Abstract
Aims: To explore optimal management strategies for bifurcation lesions with sirolimus-eluting stents (SES).
Methods and results: Among 12,824 patients enrolled in the j-Cypher Registry, we identified 2,122 patients with 2,250 non-left main bifurcation lesions (average age: 69 years; diabetes: 39%; acute coronary syndrome: 24%; lesion length ≥30mm: 17%; true bifurcation: 53%) treated exclusively with SES. The majority of lesions (1,978 lesions, 88%) were treated by provisional side branch stenting approach with a 4.5% crossover rate, while the elective two-stent approach (stenting both main and side branches) was adopted in 272 lesions. The 3-year incidence of target-lesion revascularisation (TLR) was significantly higher in the elective two-stent group than in the provisional group (18.5% vs. 9.8%, p<0.0001). The incidence of definite stent thrombosis was not different between the two groups (1.3% vs. 0.61%, p=0.21). Among 1,871 lesions with main branch stenting alone, final kissing balloon dilatation (FKB) was performed in 938 lesions (50%). The incidence of TLR was not different between the two groups with or without FKB (9.9% vs. 9.2%, p=0.98).
Conclusions: The provisional approach provided a good long-term outcome in the majority of lesions with low crossover rate to the two-stent approach. Lesions treated with FKB had similar TLR outcome to those without FKB after main branch stenting alone.
Introduction
Although coronary bifurcation lesions are frequently encountered in clinical practice, they remain a challenge for percutaneous coronary intervention (PCI) and the optimal stenting strategy has not been established in the current drug-eluting stent (DES) era. Several randomised controlled trials and meta-analyses comparing complex stenting strategy with provisional side branch stenting strategy consistently demonstrated that there were no differences in both the target lesion revascularisation (TLR) rate and the angiographic restenosis rate between the two strategies, although the incidence of myocardial infarction was higher after complex stenting.1-7 However, bifurcation lesions enrolled in these randomised trials might not represent more complex bifurcation lesions encountered in the real world clinical practice. The rates of crossover from provisional approach to complex approach varied widely among studies.
In the current pre-specified sub-analysis of the j-Cypher registry, we intend to compare the 3-year outcome of bifurcation stenting with sirolimus-eluting stents (SES) between the provisional side branch stenting approach and the elective two-stent approach (stenting both main and side branches) in a large number of patients in real world clinical practice. The effect of final kissing balloon dilatation (FKB) on TLR was also assessed, mainly in patients who underwent a bifurcation one-stent approach (main-branch stenting alone).
Methods
Study design and patient population
The study design, patient enrolment and data management for the j-Cypher registry has been previously described in detail.8 In brief, the j-Cypher registry is a physician-directed, prospective, multicentre registry in Japan enrolling consecutive patients undergoing SES implantation without any exclusion criteria (Supplemental data appendix A-C). Detailed information on bifurcation stenting strategies was recorded in the case report forms during the index stent implantation procedures. These included provisional or elective side branch stenting approaches, guidewire protection of the side branch before main branch stenting, rewiring in the side branch after main branch stenting, FKB and final side branch stenting.
From August 2004 to November 2006, 12,824 patients (19,675 lesions) were enrolled in the j-Cypher registry. There were 3,410 patients (26.6%) with bifurcation lesions (3,716 lesions). There were 1,143 patients (1,198 lesions) with distal left main coronary artery (LMCA) bifurcation lesions, including ostial left anterior descending coronary artery (LAD) and ostial left circumflex coronary artery (LCX) lesions. Excluding lesions treated by modalities other than SES and saphenous vein graft bifurcations, 2,122 patients (2,250 lesions) with non-LMCA native coronary artery bifurcation lesions treated exclusively with SES constituted the study population for the current analysis (Figure 1).
