Abstract
Aims: It has not been known which two-stent technique is best for treating bifurcation lesions. We aimed to compare the outcomes from main vessel (MV) first and side branch (SB) first techniques for patients with bifurcation lesions requiring a two-stent approach.
Methods and results: A total of 673 patients with bifurcation lesions were treated with two-stent techniques: MV first (n=250) or SB first (n=423). The rate of a composite of cardiac death, myocardial infarction, or target lesion revascularisation (TLR) was similar in the two groups (SB first versus MV first, 15.1% versus 15.6% in the total population [p=0.90]; 14.3% versus 17.4% in a propensity score-matched population [p=0.80]). There were significant interactions associated with TLR risk between MV and SB first techniques according to angiographic factors. Patients in the MV first group had a lower risk of TLR when they had a lesion with MV diameter stenosis ≥70% (p for interaction=0.04), more severe stenosis of the MV than of the SB (p for interaction=0.008), or MV lesion length ≥18 mm (p for interaction=0.01).
Conclusions: Clinical outcomes were similar for patients treated with MV or SB first two-stent techniques. Using “more severe lesion first” two-stent techniques might offer a favourable prognosis. ClinicalTrials.gov number: NCT01642992
Abbreviations
COBIS II: COronary BIfurcation Stenting II
DES: drug-eluting stent(s)
MACE: major adverse cardiac events
MLD: minimum luminal diameter
MV: main vessel
PCI: percutaneous coronary intervention
RD: reference diameter
SB: side branch
TIMI: Thrombolysis In Myocardial Infarction
TLR: target lesion revascularisation
Introduction
A provisional side branch (SB) intervention after main vessel (MV) stenting is currently the standard treatment for coronary bifurcation lesions1. In randomised controlled trials comparing one-stent versus two-stent techniques, however, crossover from one-stent to two-stent techniques occurred somewhat frequently for patients who were assigned to receive one-stent techniques2,3. Furthermore, two-stent techniques are frequently needed in real-world practice4. Although a variety of two-stent techniques have been used to treat coronary bifurcation lesions, there is a paucity of studies that compare the outcomes from different two-stent techniques5,6. In our previous study, we were not able to identify significant outcome differences between MV first and SB first techniques, possibly due to the relatively small sample size and the short duration of follow-up7. Therefore, we sought to compare MV first and SB first two-stent techniques among patients with coronary bifurcation lesions using a large bifurcation registry with a long duration of follow-up.
Methods
STUDY POPULATION
This observational, multicentre registry enrolled 2,897 patients with coronary bifurcation lesions who underwent percutaneous coronary intervention (PCI) with drug-eluting stents (DES) from 18 major coronary intervention centres in the Republic of Korea between January 2003 and December 2009. The protocol was approved by each hospital’s institutional review board; the need for informed consent for access to each institutional registry was waived. The design, inclusion and exclusion criteria, and data collection methods of the COronary BIfurcation Stenting (COBIS) II registry have been described previously8. In brief, patients treated with DES for coronary bifurcation lesions with an MV diameter ≥2.5 mm and SB diameter ≥2.3 mm according to core laboratory analyses were included. Patients who had experienced cardiogenic shock or cardiopulmonary resuscitation, and patients with a protected left main disease were excluded.
To compare MV first and SB first two-stent techniques, we excluded patients undergoing one-stent techniques, defined as the presence of stents at the MV or SB ostium (n=2,127) and selected only patients who were treated with two-stent techniques, defined as the presence of stents at both the MV and SB ostium (n=770). Patients treated with kissing or V-stenting techniques (n=97) were excluded because they could not be divided into either the MV first or the SB first group. Finally, 673 patients being treated with MV first or SB first techniques were included in our analyses (Figure 1). PCI was performed according to current practice guidelines. The treatment strategy, stenting techniques, type of DES, use of intravascular ultrasound or non-compliant balloon, and implementation of final kissing balloon inflation were determined according to the operator’s discretion.
