Percutaneous coronary interventions (PCI) with the implantation of a drug-eluting stent (DES) for either bifurcation or non-bifurcation lesions are associated with a dramatic reduction of the need for revascularisation when compared to a bare metal stent implantation1,2. During the procedure, overdilation is frequently required to achieve full apposition, although there is no consensus with respect to the degree of extensive post-dilation in real-world international practice.
To this end, a timely bench-test study focusing on the impact of overdilation on stent maximal expansion capacity and deformation appears in this issue of EuroIntervention3. For lesions that are localised in either the left anterior descending artery (LAD) or the distal left main (LM) bifurcation, a diameter discrepancy in the proximal and distal vessel segment is one common reason leading to the use of overdilation with a larger, non-compliant (NC) balloon. However, several concerns have been raised regarding overdilation, namely the estimation of proximal vessel diameter, the maximal expansion capacity of the implanted stent, the methods of overdilation and finally complications caused by overdilation such as stent fracture, stent recoil and longitudinal compression.
Estimation of vessel diameter
Although intravascular ultrasound (IVUS) and optical coherence tomography(OCT) are two currently available accurate tools for the estimation of the vessel diameter, angiographic imaging is the most convenient one according to Murray’s law: Dmain=(Ddaughter–1+Ddaughter–2)×2/3. However, in the case of diffuse lesions without a normal reference segment, this formula has a limited ability to calculate accurately the main vessel diameter.
Maximal expansion capacity of implanted stents
Previous in vitro studies analysed the maximum stent expansion in one diameter segment following overdilation by a 5 mm NC balloon4-7. In this issue, Foin et al examine the differences in workhorse designs of six commercially available DES3. They report that minimal lumen diameter (MLD) of any type of the larger stents could be increased to >5.5 mm with a 6.0 mm NC balloon, and that maximum expansion capacity for each stent diameter was limited by its design. Knowledge of the cut-off diameter among the different existing stent designs is mandatory for everyday practice.
Methods of overdilation
Obviously, one limitation from previous studies, including the one by Foin et al, is that the kissing balloon inflation (KBI) was not tested in their models3-7. The working patterns of two balloons during kissing inflation affects the stent strain and distortion as well as the achievement of final MLD. In Figure 1, two NC balloons wrapped around each other when the distal LM bifurcation angle was >70°, and two balloons used shoulder-to-shoulder were thought to be an appropriate pattern causing less vessel strain. With overdilation, stent cell size increased significantly3,4,6. If the configuration of the cell area is irregular, the shorter (smaller) diameter of the cell determines the maximum stent expansion during KBI. In Figure 2, a side branch balloon was completely inflated at an alternative stage and was “compromised” by the main balloon during KBI after employment of the classical crush stenting technique. This phenomenon has been termed as kissing unsatisfied (KUS), which was one critical factor predicting the occurrence of restenosis at ostial side branch in our DK-CRUSH serial studies.8 Moreover, for the one-stent technique, cell size could be predicted after overdilation, but it is somewhat difficult or impossible to predict cell size after a complex stenting technique is applied (Figure 3).
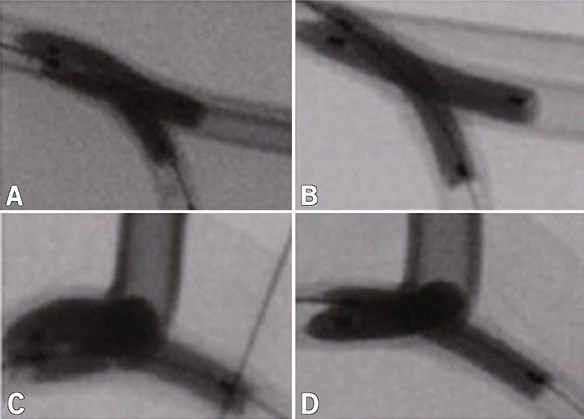
Figure 1. Patterns of two balloons during kissing inflation. For a type Y bifurcation angle (A, B), two short balloons are inflated at 8 atm parallel to each other (A); two long balloons became slightly wrapped together when inflated at high pressure (14 atm, B). For a type T bifurcation angle (C, D), two balloons wrapped together significantly.
