Abstract
Aims: The long-term impact of treating bifurcation lesions on the overall outcome of patients with multivessel coronary disease treated percutaneously with drug-eluting stents is unknown. This analysis determined the influence of bifurcation treatment using sirolimus-eluting stents on 3-year clinical outcomes.
Methods and results: Of the 607 patients (2,160 lesions) in the ARTS II study, 324 patients underwent revascularisation procedures involving treatment of at least one bifurcation (465 lesions). Three-year outcomes were compared to those without bifurcations. Despite more diffuse and complex disease in the bifurcation group, survival free of adverse events was equivalent in the two groups. At 3-years, there was no difference in rate of overall MACCE (20.2% vs. 18.5%, p=NS) or any of the component events between the bifurcation and the non-bifurcation group. There was a trend for a higher rate of definite stent thrombosis in the bifurcation group (4.6 vs 2.1%, p=0.1), but in multivariate analysis the CK value post-procedure served as the only independent predictor of definite stent thrombosis (p=0.015), with the presence of a bifurcation lesion of borderline significance (p=0.056).
Conclusions: In multivessel disease treated by PCI with DES, the presence of bifurcation disease had no adverse influence on 3-year clinical outcomes.
Introduction
In the drug eluting stent (DES) era, randomised trials are re-addressing the comparison between outcomes of percutaneous and surgical revascularisation for patients with multivessel coronary disease1,2. Should treatments be deemed equivalent, the presence of one or more bifurcation lesions may continue to influence the decision making process in favour of bypass surgery. When percutaneous coronary intervention (PCI) involves a bifurcation lesion, procedure times are longer and contrast volumes and radiation exposure greater. Moreover, to date, immediate and long-term success rates have been inferior to those observed in the treatment of simple discrete lesions3-8.
Our earlier substudy of the Arterial Revascularisation Therapies Study, part II (ARTS II) specifically addressed this issue by examining the practical impact of bifurcation treatment in patients with multivessel disease treated with sirolimus-eluting stents9. At 30-days and one-year, event-free survival was high for patients in whom a bifurcation was treated and equivalent to patients with multivessel intervention not involving a bifurcation. With the recent concerns regarding long-term safety of DES and the potential increase in late stent thrombosis, longer follow-up data in patients treated for bifurcation lesions with DES is required. Patients enrolled in ARTS II have now been followed for three years, and the outcomes presented in this analysis focus specifically on whether or not bifurcation treatment with DES increases the risk of late adverse events or repeat revascularisation.
Methods
Patient population
A total of 607 patients with multivessel disease (2,160 lesions) were included in the ARTS II study. Principal inclusion and exclusion criteria and recruitment procedures have already been described9,10. In brief, patients had stable or unstable angina or silent myocardial ischaemia and needed treatment of the left anterior descending (LAD) artery and at least one other significant lesion (>50% diameter stenosis by visual estimate) in another major epicardial coronary artery. Patients with any previous coronary intervention, left main coronary disease, overt congestive heart failure or a left ventricular ejection fraction of less than 30% were excluded. All 607 patients gave written informed consent. Of these patients, 602 were treated with PCI and the remaining five underwent bypass surgery.
Bifurcation subgroup
For the purpose of this analysis, bifurcation lesions were defined as a ≥ 50% diameter stenosis involving a main branch (MB) and/or contiguous side branch (SB) with a diameter ≥2.0 mm by visual estimate. A side branch was required to be within a distance from the lesion of less than three times the SB reference vessel diameter, measured from the branching point. Both the MB and the SB needed to have at least a Thrombolysis in Myocardial Infarction (TIMI) flow grade 1 preprocedure.
“True” bifurcation lesions were defined as lesions with significant stenoses located in both the MB and the ostium of the SB. “Partial” bifurcation lesions were defined as lesions in which a branching vessel did not have significant ostial stenosis. Lesions were further classified according to the SYNTAX Score bifurcation definition A–G11.
Just over half of all patients, 324 with 465 bifurcation lesions, met the criteria for inclusion in this analysis (210 patients with 1 bifurcation lesion; 114 patients with two or more bifurcation lesions) and were compared with the remaining 283 patients without bifurcations. Two additional subgroups were examined based on lesion morphology and stenting strategy: 1) Two-hundred (200) patients with at least one “true” bifurcation were compared with 124 that had only “partial” bifurcations, and 2) Two-hundred sixty-three (263) patients treated with a single stent strategy only were compared with 61 treated by 2-stent strategy (stent implantation in both branches) in at least one bifurcation (Figure 1).
