Abstract
The European Bifurcation Club recommends an approach to a bifurcation stenosis which involves careful assessment, planning and a sequential provisional approach. In the minority of lesions where two stents are required, careful deployment and optimal expansion are essential to achieve a long-term result.
Abbreviations
| EBC | European Bifurcation Club |
| IVUS | intravascular ultrasound |
| LAD | left anterior descending |
| LCx | left circumflex |
| LMCA | left main coronary artery |
| MB | main branch |
| OCT | optical coherence tomography |
| POT | proximal optimisation technique |
| SB | side branch |
Introduction
The European Bifurcation Club (EBC) was inaugurated in 2004 with the objective of facilitating scientific discussion and an exchange of ideas on the optimal management of bifurcation lesions. Since then the EBC has held an annual meeting which brings together physicians, pathologists, engineers, biologists, physicists, mathematicians, epidemiologists and statisticians. Each meeting has been finalised by the production of a consensus statement that combines these opinions on bifurcation management.
This document represents the summary and recommendations from the 14th annual EBC meeting held in Brussels in 2018. Recent specific publications from the EBC have included consensus statements on left main treatment (13th consensus)1, intravascular ultrasound (IVUS) in the left main bifurcation2, optical coherence tomography (OCT) in bifurcation treatment3, a consensus on the role of bench testing in bifurcations4, and the use of quantitative angiography methods in bifurcations5. Reference to these documents is made throughout the text and readers are encouraged to refer to these original documents for further detailed information.
The EBC ethos of treatment for bifurcation
Use of a provisional side branch (SB) stenting strategy is one of the fundamental philosophies of the EBC and consequently the use of a second stent during bifurcation treatment is mandated only under specific circumstances. Recommendation of an intentional (up-front) two-stent approach is unusual but it is recognised that there are circumstances where this is desirable and represents optimal practice. The EBC promotes a simple description of bifurcation lesions and recommends routine use of the Medina classification6 in clinical practice.
In this new consensus, an updated MADS7 classification is described with accurate definition of each of the various techniques used in bifurcation stenting combined with a precise classification system to facilitate the description. We hope that this will allow clearer database recording of interventional procedures and the opportunity to standardise reports and facilitate future comparison(s). The decision on which technique to use in a specific bifurcation lesion involves not only a matter of the best fit of a given technique to the anatomy and physiology, but also the technical skills and experience of the operator. The EBC principles are:
− Keep it simple and safe
− Understand and respect the original bifurcation anatomy
− Optimise the flow and function of a bifurcation following percutaneous intervention
− Limit the number of stents which should be well apposed and expanded with limited overlap.
Update on provisional bifurcation stenting strategy
The provisional SB stenting strategy is the “standard” approach for treatment of most bifurcation lesions8. A review of the sequence of the provisional approach was provided in the 12th consensus statement9. In this 14th consensus statement, particular detail and contemporary insights are provided on 1) evaluation of the importance of the side branch based on data from both computed tomography (CT) and physiological testing, 2) how to perform the proximal optimisation technique (POT) correctly, and 3) discussion of the advantages/considerations of POT/kiss/POT vs. POT/side/POT.
Almost all bifurcation lesions – including the distal left main coronary artery (LMCA) – can be safely treated via the radial artery approach with a large-lumen 6 Fr guiding catheter.
OPTIMAL ANGIOGRAPHIC VIEW
Given the tri-dimensional structure of bifurcations, it is impossible to avoid foreshortening when trying to obtain a clear image of the three bifurcation segments. Consequently, it is necessary to record several views from various angles. The point of the SB take-off is the crucial point, which is rarely visualised adequately from two routine orthogonal views; views should be explored to find “the working view”. An optimal view of the left circumflex (LCx) ostium can be difficult to acquire; when this situation arises, the use of intravascular imaging is especially important. Using diagnostic angiographic images, three-dimensional (3D) QCA images can be created and used to inform procedural planning10. Increasingly, patients presenting with stable angina will have undergone diagnostic CT scanning during their assessment. These CT images can also be used to plan the procedure11 by defining the optimal angiographic view and may be used to assess the importance of a side branch.