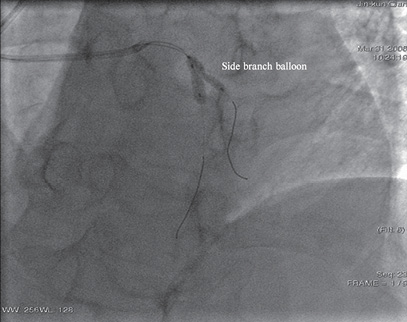
Figure 2. Kissing unsatisfied. During kissing balloon inflation, side branch balloon was compromised by the main vessel balloon.
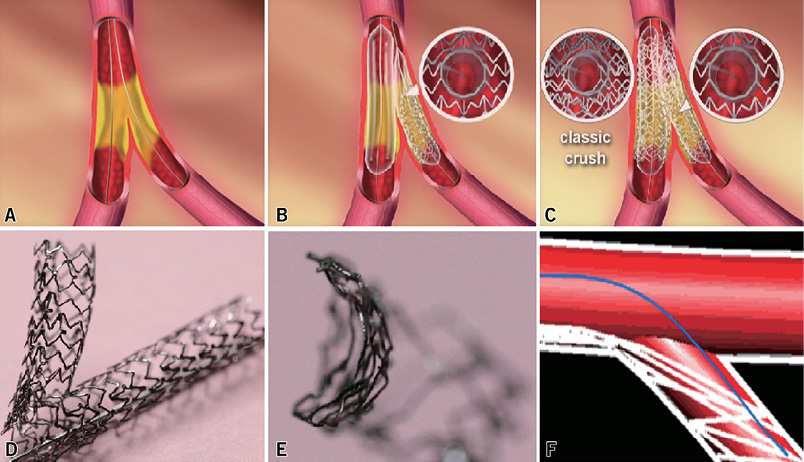
Figure 3. Comparison of cell openings. For a given bifurcation lesion (A) there is only one layer of stent struts around the orifice of the side branch (B), thus, cell size is easily opened. However, the presence of three layers of struts at the level of the ostial side branch limits the full opening of these cells (C). In fact, the selection of the right cell for opening is very difficult (D) and, because of the large gap between side stent and vessel wall, devices (such as wires and balloons) are apt to jump into this gap and then pass into the true lumen of the side stent (D, E, F).
Complications caused by overdilation
As IVUS has shown that plaque prolapse was commonly observed after deployment of a DES with open cell design, overdilation will significantly enlarge cell size resulting in a potential increase in the risk of plaque prolapse, although the influence of severe plaque prolapse on long-term outcomes is still unknown. However, an overly incremental increase of cell size raises concerns regarding the drug distribution in the vessel wall3,5. Thus, further studies to elucidate the effective area of drug distribution before and after overdilation are critical.
Another complication is the damage or erosion of the polymer caused by overdilation. Using scanning electron microscopic assessment, Basalus et al reported the presence of coating irregularities of the first generation of DES in an unexpanded state4. Theoretically, overdilation causes extensive damage of the polymer coating leading to the risk of delayed healing and stent thrombosis. The remaining questions concern how much the overdilation cut-off values (pressure and diameter) will destroy the integrity of a polymer coating. To address this issue, additional research is required.
Overdilation induces severe vessel injury via direct (the stent being buried in the intima) and indirect (vessel strain, stent deformation) mechanisms and carries the high risk of stent damage. In Figure 4, shear stress at the proximal segment was maintained at acceptable levels immediately after stent deployment with 14 atm, which was further decreased to a much lower level after overdilation by KBI with two large NC balloons. While stent struts buried deeply in the intimal layer was good for the reduction of shear stress resulting from complete apposition, the direct vessel injury coupled with the damage to the polymer coating along with worsening drug distribution or edge dissection will put patients at a high risk of restenosis.