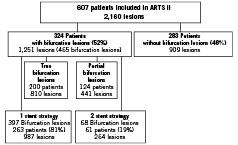
Figure 1. Patients with bifurcation lesions enrolled in the ARTS II study with sub-grouping according to bifurcation lesion type and stenting strategy employed.
Procedures
All lesions were treated with SES (Cypher®; Cordis Corp., Johnson & Johnson, Warren, NJ, USA) with a diameter of 2.5-3.5 mm and a length between 13 and 33 mm. The total length of stents implanted in an overlapping manner was unrestricted. The bifurcation stenting strategy (T- or V-stenting, culotte or crush)12 and the use of one or two stents were left to the operators’ discretion.
It was recommended that patients receive aspirin indefinitely and clopidogrel for a minimum of two months, or six months in the presence of diabetes, or after treatment of a chronic total occlusion. The recommendations for antiplatelet therapy were not different after bifurcation treatment.
Angiographic analysis of bifurcation lesions
Angiographic analysis of bifurcation lesions and procedural strategies were conducted by the core laboratory. For each lesion plaque distribution was described on the basis of the SYNTAX score11 and the take-off angle of the SB was measured (as the internal angle between the distal MB and SB by in a non-foreshortened projection). For the procedure, the stenting strategy and the use of a final kissing balloon inflation were documented. In true bifurcations, the presence of significant residual SB stenosis (≥ 50% diameter) was recorded and in partial bifurcations, significant plaque shift (≥ 50% diameter stenosis in one of the ostia after stenting) was documented. Angiographic success was defined for each branch as the presence of TIMI 3 flow and < 50% residual luminal diameter stenosis by visual assessment.
Endpoints and clinical definitions
The primary endpoint of this analysis was freedom from any major adverse cardiac and cerebrovascular event (MACCE) at three years, comprising all-cause mortality, any cerebrovascular event, non-fatal myocardial infarction and any repeat revascularisation by PCI or surgery after the index procedure.
Serum CK and CK-MB isoenzyme concentrations were measured 6, 12, and 18 hours after the intervention. Within seven days after procedure, myocardial infarction was defined as documentation of new abnormal Q waves and either a serum CK or CK-MB isoenzyme rise above five times the upper limit of normal or a CK-MB to total CK ratio greater than 0.1. As of eight days after intervention, either abnormal Q-waves or enzymatic changes as described above, were sufficient for the diagnosis of MI.
Definite and probable stent thrombosis events were adjudicated according to the ARC criteria13. Stent thrombosis was categorised depending on the timing of occurrence into acute (peri-procedure), sub-acute (post-procedure to 30 days), late (30 days to one year), or very late (> 1 year).
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) and categorical variables as frequency (%). Patient demographics and procedural characteristics in the “bifurcation” group were compared to those in the “non-bifurcation” group using the Student’s t-test with chi squared or Fisher’s exact testing for categorical variables. Additional subgroup comparisons were performed between patients with “true” and “partial” bifurcations and between patients treated with a single versus 2-stent strategy. Kaplan-Meier analyses and survival rates between groups were compared using the log-rank test. A two-sided p value < 0.05 was considered statistically significant. Analyses were performed using SAS version 8.02 (SAS Institute, Inc., Cary, NC, USA). A specific analysis was performed for stent thrombosis (ST). Due to the low number of events it was decided to group the possible and probable ST’s into one class thus obtaining three classes: no ST, possible or probable ST, and definite ST. These data were analysed using logistic regression with cumulative logits as link function. A univariate test was performed to obtain all regressors with a P value of less than 0.15. These were combined in a multivariable analysis, which, of course broke down because of heavy over-parametrisation. However, the diagnostic messages allowed us to identify the variables that should be removed because of co-linearity problems. Further pruning of the model was required as the proportional odds assumption was violated.
Results
Baseline characteristics
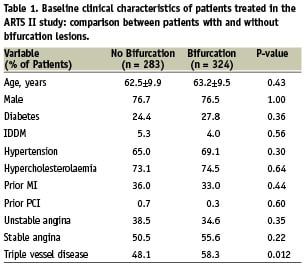
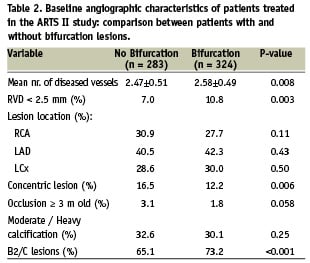
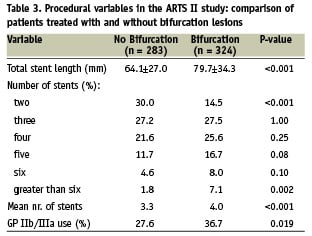
Patient demographics and the clinical manifestations of coronary artery disease were similar between the two groups (Table 1). The bifurcation group, however, had more extensive coronary artery disease (mean number of diseased vessels 2.58±0.49 vs 2.47±0.51, p=0.008) and more complex lesions (B2/C lesions 73.2% vs 65.1%, p<0.001) than the non-bifurcation group (Table 2). In agreement with these observations, procedural complexity in the bifurcation group was greater as reflected by longer total stent length per patient and a greater number of stents implanted (Table 3).