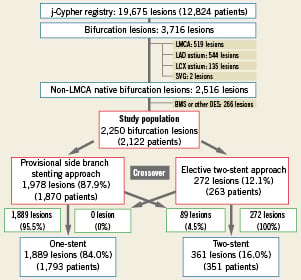
Figure 1. Patients and lesion flow-chart. LAD: left anterior descending coronary artery; LCX: left circumflex coronary artery; LMCA: left main coronary artery; SVG: saphenous vein graft
We compared 3-year incidences of TLR and definite ST on a lesion-level basis between a provisional side branch stenting approach (provisional group: 1,978 lesions in 1,870 patients), and an elective two-stent approach (elective two-stent group: 272 lesions in 263 patients). Excluding 11 patients who had both types of lesions with provisional and elective side-branch stenting, 2,111 patients constituted the analysis set for clinical events such as death, cardiac death, MI and coronary artery bypass grafting (CABG) surgery. Subgroup analyses were also carried out to evaluate the effect of FKB on TLR outcome in lesions treated with main branch stenting alone (one-stent group) and in lesions treated with final two-stent.
The relevant review boards in all 37 participating centres approved the study protocol. Written informed consent was obtained from all patients enrolled.
Definitions
A “bifurcation lesion” was defined as that involving a side branch of ≥2.2 mm in diameter. The sizes of the side branches were visually estimated by the site investigators. Bifurcations were stratified according to the Medina classification.9 Medina class was also visually adjudicated by the site investigators. Selection of the bifurcation stenting strategies was left to the operator’s discretion. Techniques of stenting were pre-specified and recorded in the case report forms during the index stent implantation procedures. When stenting of the side branch ostium was performed before stenting of the main branch, the procedure was regarded as an elective two-stent strategy. When stenting of the side-branch ostium was performed after stenting of the main vessel, the procedure was regarded as a provisional side branch stenting strategy. The two-stent strategies were further classified into four patterns (T-stenting, Crush stenting, Culotte stenting and Kissing stent). Decision regarding the FKB was also left to the operators.
Quantitative angiographic analysis (QCA) was performed and reported by the site investigators (single vessel QCA [CMS, CAAS II, Centricity Cardiology CA 100 V2, Toshiba Cardio Agent, and CCIP-310/W]: 1,564 lesions, and visual estimation: 680 lesions).
Definitions for the clinical events were previously described.8 Definite ST on a lesion-level basis was used as the endpoints for ST. TLR was defined as either PCI or CABG due to restenosis or thrombosis of the target lesion that included the proximal and distal edge segments as well as the ostium of the side branches.
Statistical methods
Continuous variables were expressed as mean value±standard deviation unless otherwise stated, and were compared using the Student’s t-test or Wilcoxon rank sum test based on distribution. Categorical variables were compared using the chi-square test. Cumulative incidences of adverse events were estimated by the Kaplan-Meier method and the differences were compared using the log-rank test.
In an attempt to adjust for the differences in baseline clinical, angiographic and procedural characteristics between the provisional and elective two-stent group, a multivariable logistic regression model was constructed using TLR at three years as dependent variable and 30 baseline and procedural factors listed in Table1 including FKB as well as the treatment strategy of bifurcation lesions (provisional or elective two-stent) as independent variables. A multivariable logistic regression model instead of Cox proportional hazard model was used, because the timing of TLR could be highly influenced by physicians’ and patients’ decision. Actually, proportional hazard assumption was not justified for TLR in the current analysis. Eligible lesions for logistic regression analysis included those lesions with TLR within three years (202 lesions) relative to those lesions with complete follow-up and without TLR at three years (674 lesions). Continuous variables were dichotomised by clinically meaningful reference values. We selected variables with p<0.05 in the univariate analyses together with the treatment strategy of bifurcation lesions (provisional or elective two-stent) and included them simultaneously in a multivariable model. The effect of FKB on TLR was also evaluated among lesions with final one-stent placement by a multivariable logistic regression model including percent diameter stenosis of the ostium of the side branch after main branch stenting as an additional independent variable. Adjusted risk of elective two-stent approach and FKB for TLR were expressed as odds ratios (OR) and their 95% confidence intervals (CI).
The logistic regression model required exclusion of cases without 3-year follow-up. This seriously reduced the available subject pool and offered large opportunity for the introduction of biases due to historical timing and drop out. Therefore, the Cox proportional hazard model was also used as a sensitivity analysis.