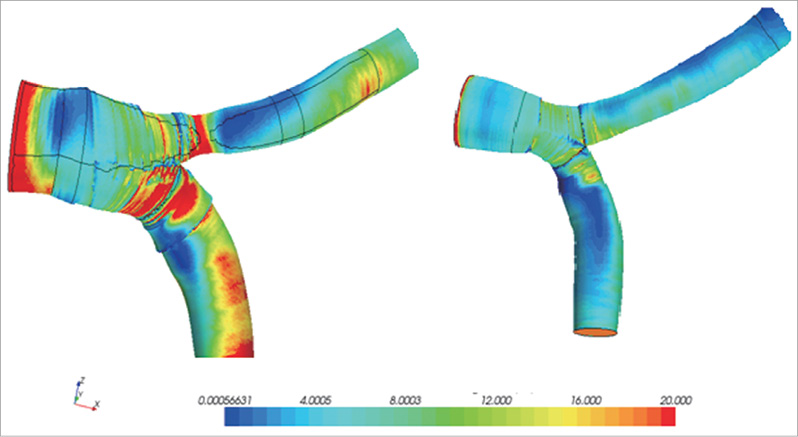
Figure 4. Redistribution of shear stress. Immediately after kissing balloon inflation (KBI) at 14 atm, higher shear stress was seen at the proximal edge and carina level, compared to lower shear stress at the lateral daughter vessel (left); after KBI at a higher pressure, previous high shear stress disappeared (right).
Stent fracture, stent recoil and longitudinal compression
The incidence of stent fracture is reported to be around 0.8% to >8%. Stent fractures in clinical settings have been reported to be frequently seen in ostial location and lesions with hinge motion, calcification or severe tortuosity, especially when a closed cell design stent was used. In fact, Kuramitsu et al demonstrated that stent fracture (2.9%) was not rare, even in second-generation DES9. Although in the current second-generation DES strut thickness is decreased significantly, overdilation can easily create stent deformation and stent fracture and both are potentially contributive to an increase in adverse clinical events.
Indeed, stent recoil is commonly seen in the contemporary DES era. Direct evidence shows that the in-stent MLD after deployment at the manufacturer’s recommended inflation pressure is below the expected diameter, with segmented or extensive underexpansion. This may explain why overdilation is performed by many interventionalists. Working with a flexible metal tube and concentrating on one aspect of deployment while losing another is unavoidable –full expansion and good apposition are obtained, but with the possibility of recoil and longitudinal compression. In Figure 5, longitudinal compression resulted in a large gap between two stents. This illustrates the need for a better understanding (as addressed in this issue) and careful selection of stent designs and positioning which are crucial in order to minimise the geographic loss.