ASSESSING THE IMPORTANCE OF THE SB
There has been considerable historical debate about how to assess the relative importance of a side branch. This debate arises from an element of inevitable uncertainty about the likely consequences of SB occlusion. Although very minor elevations of troponin might be safely ignored, it is clear that higher levels of troponin elevation are clinically relevant, especially when accompanied by symptoms and evidence of new infarction on myocardial imaging12,13. Data using CT angiography and fractional flow reserve (FFR) confirm that an SB supplies less myocardium than the main branch (MB) and that stenosis of the SB is less likely to cause relevant ischaemia than a similar stenosis of the MB14. Notably, those SBs with length measured by CT >73 mm were most likely to supply at least 10% of fractional myocardial mass. Interestingly in this analysis, the first diagonal branch (but not the second) and the obtuse marginal branches of the LCx commonly supplied substantial amounts of myocardium. Consequently, the length of the SB together with the degree of stenosis and the length of stenosis define an important/complex SB lesion which must always be protected during the revascularisation procedure. An elective decision to use two stents preferentially in these important side branches with complex/extensive stenoses (>5 mm disease extending into the SB) is more likely, especially when it is challenging to wire both branches.
WIRING THE LESION
In elective patients with chest pain and a bifurcation lesion, physiological assessment using either a hyperaemic or non-hyperaemic index should be considered routinely prior to intervention. However, initial pressure wire assessment before MB balloon dilation cannot reliably predict whether a second stent in the SB will be required after MB stenting. The EBC recommends the “jailing wire” technique which consists in leaving a wire in the SB while implanting a stent in the MB. This has the following potential advantages: 1) the technique may help to keep the SB open and, in case of occlusion, the guidewire marks the SB position; 2) it facilitates access to the SB by favourably changing the angle of the bifurcation; 3) the jailed wire is a modality of anchoring that facilitates the intubation of the guiding catheter, providing a firmer support for the balloon to cross the origin of the SB; and 4) in extreme situations, the jailed wire can be used as a rescue procedure, to pass a low-profile balloon and dilate the SB to regain some flow15.
Ideally, the most difficult lesion/branch should be wired first in order to avoid wire wrap. Avoid pushing the MB wire too distally to maintain the shape of the wire tip which will be used to wire the SB through the MB stent and reduce the risk of distal dissection/perforation. When SB wiring access is difficult, plaque modification with rotablation16 or occasionally balloon dilatation may facilitate passage of a wire prior to stenting.
Removing a jailed wire from an SB can cause the guide catheter to dive antegradely into the coronary artery. Consequently, a slow controlled withdrawal pressure on the wire is advised with preventative guide catheter traction. The risk of complications during trapped wire removal can be reduced in calcified vessels by minimising the length of the trapped wire behind the stent and lowering post-dilation pressures. Once the SB wire has been relocated through rather than behind the stent, further post-dilation can be safely performed. Both polymer-coated and non-polymer-coated wires can be safely jailed behind stents.
PREDILATION
After wiring both branches the MB is identified. Predilation of the MB facilitates the bifurcation procedure and allows planning with regard to the length of stent required to facilitate a safe POT dilation, proximal to the bifurcation. Notably, this ensures optimal stent expansion within the MB, as it is the MB status which influences the long-term outcomes following bifurcation stenting. Routine SB predilation is not recommended unless either SB access is difficult, or there are severe diffuse and/or calcified SB lesions or when flow is compromised after wiring.
MAIN BRANCH STENTING
Drug-eluting stents (DES) are recommended. Selection of the most appropriate stent platform should be made according to the expansion ability of the stent, in order to allow optimal stent apposition proximally before the bifurcation lesion and at the SB ostium. The maximal cell diameter of the stent to be placed over the SB ostium is also an important consideration for bifurcations in large vessels such as the left main (LM)17. Stent diameter for the MB stenting is selected according to the size of the MB beyond the bifurcation as this reduces the risk of SB occlusion caused by carina shift and dissection within the distal segment if the stent diameter is too large. When using this distal sizing strategy, a final POT is essential to ensure optimal stent expansion.
PROXIMAL OPTIMISATION TECHNIQUE (POT)
POT should be performed routinely during the bifurcation procedure as it optimises stent deployment/apposition and restores the fractal geometry of the vessels8. It should be performed before SB rewiring as it facilitates access towards the SB, by reducing the possibility that the wire might cross into the SB behind the MB stent, and it may also facilitate crossing into a distal cell within the MB stent. POT may be repeated when the wire cannot recross into the SB.