Probability was considered significant at p<0.05. All statistical tests were two-tailed. All statistical analyses were conducted by physicians (Toshihiro Tamura and Takeshi Kimura) and by an independent statistician (Takeshi Morimoto) with the use of JMP 7 (SAS Institute Incorporated, Cary, NC, USA) and SAS 9.1 (SAS Institute).
Results
Baseline characteristics and procedural data
Among 2,250 lesions enrolled, the proportion of true bifurcation lesions was 53% (Table 1). The majority of lesions (88%) were treated by provisional side branch stenting approach. The crossover from the provisional group to the elective two-stent group was seen only in 4.5% (89 lesions). Finally, 1,889 lesions (84.0%) were treated by one-stent approach and 361 lesions (16.0%) were treated by two-stent approach (Figure 1). Baseline clinical characteristics were generally similar between the provisional and elective two-stent groups (Table1A). In terms of lesion and procedural characteristics, the proportions of LAD lesions were not different between the two groups. The prevalences of true bifurcation, chronic total occlusion, and use of FKB were significantly higher in the elective two-stent group than in the provisional group. Reference diameter and percent diameter stenosis before the procedure in the side-branches were greater in the elective two-stent group than in the provisional group (Table1B). In the final two-stent group, the techniques of two-stent placement included T-stenting (59%), crush stenting (20%), culotte stenting (16%) and kissing stenting (4.7%).
Clinical outcomes: the provisional approach versus the elective approach
The median follow-up was 826 days (interquartile range, 666-1,095 days). Cumulative incidence of TLR at three years was significantly higher in the elective two-stent group than in the provisional group (18.5% vs. 9.8%, p<0.0001) (Figure 2). The difference remained significant after adjusting baseline and procedural characteristics by both logistic regression model and Cox proportional hazard model (Supplemental Table 1, 2).
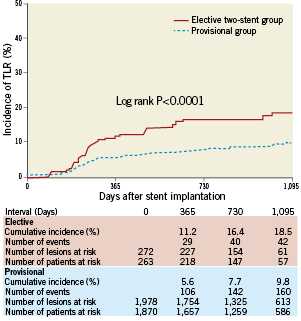
Figure 2. Cumulative incidence of TLR compared between the elective two-stent group and the provisional side branch stenting group. TLR: target lesion revascularisation
The cumulative incidence of ARC definite ST at 3-years was not different between the elective two-stent group and the provisional group (1.3% vs. 0.61%, p=0.21) (Figure 3). The incidences of other clinical events such as death, cardiac death, MI, and CABG were similar between the two groups (Table 2).
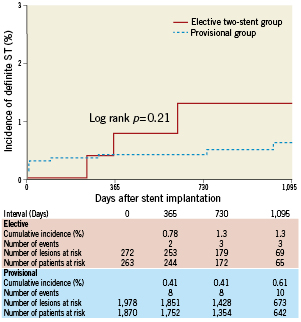
Figure 3. Cumulative incidence of definite ST compared between the elective two-stent group and the provisional side branch stenting group. ST: stent thrombosis
Effect of final kissing balloon dilatation on TLR
Among 1,889 lesions with final one-stent placement, FKB was performed in 938 lesions (50%). Among 933 lesions without FKB, crossing of a guidewire or balloon was unsuccessful in 50 lesions (5.4%), while FKB was not attempted in 883 lesions (95%). Data on percent diameter stenosis of the ostium of the side branch was reported in 1,871 lesions. Clinical characteristics were generally similar between the two groups of patients with or without FKB (Table3A). With respect to lesion characteristics, the prevalence of Y-shaped lesions and chronic total occlusion were significantly higher in the FKB group. The prevalence of severe calcification was significantly higher in the non-FKB group. Reference diameter and percent diameter stenosis before the procedure in the side-branches were not different between the two-groups (Table3B). The proportion of patients with percent diameter stenosis of the ostium of the side branch ≥50% after stenting of the main branch was significantly higher in the FKB group than in the non-FKB group (60% vs. 53%, p=0.002) (Figure 4).