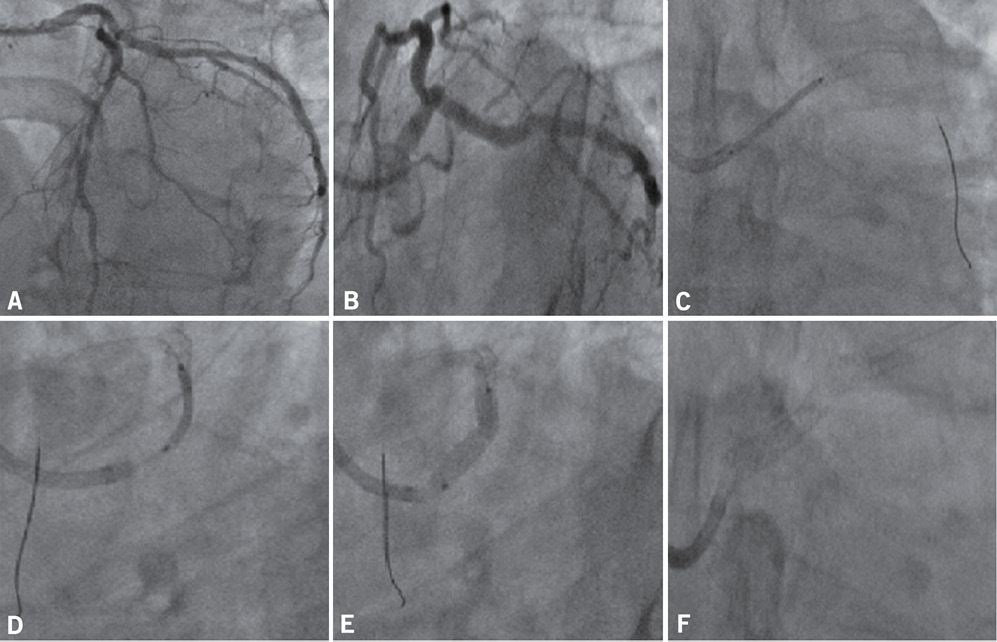
Figure 5. Longitudinal compression. A 52-year-old man had acute anterior wall myocardial infarction. In a local hospital, two drug-eluting stents were implanted in the left anterior descending (LAD) artery and left circumflex, respectively. Six months later, the patient presented with unstable angina. Angiography showed a critical stenosis from left main to LAD (A). A spider-view showed the overlapping of vessels (B). A 4.0×20 mm Promus Element™ stent was placed in position (C) and overlapped with the previous LAD stent (C, D, E). Stent boost demonstrated a gap between the two stents (F), as confirmed by intravascular ultrasound (image not included).
Further complexities of overdilation after double stenting for bifurcation lesions
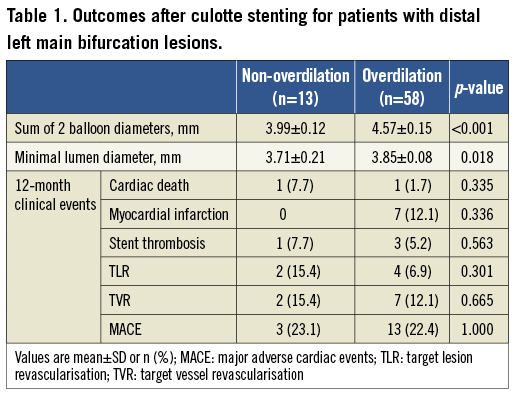
KBI was reported to be associated with improved clinical outcomes after complex stenting approaches. Unfortunately, there are no data with respect to the different incidents of MACE between “with overdilation” vs. “without overdilation”. In Table 1, 71 patients with distal LM bifurcation lesions were treated by the culotte stenting technique. Of these, overdilation (defined as the difference in balloon and vessel diameter >0.75 mm) was performed in 58 (81.7%) patients. The mean diameter of the stent selected was comparable between the two groups (3.5 mm). The expected stent diameter (calculated from two balloons) was 3.99 mm in the non-overdilation group, compared to 4.57 mm in the overdilation group (p<0.001). After KBI by two NC balloons at 16 atm, the final MLD by QCA was 3.85 mm in the overdilation group, significantly higher than 3.71 mm in the non-overdilation group (p=0.046). Importantly, the myocardial infarction rate in the overdilation group was high when compared to the non-overdilation group at 12-month follow-up (12.1% vs. 0.0%, p=0.336), while the target lesion revascularisation rate was low (6.9% vs. 15.4%, p=0.301), although there was no significant difference between the two groups. One may postulate that this difference in clinical outcome would be greater if the sample size increased substantially.
Finally, the correlation of overdilation or post-dilation with the dynamic change of FFR is another issue which needs to be addressed in the future. What should be kept in mind is that the rate of FFR>0.90 post-DES with appropriate post-dilation, as showed by DKCRUSH-IV study, is only achieved in 40% of patients with bifurcation lesions treated by provisional stenting10. Therefore, the cut-off values of inflation pressure, NC balloon diameter and use of invasive imaging tools are three critical parameters potentially influencing the clinical results.