POT involves inflating a short appropriately sized balloon just proximal to the carina. Consequently, this extra 6 to 10 mm (the smallest length of commonly available balloons) needs to be considered when choosing the proposed MB stent length. The diameter ratio between the balloon and the proximal MB reference segment should be 1/1 and a non-compliant balloon should be used18. Careful positioning of the balloon for POT is crucial as, if it is too distal, it increases the risk of SB occlusion (caused by carina shift) and, if it is too proximal, it has no effect on pushing the stent strut towards the SB ostium. Importantly, the distal shoulder of the balloon should be positioned just proximal to the carina while the proximal balloon is still completely within the stent in order to avoid inadvertent proximal vessel injury.
Technical challenges of POT include ensuring the accurate position of the balloon within the 3D geometry of the bifurcation; this may take several radiographic views to achieve. A number of stent enhancement techniques are available on radiographic equipment. These sequences may have a particular role during placement of the POT balloon. Also, positioning of the distal marker compared to the distal shoulder of the balloon may vary between manufacturers. Recent unpublished bench data have augmented previous awareness of the hazards of distal POT and its potential to cause SB distortion19. Notably, when the balloon does not span the entire stented proximal MB stent segment, the balloon should be repositioned and re-inflated to ensure that the most proximal part of the stent is also sufficiently expanded.
SB TREATMENT – OPENING
The fundamental advantage of the provisional approach is that SB treatment remains an alternative at any stage throughout the procedure. Opening the distal stent strut (close to the carina) of the MB stent towards the SB improves ostial SB scaffolding and decreases the need for a second stent. In order to increase the odds of crossing the distal strut, the recommended technique is to have a perpendicular view of the SB ostium and to pull back the MB wire (or a third wire in the same direction). If there is any doubt or if a balloon will not cross, the jailed SB wire can be removed, and a further attempt can be made. The position of the wire cross and its position relative to the stent can be accurately assessed by OCT. Use of non-compliant (NC)18 balloons is recommended as they are associated with a lower risk of SB dissection and consequently there is less requirement for an SB stent.
When the SB is small, a “keep it open strategy” is usually the best approach, starting by wiring both branches, stenting the MB followed by POT. Unless flow is reduced within the SB further treatment is unnecessary. In small SBs with reduced flow, rewiring through the stent struts, with SB dilation and further final POT, should be initially considered. Even when kissing balloon inflations (KBIs) are performed, a further final POT inflation is still recommended to minimise eccentricity index20 and optimise a round MB lumen (KBI can result in an oval MB luminal contour). The decision to place a second stent is based on the size of the vessel and the quality of the achieved result. However, ensuring an optimal result in the MB should be given priority over optimising the appearance in the SB if there is a need for a preference.
When the SB is substantial, both branches should always have been wired before dilation. Stent implantation in the MB and POT should be performed in sequence. At the 14th consensus meeting, POT/side/POT or a POT/kiss/POT approach was debated. Preference was confirmed for the POT/kiss/POT strategy as it was less likely to cause problematic stent deformation when performed in a “real-world setting”, although clinical verification of this is still awaited.
SB TREATMENT – STENTING
Use of a second stent may be needed in 10% of cases treated with a provisional approach. The second stent is indicated when the angiographic result is clearly suboptimal and, particularly when flow remains reduced, subsequent SB stenting can be performed using either T or T and protrusion (TAP) or culotte. The choice of T vs. TAP can be informed by careful imaging with stent enhancement to see whether there is MB stent malapposition opposite the SB on the opposite wall of the carina after KBI and POT (Figure 1). This is more likely after the MB stent has been crossed distally and the POT has been accurate. Under these circumstances T stenting can be considered. In most circumstances, accepting the creation of a small neocarina using the TAP technique is advised.