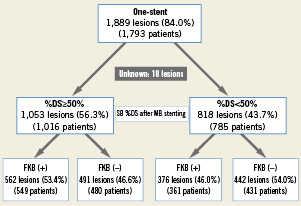
Figure 4. Lesion flow-chart for final kissing balloon dilatation in lesions treated with one-stent strategy DS: diameter stenosis; FKB: final kissing balloon dilatation; MB: main-branch; SB: side branch
The cumulative incidence of TLR at 3-years was similar between the two groups with or without FKB (9.9% vs. 9.2%, p=0.98) (Figure5). The cumulative incidences of TLR at 3-years were also similar between the two groups irrespective of percent diameter stenosis of the ostium of the side branch ≥50% or <50% after stenting of the main branch (Figure 6). The difference remained insignificant after adjusting baseline and procedural characteristics by both logistic regression model and Cox proportional hazard model (Supplemental Table 3, 4).
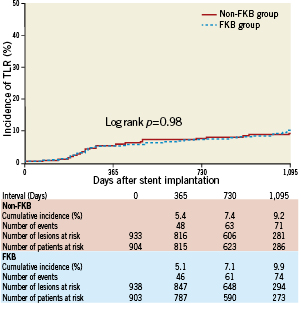
Figure 5. Cumulative incidence of TLR compared between the FKB group and the non-FKB group in lesions treated with a one-stent strategy. FKB: final kissing balloon dilatation; TLR: target lesion revascularisation
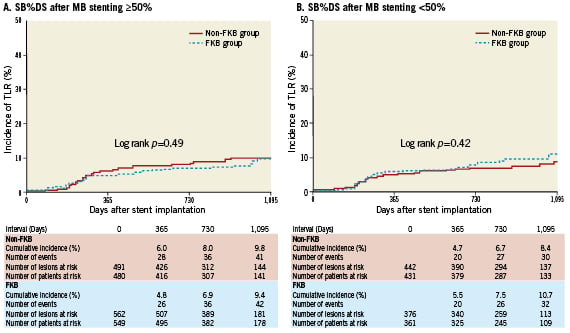
Figure 6. Cumulative incidence of TLR compared between the FKB group and non-FKB group; (A) in lesions ≥50% SB%DS after MB stenting, and (B) in lesions <50% SB%DS after MB stenting. DS: diameter stenosis; FKB: final kissing balloon dilatation; MB: main branch; SB: side branch; TLR: target lesion revascularisation.
Discussion
There were three main findings in the present study. First, provisional side branch stenting approach with SES could be applicable in the majority of patients with bifurcation lesions in the real world with low rate of crossover to two-stent approach and with low rate of TLR. Second, we did not notice any safety concerns for the elective two-stent approach as compared with the provisional side branch stenting approach in terms of death, MI and ST. Third, among the final one-stent group, lesions treated with FKB had similar TLR outcome to those lesions without FKB.
Two relatively large randomised controlled trials comparing complex strategy with simple strategy in bifurcation lesions consistently demonstrated low rate of TLR in Nordic Bifurcation study (1.0% vs. 1.9% at 6 months, p=0.36) and low rate of target vessel failure in BBC-ONE study (7.2% vs. 5.6% at 9 months, p=0.43).1,6 The rates of crossover from simple strategy to complex strategy were also very low in both studies (4% and 3%, respectively). However, considering the low rates of both TLR and crossover, it is likely that relatively simple bifurcation lesions suitable for simple strategy were preferentially enrolled in these trials. The CACTUS study, which compared crush stenting with provisional side branch stenting only in true bifurcation lesions, reported relatively high crossover rate (31%) with equivalent rates of angiographic restenosis and clinical events.4 Therefore, it is currently unknown what proportion of bifurcation lesions encountered in the real world clinical practice could be treated safely and effectively with simple strategy. In the current study encompassing a larger number of patients with complex clinical characteristics, the provisional side branch stenting approach was adopted in 88% of lesions with low rate of crossover (4.5%), suggesting that the simple approach could be applicable in the majority of patients with bifurcation lesions. However, we should be aware that the threshold for crossover varies widely across operators, and we do not currently know the optimal threshold for crossover because we have no studies evaluating the impact of residual stenosis in the side branch on clinical outcomes.