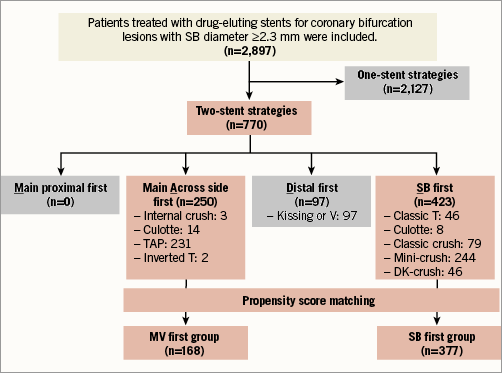
Figure 1. Study flow chart. Among patients with coronary bifurcation lesions with an SB diameter ≥2.3 mm, we excluded patients undergoing one-stent techniques and selected patients treated with two-stent techniques. “MADS classification” was based on the manner in which the first stent had been implanted: Main proximal first, main Across first, Distal first, and SB first. No patient was treated with a main proximal first technique. Patients treated with kissing or V-stenting techniques were excluded because they could not be divided into “main across side first (MV first)” or “SB first” groups. Finally, patients treated with MV first or SB first techniques were included in our analysis. DK: double kissing; MV: main vessel; SB: side branch; TAP: T-stenting and small protrusion
DATA COLLECTION AND ANGIOGRAPHIC ANALYSIS
Data were obtained using a web-based reporting system. Coronary angiograms were analysed at the angiographic core laboratory (Samsung Medical Center, Seoul, Republic of Korea) using an automated edge-detection system (Centricity CA1000; GE Healthcare, Waukesha, WI, USA). Bifurcation lesions were divided into three segments for quantitative coronary angiographic analysis: proximal MV, distal MV, and SB ostium8. We determined the minimum luminal diameter (MLD) and reference diameter (RD) for each segment.
STUDY OUTCOMES AND DEFINITIONS
The primary outcome was major adverse cardiac events (MACE), which were defined as a composite of cardiac death, myocardial infarction, or target lesion revascularisation (TLR) that occurred during follow-up. The secondary outcomes included individual components of the composite primary outcome, death from any cause, and definite or probable stent thrombosis. The study outcome definitions of the COBIS II registry have been described previously9.
STATISTICAL ANALYSIS