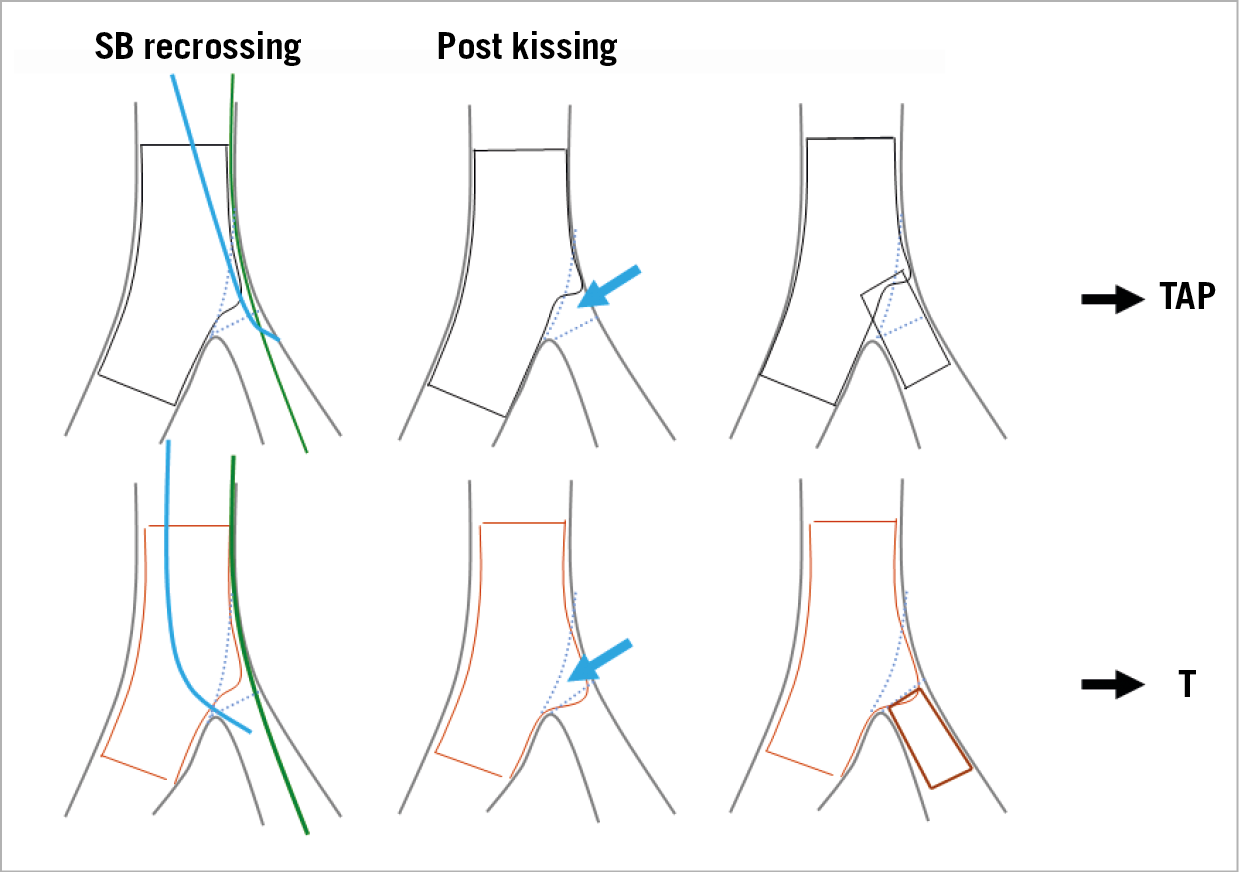
Figure 1. Assessing the result of the provisional approach (after kissing and POT). Either T or T with protrusion can be selected depending on the deformation of the stent in relation to the SB orifice.
Both T stenting and TAP should routinely be finalised with a KBI and a POT. Careful placement of the final POT balloon is essential in both techniques, but particular care is needed to avoid the neocarina following the TAP technique (to prevent crushing the protuberant SB stent).
Following MB stenting, focal ostial “pinching” with normal flow in both branches is quite common. Although it may be tempting to place a second stent under these circumstances, it is usually not necessary. Decision making can be facilitated by pressure wire placement in the SB; in the absence of an ischaemic measurement, a second stent to the SB is clearly unnecessary21. When the physiological index suggests borderline ischaemia, management is more controversial but kissing/ostial SB balloon dilation and further careful POT can be considered.