Three-year outcome in the bifurcation group versus the non-bifurcation group
At three years post procedure 79.8% patients with at least one bifurcation remained free from adverse events as compared to 81.5% of patients without a bifurcation (relative risk [95% CI] = 1.09 [0.79, 1.52; P=0.61) (Figure 2). When the individual components of the primary endpoint were compared, at 3 years there were no significant differences in outcomes between the two groups (mortality 2.8 vs 3.2% p=0.81; CVA 3.1 vs 2.5% p=0.81; QWMI 3.1 vs 1.1 p=0.10; NQWMI 2.2 vs 1.1 p=0.35, any repeat revascularisation 15.4 vs 13.1% p=0.42). Nor were there any differences when true and partial bifurcations were considered separately (Figure 3). Neither the occurrence of the primary endpoint nor the need for repeat revascularisation depended on whether a one- or two-stent strategy was used (Figure 4).
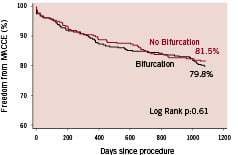
Figure 2. Kaplan Meier survival curves illustrating freedom from MACCE (major adverse cardiac and cerebrovascular events) in 324 patients treated for multivessel disease including bifurcation treatment (bifurcation) and 283 patients treated for multivessel disease with no bifurcation treatment (no bifurcation).
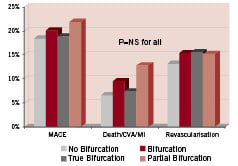
Figure 3. Occurrence of MACCE (major adverse cardiac and cerebrovascular events) by 3-years following multivessel angioplasty in 324 patients with and 283 patients without bifurcation lesions and in the subgroups of 200 patients with ‘true’ bifurcations and 124 patients with ‘partial’ bifurcation lesions.
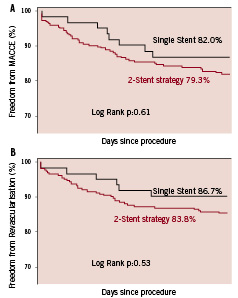
Figure 4. Kaplan Meier survival curves illustrating freedom from MACCE (major adverse cardiac and cerebrovascular events) in 263 patients treated for multivessel disease including treatment of a bifurcation using only a single stent strategy and 61 patients in whom at least one bifurcation was treated using a 2-stent strategy.
Incidence of stent thrombosis
Over the 3-year period, definite stent thrombosis (ST) occurred in 4.6% patients in the bifurcation group, and in 2.1% patients in the non-bifurcation group (p=0.12). The combination of definite and probable ST according to ARC criteria occurred more commonly in the bifurcation group (23/324 patients) than in the non-bifurcation group (9/283 patients), (7.1% vs 3.2% P=0.044) (Figure 5). More definite and probable ST occurred in the 2-stent strategy-group than in those treated with a single stent approach, but this difference was not statistically significant (11.5% vs 6.1%, p=0.16).
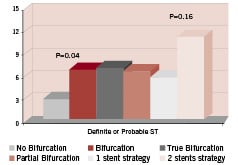
Figure 5. 3-year cumulative incidence of definite and probable stent thrombosis (Dublin criteria13) in patients treated with SES for multivessel disease with and without bifurcations and in subgroups according to lesion type and stenting strategy.
The search for independent predictors of ST by multivariate analysis identified only two variables: the presence of bifurcation(s) and maximal post-procedural CK-value. As these latter values have a highly skewed distribution the data were log transformed. On the log scale the maximum CK-value remained a significant factor. The presence of a bifurcation lesion by itself was integrated in the model but was of borderline significance (p= 0.0560). No other variable (specifically those highlighted by univariate analysis) was able to improve this model. Figure 6 gives the probability of definite ST in the bifurcation and non-bifurcation groups according to the model derived. Figure 7 illustrates the probability of any possible/ probable/ definite ST event as a function of the maximum CK-value.