Categorical variables were summarised as frequencies with percentages and were compared using the chi-square test or Fisher’s exact test. Continuous variables were presented as a median with 25th-75th percentiles and were compared using the t-test or Wilcoxon rank-sum test. Time-to-event hazard curves were estimated with the Kaplan-Meier method and were compared using a log-rank test. To minimise the impact of selection bias and any potential confounders, we adjusted for differences in baseline characteristics using propensity score-matching methods. The propensity score was created using the preprocedural variables shown in Table 1 and Table 2, and the pairs were matched at varied matching ratios using the nearest neighbour method with a calliper width of 0.2 times the SD10. A covariate was considered balanced if the standardised mean difference of each variable was less than 10%. To find angiographic determinants of SB first techniques, we used multivariable logistic regression models that included quantitative coronary angiographic variables. Receiver operating characteristic (ROC) curves were used to evaluate the optimal cut-off value. The effects of interaction terms between subgroups and treatment effects on clinical outcomes were estimated using Cox regression models. All p-values were two-tailed, and p<0.05 was considered statistically significant. All analyses were performed using R software version 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
BASELINE CHARACTERISTICS
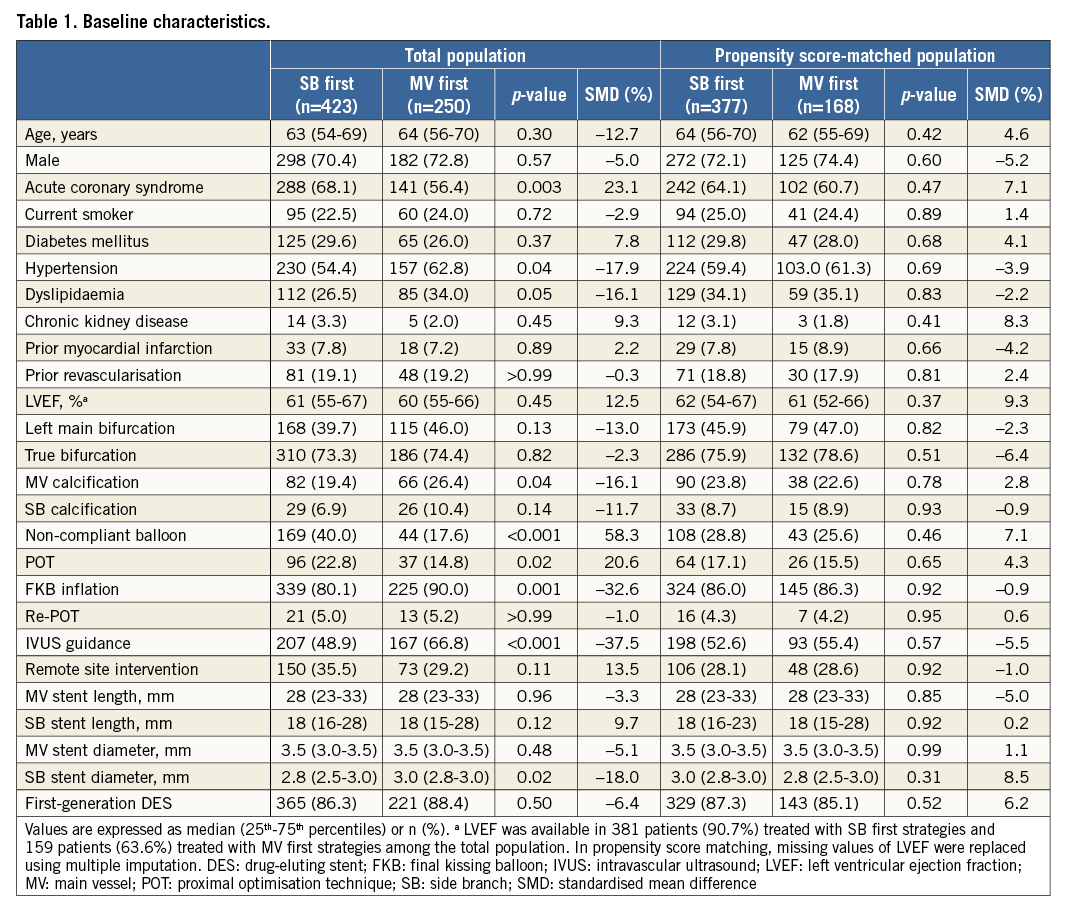
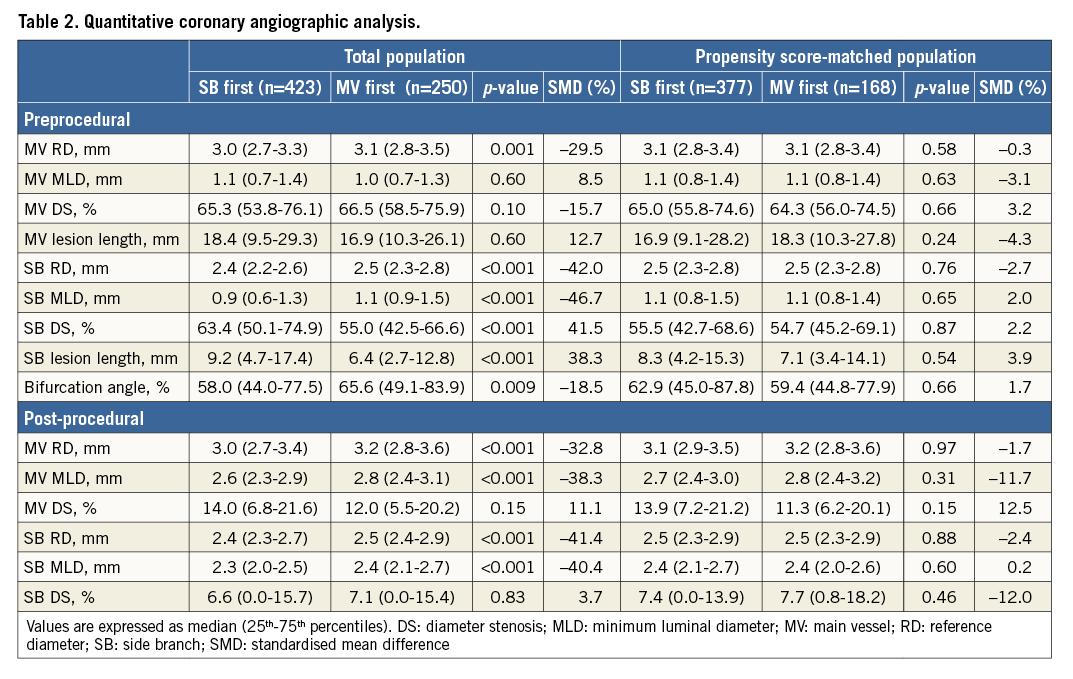
Among the 673 eligible patients, SB first techniques were performed in 423 patients (63%) and MV first techniques were performed in 250 patients (37%). The clinical, angiographic, and procedural characteristics of the two groups are shown in Table 1. The SB first techniques group had a higher prevalence of acute coronary syndrome at admission. Patients treated with SB first techniques were also younger and had a higher left ventricular ejection fraction than those treated with MV first techniques. SB first techniques were used less frequently for left main bifurcation lesions and calcified lesions, compared with MV first techniques. Non-compliant balloon and remote site intervention were performed more frequently in patients treated with SB first techniques, while final kissing