In the current issue of EuroIntervention, authors from the Asia Pacific (APAC) region present a consensus document on the management of coronary bifurcation lesions within their respective countries/geography1.
The publication is intended to supplement previous publications on the same topic from the European Bifurcation Club (EBC) and provide additional insights relevant to local challenges for health care, clinical practice and progress in medical knowledge. This publication follows recent EBC publications2,3,4, the joint ESC/EACTS Guidelines on revascularisation published in 20185 and most recently the DEFINITION II trial6. When reading this particular consensus statement, one is forced to consider and perhaps challenge the relative roles of “consensus statements” and guidelines in our clinical practice.
The Oxford English Dictionary defines consensus as “an agreement in opinion, the collective unanimous view of a number of persons”. Alternatively, a guideline is defined as “a general rule or principle or piece of advice”. It is designed to streamline a process according to a set of principles or sound policies and it is issued to “make actions more predictable and of higher quality”. By definition, neither a consensus statement nor a guideline need be followed in mandatory fashion.
For clinicians, considering these different dictionary definitions is probably valuable. The ESC has a clear process by which data may be considered for inclusion within a guideline. A randomised controlled trial is the highest level of evidence and multiple randomised controlled trials on a single clinical question will result in strong guideline support and an evidence rating of 1A. Inevitably, many questions and practices in medicine have never been subject to randomised trial either because they are historically accepted or because they are new and yet to be proven. Within guidelines, these historically accepted statements are usually rated 1C. In contrast, consensus statements have a less clear structure and a less prescribed membership and process. Presumably, therefore, their role is to collate expert opinion in areas where randomised trials have generally not been performed and provide a commonsense framework of opinion for practising clinicians which they can use on a day-to-day basis.
The field of bifurcation intervention remains challenging and, to a certain extent, controversial. It is clear that, just as no two patients are the same, no two bifurcations are the same – even within the same patient. Consequently, applying a blanket guideline approach to the practical interventional approach to a bifurcation is not likely to be appropriate. The consensus generated for the APAC area1 covers a diverse range of countries with clearly divergent socio-economic status. Authors from Australia, Singapore, Korea, New Zealand, China, Malaysia, India and Japan together with colleagues from Europe reflect on how societal attitudes towards cardiac surgery and the availability of medical therapy might impact upon local revascularisation strategies. Importantly, they conclude that, despite previous speculation, patients with Asian descent have a similar (size matched) calibre of major epicardial coronary artery to the European/US populations. Consequently, they recommend that the fundamentals of bifurcation PCI in the APAC territory be regarded as similar to the rest of the world. Particular emphasis within the consensus is given to the radial approach, and insights and tips are given concerning the jailed balloon and the modified jailed balloon techniques.
Since its inception, the EBC has recommended a provisional stenting approach to most bifurcation lesions2. Using this approach, it is felt that operators can minimise risk, optimise outcome and be cost-effective. The addition of the proximal optimisation technique (POT) to ensure main branch (proximal) stent apposition has been a fundamental evolution in strategy and is applicable to almost all bifurcation treatments. Together with the recent ESC Guidelines5, the APAC consensus endorses this approach.
Deciding which coronary bifurcation lesions require an elective two-stent approach remains a fundamental discussion point together with the role of the double kiss (DK) crush technique7. Controversy persists about how one can truly identify a bifurcation lesion which is likely to have a prognostic implication for a patient and the relative importance of elevation of cardiac enzymes during interventional procedures8,9. In the APAC statement, a number of risk prediction models are referenced. Ultimately, an elective two-stent strategy is recommended “when the side branch is clinically relevant with a functionally significant stenosis and it is prognostically important”. The DK crush technique can be considered, although the familiarity of the physician with the technique should be taken into consideration.
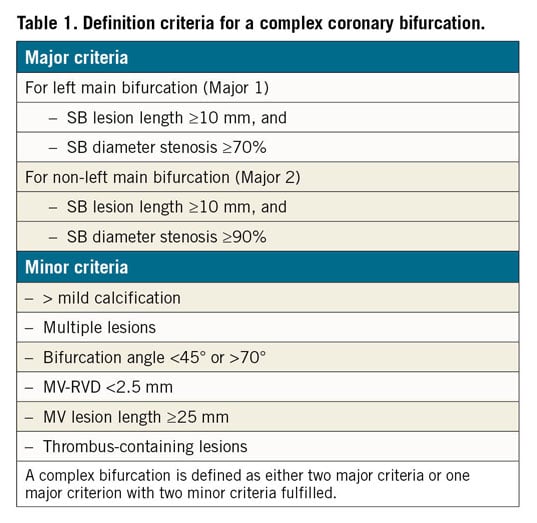
In the last few weeks, the DEFINITION II trial has been published in the European Heart Journal6. Patients were considered for inclusion if they fulfilled the DEFINITION criteria for a complex bifurcation lesion (Table 1). This study included 660 patients with Medina 1,1,1 or 0,1,1 bifurcation lesions undergoing revascularisation. Bifurcation lesions were randomised to either a provisional approach or an elective two-stent approach. Around 80% of the patients in the two-stent group had a DK crush procedure, although not all. The primary endpoint was target lesion failure (TLF) at one year, comprising cardiac death, target vessel myocardial infarction (MI) or target vessel revascularisation. The definition of procedural MI (within 48 hours) was a stringent one as it required elevation of creatine kinase myocardial band (CK-MB) >10x the upper limit or 5x elevation plus either 1) new Q-waves or left bundle branch block (LBBB), 2) new angiographic stenosis or occlusion, 3) imaging evidence of myocardial damage, or 4) new regional wall motion abnormality.
The trial demonstrated a significant reduction in TLF, 11.4% with the provisional versus 6.1% using the two-stent approach. This difference was largely attributable to the higher periprocedural MI rate seen with the provisional approach. Notably, both procedural approaches appear to have been very carefully performed and almost all of the side branches in the provisional group that occluded during the procedure were eventually opened successfully. The high rates of procedural MI within the provisional approach group in this trial are noted but not explained within the paper.
Using a DK crush technique for complex bifurcation within the left main achieved a IIB recommendation in the recent ESC guideline and the technique is already endorsed for complex bifurcation therapy by the EBC. These new data from DEFINITION II are clearly important, but I think the most important lesson is for clinicians to read and understand the DEFINITION criteria for complex bifurcation. When we intend to treat this complex category of lesion within our clinical practice, we should recognise that this lesion is particularly problematic and we should carefully consider a two-stent approach in most cases. For example, in the DEFINITION II trial, 95% of patients had a side branch lesion length of >10 mm – with an average length of side branch lesion of 20 mm. Clearly these are side branch lesions which most operators would agree require stenting in their own right, and therefore a two-stent technique is usually required. However, it is important to recognise the extent to which this population differs from the patterns of bifurcation coronary artery disease observed in the European population.
Additional data on the merits of the provisional approach in left main bifurcation lesions will become available from the EBC MAIN trial10 next year. Subsequent discussion of summated trial data may allow generation of a more global guideline, although I suspect that achieving a modified consensus after extensive discussion may be our ultimate pragmatic goal.
Conflict of interest statement
A. Banning has received an institutional educational grant for a fellowship from Boston Scientific Corp. and speaker fees from Boston Scientific, Medtronic, Abbott Vascular, Philips/Volcano and Miracor.
Supplementary data
To read the full content of this article, please download the PDF.