EBC recommendations on elective use of two-stent techniques in bifurcations
The elective treatment of bifurcation lesions with complex anatomy and diffuse atherosclerotic involvement of both the main vessel (MV) and the SB is more likely to require a two-stent approach. Two technical issues are critical in these patients: 1) lesion preparation before stenting, and 2) the procedure must involve KBI followed by final POT. Complete stent expansion facilitates optimal scaffolding and achieves the best acute vessel lumen gain. Malapposed or underexpanded stent struts can affect prognosis by triggering both restenosis and/or stent thrombosis. Accordingly, accurate and extensive post-dilatation is required
Elective use of two stents is indicated in very complex lesions with calcified SB and/or ostial disease extending >5 mm from the carina and in bifurcations with a major SB whose access is particularly challenging. Operators have a wide range of theoretical treatment options well summarised by the updated and amended MADS classification (Figure 2, Figure 3). MADS (main/across/distal/side) is based on the final position of the stents in the bifurcation and the sequence in which stents are implanted according to a strategy reflecting both lesion and technique complexity. In this consensus, MADS has been amended to remove untested and unreliable techniques and to facilitate recording of technique in clinical databases. Both elective T stenting and simultaneous kissing stenting (SKS technique) are not recommended by the EBC due to the lack of predictable results in terms of stent distortion and vessel wall coverage and concerns regarding safety with the long, double-layer neocarina using SKS.
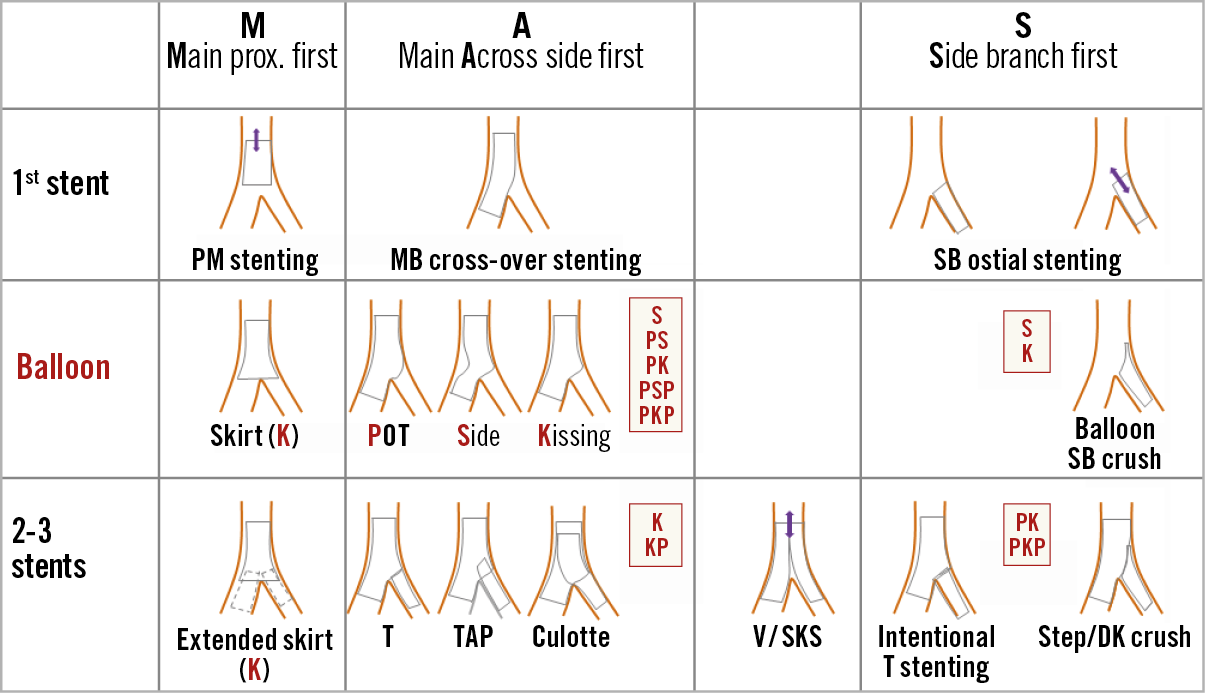
Figure 2. The new amended MADS (2019) classification. Four families are highlighted by letters selected to describe the position of the first implanted stent (or stents in the case of simultaneous deployment). The stent position is located according to the “3 segment” fractal geometric description of coronary bifurcations (proximal MV; distal MV; SB) . The family names are: M: first stent implanted in the proximal MV. A: first stent implanted in the MV across the SB take-off (this technique is “provisional”). D: first stent implanted in the MV distal to the SB take-off. S: first stent implanted in the SB. The V and SKS technique are included but not recommended by the EBC. Further detail of the new MADS classification is given in Figure 3.
