the sequential strategy: POT+SB opening+final POT)97,98. A final OCT pullback in the MV should be performed to confirm adequate strut apposition in the distal and the proximal segment.
Routine final kissing balloon dilatation (FKBD) is not recommended. Recently, mini-FKBD was proposed (“snuggle balloon dilatation”), with minimal overlap of two balloons, positioning the proximal marker of the SB balloon in the MV immediately proximal to the SB ostium and low-pressure inflation (5 atm)99,100. Higher pressures increase the risk of strut fracture.
SB stenting strategies using BRS
Because of limited experience available for SB stenting strategy following BRS implantation in the MV, a preliminary consensus is proposed.
Based on insights from bench testing and initial clinical reports, when SB stenting is required as a crossover from provisional, metallic stent or BRS implantation in the SB should be considered utilising either the T or the TAP stenting technique97,99,101,102.
Likewise, when stenting of both branches was planned from the beginning, either a BRS or a metallic stent was evaluated for the SB101,102. When a metallic stent was implanted in the SB as a planned two-stent strategy, feasibility of the mini-crush technique was tested in vitro101. The culotte and the crush stenting techniques should be avoided to prevent scaffold strut fractures and excessive overlap due to the thickness of the struts.
Before a firm recommendation on clinical application can be made, all two-stent techniques require careful evaluation in fractal bench-testing models with different bifurcation angles. Finally, head-to-head evaluation in large randomised trials is needed.
Although BRS technology is still in its infancy, in vitro testing and initial clinical results in bifurcation lesions seem promising. Present recommendations apply to the Absorb™ BRS and may need to be revised with other stent designs, including the magnesium-based BRS which may behave in a more well-known pattern as known from other metallic stents.
Conclusion
The EBC’s 10-year anniversary consensus document is the up-to-date recommendation on management of coronary bifurcation lesions, and is based on the first 10 year’s meetings and consensus documents. In 2012, the EBC changed status to a formal independent club with its own bylaws and a constituted board of directors with the aim of being a non-political think tank of dedicated specialists with a particular interest in bifurcations. The club will continue to promote open discussions and exchanges of ideas, and to aim towards the development of collaborative research. Furthermore, the EBC will continue to publish a yearly consensus statement on bifurcation management.
Conflict of interest statement
The authors have no conflicts of interest to declare.