Despite observed higher rate of TLR in the two-stent group, we should emphasise that lesions, which need treatment with two-stents, are very different from lesions that need one stent. This registry was not constructed with the purpose of evaluating the advantage of one-stent versus two-stent techniques. Considering the very selective use of elective two-stent approaches in more complex lesions, TLR rate of 18.5% at 3-year seemed to be acceptable. It was also reassuring that there was no signal suggesting safety concerns for the elective two-stent approach in non-LMCA coronary bifurcations. Therefore, although the elective two-stent approach as a routine strategy should be discouraged, it may be necessary when dealing with large proximal side branches that cannot be ignored.
The absence of FKB was reported to be a risk factor for TLR after DES implantation with the crush stenting technique.10 Ormiston et al also suggested the need for FKB to ensure optimal geometry of both stents and adequate scaffolding of both vessels by the bench test.11 Therefore, FKB seems to be a better strategy in the two-stent approach. Two randomised studies evaluated the efficacy of FKB in the one-stent approach. In the THUEBIS study, there was no significant difference in the rate of TLR between the mandatory FKB group and the provisional side branch balloon dilatation group after stenting of the main branch (17.9% vs. 14.8%, p=0.7).12 In the Nordic Bifurcation III study, there was no difference in the incidence of TLR between FKB group and non-FKB group in patients with the one-stent approach (1.3% vs. 2.1%, p>0.05). (TransCatheter Therapeutics, 2009, oral presentation) The current study confirmed these previous observations. Even in lesions with a percent diameter stenosis of side branches ≥50% after main-branch stenting, lesions treated with FKB had similar TLR outcome to those lesions without FKB. However, we should emphasise the fact that operators decided when to perform final kissing inflation. The current study does not determine the value of FKB, while giving importance to the selective performance of this manoeuvre.
Study limitations
There are several limitations in the present study. First, it was a non-randomised study. The choices for stenting strategies and for the use of FKB were left to the operator’s discretion. The outcomes between the elective group and the provisional group could still have been biased, even after adjusting for known confounders. Importantly, we did not evaluate lesion length of the side branch that might be an important determinant of the outcome of bifurcation stenting. Second, QCA was not performed by a core laboratory.
Conclusions
For SES placement in non-LMCA bifurcation lesions, the provisional side branch stenting approach provided a good long-term outcome in the vast majority of bifurcation lesions encountered in daily practice, with a low rate of crossover to the two-stent approach. Lesions treated with FKB had similar TLR outcome to those lesions without FKB after main-branch stenting alone.
Acknowledgements
We gratefully thank the members of the cardiac catheterisation laboratories of the participating centres, as well as the clinical research coordinators.
Funding sources
The study sponsor, Cordis Cardiology Japan, a Johnson and Johnson Company, was involved in the discussion of the study design. However, the study sponsor was not involved in the collection, analysis and interpretation of data; in the writing of the report or in the decision to submit this paper for publication.
Conflict of interest statement
Dr. Kimura serves as an advisory board member and member of the speakers’ bureau for Cordis Cardiology and has received honoraria from Cordis Cardiology. The remaining authors have no conflicts of interest to declare.
Online data supplement
Supplemental Table 1. Unadjusted and adjusted comparison in the risk of TLR between elective and provisional strategies by the multivariable logistic regression model.
Supplemental Table 2. Unadjusted and adjusted comparison in the risk of TLR between elective and provisional strategies by the Cox proportional hazard model.
Supplemental Table 3. Unadjusted and adjusted comparison in the risk of TLR between the FKB and non-FKB groups by the multivariable logistic regression model.
Supplemental Table 4. Unadjusted and adjusted comparison in the risk of TLR between the FKB and Non-FKB groups by the Cox proportional hazard model.
Supplemental Appendix A. List of participating centres and investigators for the j-Cypher registry.
Supplemental Appendix B. List of clinical research coordinators.
Supplemental Appendix C. List of clinical events committee members.