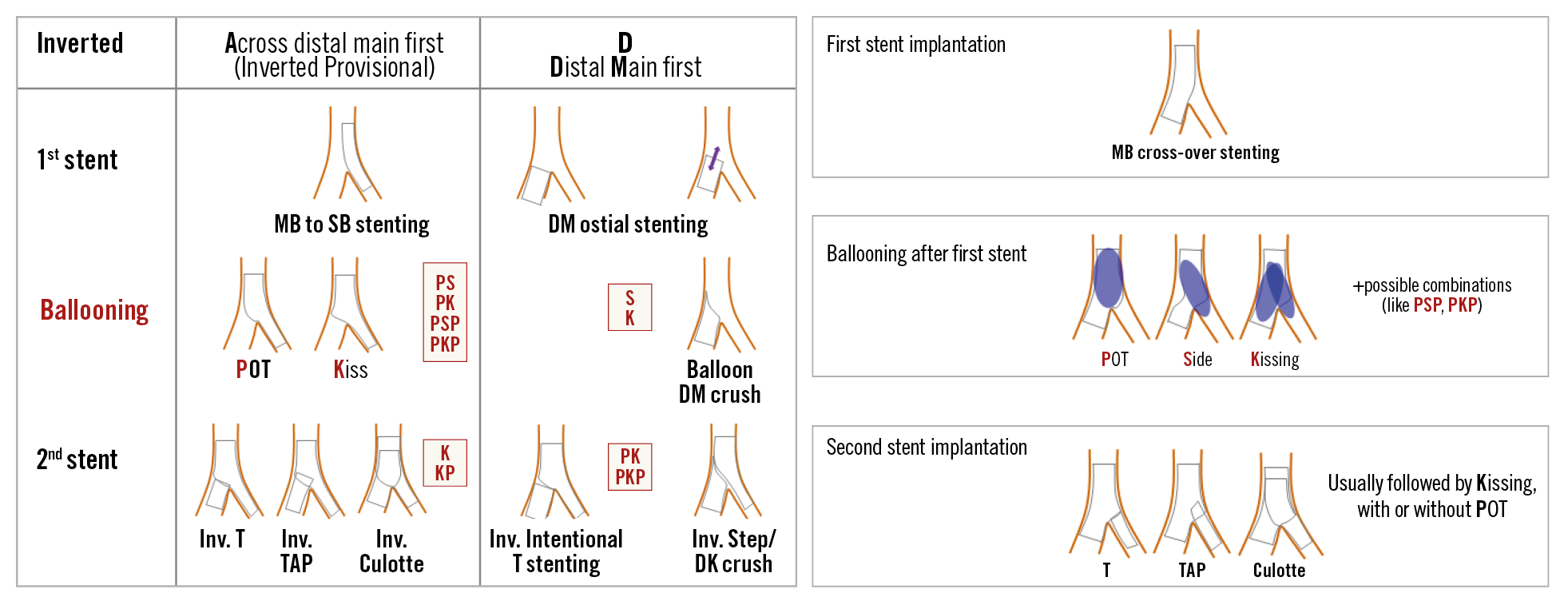
Figure 3. The new amended MADS (2019) classification. Three types of balloon dilation techniques are considered pivotal during bifurcation treatment. These have been inserted in MADS-2 using a single letter ballooning technique code: P = post-dilation of the proximal main vessel (usually reported as proximal optimisation technique [POT]); S = balloon dilation of the SB ostium; K= balloon inflation in the MV and SB (usually reported as kissing balloon inflation technique). Combinations of the ballooning techniques can be highlighted by appropriately ordered letter sequences, e.g, PKP stands for POT, followed by kissing, followed by further POT. PSP represents POT, followed by side branch inflation, followed by final POT.