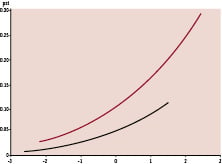
Figure 6. Probability of definite stent thrombosis for patients with (red line) and without (black line) bifurcation lesions according to the logarithm of the maximum post-procedural CK.
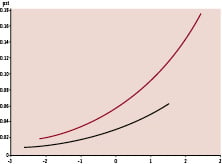
Figure 7. Probability of any (possible, probable and definite) stent thrombosis for patients treated with (red line) and without (black line) bifurcation lesions according to the logarithm of the maximum post-procedural CK value.
Discussion
Three-years after multivessel angioplasty with SES, clinical outcomes in patients treated for bifurcation lesions were equivalent to those in patients without bifurcation lesions. Bifurcation stenting in the context of multivessel PCI did not increase the risk of myocardial infarction, death or cerebrovascular events. Despite more extensive and complex coronary disease in patients with bifurcation lesions, revascularisation results were nonetheless maintained long-term with no requirement for repeat procedures in 85% over 3-years. There was no apparent difference in long-term outcomes even when the more complex “true” bifurcation subset was examined separately and the risk of repeat revascularisation was independent of a one- or two-stent strategy.
There was no excess of stent thrombosis observed in patients treated for bifurcation lesions, but the combination of definite and probable stent thrombosis, according to the ARC criteria, occurred more frequently after procedures involving treatment of a bifurcation.
The impact of bifurcation lesions in multivessel disease in the DES era
As documented for the entire ARTS II cohort, the frequency of bifurcation disease is high in patients with multivessel coronary disease (53% patients enrolled had at least one bifurcation lesion). Repeat revascularisation rates remain higher in bifurcation studies than in those of percutaneous interventions of simple single lesions, although the absolute incidence is reduced in the DES era6,7. While the forthcoming results of randomised studies1,2 will help to clarify the role of percutaneous revascularisation as an alternative to surgery in multivessel disease, they may not convince us as to whether the presence of a bifurcation lesion should alter our choice of treatment. The results presented here suggest similar outcomes in patients with and without bifurcations when using DES for multivessel disease.
Risk of stent thrombosis in bifurcation PCI
with DES
Bifurcation lesions have repeatedly been reported as one of the independent predictors of DES thrombosis14-16. Although definite stent thrombosis was not observed more frequently in this study, there was an excess of definite or probable stent thrombosis in patients with a bifurcated lesion. Without precise documentation of the majority of these events, their relationship to the bifurcation lesion itself or to the greater stent length and higher number of stents deployed in the bifurcation group, who had more extensive and complex disease, can only be hypothesised. Indeed, in multivariate analysis bifurcation treatment alone was not a significant independent predictor of thrombotic events. The search for such predictors in the 602 patients treated by multivessel PCI with SES was limited by a low event rate. The best model that could be derived comprised the combination of maximum CK rise and bifurcation treatment. The significance of CK rise as a predictor of ST is an interesting observation, which might be interpreted either as a higher risk of events in patients whose PCI was in the context of an acute coronary syndrome or as an important addition to the body of data suggesting that post-procedural CK rise is an important risk factor for future adverse events17,18.
Stenting strategy and 3-year results
Despite the inclusion of over 60% “true” bifurcations in this study, the vast majority of patients (81%) were treated using a single stent strategy. Consequently, this analysis does not contain sufficient data to confirm the safety and efficacy of complex bifurcation stenting in the context of multivessel angioplasty.
Limitations to this analysis
These data represent a post-hoc analysis of non-randomised subgroups of bifurcations and non-bifurcations. Therefore, no power or sample size calculation could be performed. Accordingly, the study may have been underpowered to detect significant differences in uncommon adverse events between the eventual two groups.
The ARTS II study examined clinical outcomes and there was no mandated angiographic follow-up. Consequently, the revascularisation rates reported in this analysis are truly clinically driven valid in a ‘real-world’ setting but remain difficult to compare with rates from controlled studies where MB or SB restenosis was actively sought and treated with prior knowledge of the angiographic appearances.
Conclusions
The use of DES in multivessel disease is associated with a reduced need for repeat revascularisation procedures. This remains true whether or not a bifurcation lesion is treated. Treatment of bifurcation disease in this setting does not increase the incidence of adverse clinical events in the first 3-years. The concerns about an increase in DES thrombosis following bifurcation angioplasty are supported by the finding of a two-fold increase in the rate of definite or probable stent thrombosis in these patients, but this does not translate into an increase in major adverse clinical events.