All two-stent techniques share the increased risk of stent thrombosis. Although this risk can be reduced by scrupulous technique including mandatory kissing inflations and performing final POT, patient adherence and compliance to dual antiplatelet therapy is crucial. Preliminary unpublished data from a bifurcation substudy of the GLOBAL LEADERS22 trial have added to existing data23, suggesting that prolonged prescription of the potent ADP antagonist ticagrelor may be useful in reducing clinical events following a two-stent technique.
Culotte vs. DK crush
The crush technique initially reported by Colombo has been modified by Chen and colleagues to the much more predictable DK-crush technique24. This modification requires the systematic performance of two KBIs but reduces the risk of failure to performing KBI. The results of DKCRUSH-V24 which compared DK crush with culotte were debated at the EBC meeting. It was noted that there was quite extensive side branch disease in the recruited patients (confirming the likely need for a two-stent approach, rather than provisional), that the principal difference was in repeat revascularisation rates and that perhaps operators in this study were probably more familiar with the DK crush than a culotte performed with three POT dilations.
The principal concerns about the DK crush remain that 1) it cannot be performed as a provisional approach (as the SB is stented and the proximal portion is crushed without the option for MB reassessment), and 2) many operators will only do a limited number of true bifurcations annually. As DK crush is a complex technique with additional procedural steps, this lack of familiarity may increase the potential for mistakes. However, it is clear that in expert hands it is an efficient technique especially for complex 1,1,1 left main lesions and 0,1,1 left main lesions with a large dominant diseased LCx. Notably, the recent EAPCI/EACTS revascularisation guidelines25 gave a IIb recommendation for the technique in true left main lesions compared to the provisional approach, meaning that its efficacy is less well established by evidence and that it “may be considered” as a treatment option. Recent refinements include POT after placement of the MV stent and a final POT after the second kissing inflation. Consequently, the EBC recommends that, when crush is to be performed, this modification of the classic DK crush is the preferred operative sequence.
Culotte stenting has been tested in several trials. One limitation of the technique is the need for the two stents to accommodate the potential diameter mismatch between SB and proximal MB. Optimal performance of the culotte technique involves three POT inflations to minimise the risk of wire passage behind stents and optimise the point of wire cross into the SB. Therefore, the opinion of the EBC is that, when a two-stent strategy is used, this will become apparent during a provisional stepwise approach to the lesion. Under these circumstances, finalising the procedure using a culotte technique or occasionally TAP is recommended.
Intracoronary imaging
Both IVUS and OCT may provide crucial information in planning and optimising treatment of a bifurcation. Angiographic evaluation is often limited in assessment of the SB ostium, overlapping stent segments, lesion coverage, wire positions, stent expansion and strut apposition. When imaging is performed, careful monitoring of procedural anticoagulation is essential as procedural time can be increased. Recent publications from the EBC have highlighted the use of either IVUS or OCT in bifurcation treatment2,3.
Compared to IVUS, OCT provides superior images of the lumen surface, calcified plaques, predilatation results, stent positions, wire positions and the SB ostium from both MB and SB pullbacks. IVUS allows better characterisation of plaque burden and does not require vessel flushing or additional contrast during acquisition. The main focus points for guiding bifurcation stenting using intravascular imaging are:
BEFORE STENT IMPLANTATION
− Lesions proximal or distal to the SB and ostial stenosis have been shown to affect the likelihood of SB compromise after MB stenting
− Planning of stent length including planning size and length of balloon for POT
− Assessment of segmental stent diameters based on proximal and distal reference size estimations.
POST INITIAL STENTING
− Rule out residual edge stenosis and dissection
− Evaluate stent expansion and apposition
− Verify wire position in SB recrossing and rule out accidental abluminal rewiring especially in two-stent techniques (evaluation after each rewiring can be considered).
AFTER POST-DILATION
− Final scan after KBI to evaluate the SB ostium. When an SB stent has been implanted, it is recommended then to scan the stented SB and evaluate stent expansion and apposition.
Quantitative coronary analysis (QCA) – dedicated QCA systems for bifurcations
QCA is an important standard analysis in scientific reporting and for regulatory assessment. Present 3D QCA systems further provide the optimal projection angle in bifurcations and in some systems form the backbone for co-registration to OCT and IVUS. A dedicated synopsis of the use of QCA in bifurcation lesions has been prepared by the EBC4.
The left main
Recent guidelines on myocardial revascularisation from the European Society of Cardiology/European Association for Cardio-Thoracic Surgery25 give a class 1 indication for percutaneous coronary intervention (PCI) in patients with significant LM disease and a low/intermediate SYNTAX score. PCI in patients with significant LM disease with a SYNTAX score ≥33 is given a class III recommendation. PCI in the LM should always be regarded as a challenging procedure. Operators and their teams need to be experienced and proficient in responding rapidly to a sudden unplanned deterioration and the requirement for bail-out stenting strategies.
A recent EBC consensus has summarised the differences between the LM and other bifurcations1.
These include the following:
− The SB is usually the Cx which most often has a large reference diameter and is angulated making it difficult to access with guidewires. Acute occlusion of the LCx usually results in considerable ischaemia. The T-shaped, bifurcation angle of the left main stem (LMS) may also affect implantation technique, and a highly angulated LCx take-off may impact on prognosis after LM stenting.
− The LM is the only bifurcation where the proximal MB originates directly from the aorta. This increases complexity because of the interaction with the guide catheter and the potential for guidewires to go behind LM stent struts.
− Longitudinal compression during left main stenting is common and when untreated is associated with an adverse outcome.
− The proximal reference diameter may reach 6 mm – which is close to the dilatation limit of many coronary stents. Careful reference to manufacturers’ guidelines is recommended14.
− Left main trifurcations are encountered in about 10% of LM cases and require specific treatment strategies.
A provisional SB stenting approach is recommended for LM treatment in most cases. However, there are occasions where a two-stent strategy is required from the outset of the LM procedure. Coronary calcification is especially common, and the presence of calcium means that adjunctive plaque modification may be required to facilitate optimal stent implantation. When plaque modification is felt to be unnecessary, either invasive imaging or careful predilation with an appropriately large (ideally non-compliant) balloon is recommended to ensure that subsequent stent expansion is possible. Initial wiring of the SB is recommended, and a careful single-stent approach with POT is particularly applicable because of the changes in vessel calibre proximal and distal to the LM bifurcation. Appropriate POT will reduce malapposition which is common in the LM and this may also reduce longitudinal shortening26.
EBC MAIN is a prospective, multinational, randomised clinical study of LM stem true bifurcation lesions (type 1,1,1 or 0,1,1: both left anterior descending and LCx artery >2.75 mm diameter) promoted by the EBC group. The study hypothesis is that LM coronary bifurcation lesions are best treated with a planned single-stent strategy rather than a planned dual stent strategy, with respect to death, target lesion revascularisation and myocardial infarction at one year. Study enrolment will be completed in 2019.
USE OF OCT AND IVUS IN LM
Angiographic assessment of the LM has several limitations; this mandates a low threshold for use of IVUS or OCT. Imaging may influence lesion preparation in particular, as detection of confluent arcs of calcium will usually require use of adjunctive technology rather than just conventional balloon predilation. Stent malapposition, distortion of stents during rewiring and guide/guide catheter extension device manipulations in the LM as well as stent undersizing contribute to the long-term risk of stent thrombosis which in the LM is potentially catastrophic. Unpublished insights from the EXCEL trial were discussed at EBC 14. These highlighted the adverse impact of uncorrected longitudinal stent distortion on clinical outcomes. Consequently, systematic imaging and remedial actions informed by the imaging are recommended by the EBC during and especially after elective LM stenting.
Conclusion
This document from the 14th EBC meeting represents highlights of the current consensus and clinical recommendations of the EBC. Particular emphasis has been placed on a careful and sequential approach to bifurcation stenting using the provisional strategy. Whilst the decision on which technique to use in an individual lesion remains specific to the operator and the lesion, the EBC believes that most bifurcations are best treated in this way rather than committing to a complex two-stent approach at the initiation of the procedure. Much has already been learned, but the EBC aims to continue to develop its approach, embracing new technology with the aim of improving outcomes for our patients with bifurcation lesions.
Funding
A. Banning is partially funded by the NHS NIHR Oxford Biomedical Research Centre.
Conflict of interest statement
F. Burzotta reports receiving honoraria from Abiomed, Medtronic and Abbott. A. Banning reports receiving honoraria from Abbott, Boston Scientific and Volcano. The other authors have no conflicts of interest to declare.