balloon inflation and intravascular ultrasound were performed less frequently in patients who underwent SB first techniques. Preprocedural quantitative coronary angiographic data are presented in Table 2. MV RD, SB RD, percent MV diameter stenosis, and bifurcation angle were smaller in patients treated with SB first techniques. However, patients treated with SB first techniques had higher percent SB diameter stenosis and a longer MV and SB lesion length compared to those who underwent MV first techniques.
After propensity score matching, a total of 545 patients remained in the matched population: 377 patients in the SB first group and 168 patients in the MV first group (Table 1, Table 2). There were no significant imbalances in baseline variables between the matched populations. Patients treated with SB first techniques had a tendency towards greater post-procedural MV residual stenosis compared to those who received MV first techniques.
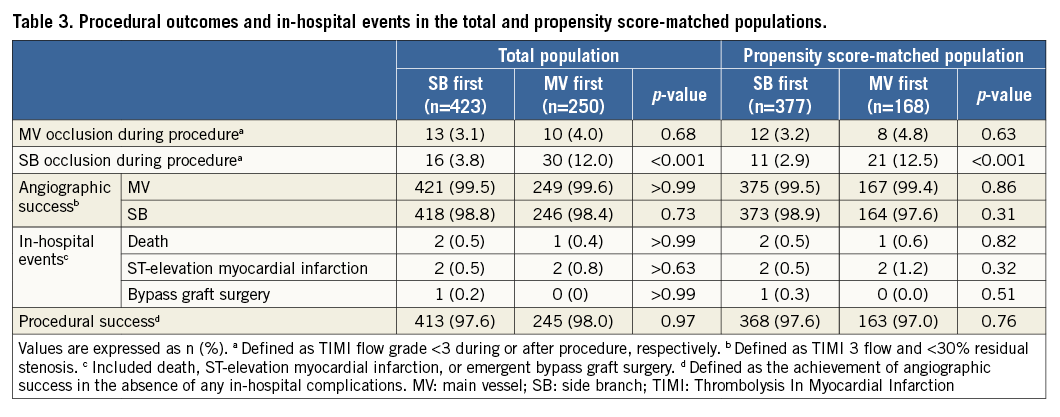
PROCEDURAL OUTCOMES
As shown in Table 3, SB occlusion occurred less frequently in patients treated with SB first techniques than in those treated with MV first techniques among the total and propensity score-matched populations. Other procedural outcomes occurred similarly between the two groups.
CLINICAL OUTCOMES
Complete clinical follow-up data were obtained for 96.3% of all patients at a median of 36 months (25th-75th percentiles, 24-52 months). Observed clinical outcomes are shown in Table 4. MACE was observed similarly among 64 patients in the SB first group (15.1%) and among 39 patients in the MV first group (15.6%; hazard ratio [HR] 0.97, 95% confidence interval [CI]: 0.65-1.45; p=0.90) (Figure 2). Definite or probable stent thrombosis occurred in eight patients in the SB first group (1.9%) and in five patients in the MV first group (2.0%; HR 0.93; 95% CI: 0.30-2.84; p=0.90). In the propensity score-matched population, the SB first group did not differ from the MV first group with respect to MACE (HR 0.91, 95% CI: 0.59-1.41; p=0.67) or definite or probable stent thrombosis (HR 0.52, 95% CI: 0.14-1.92; p=0.33).
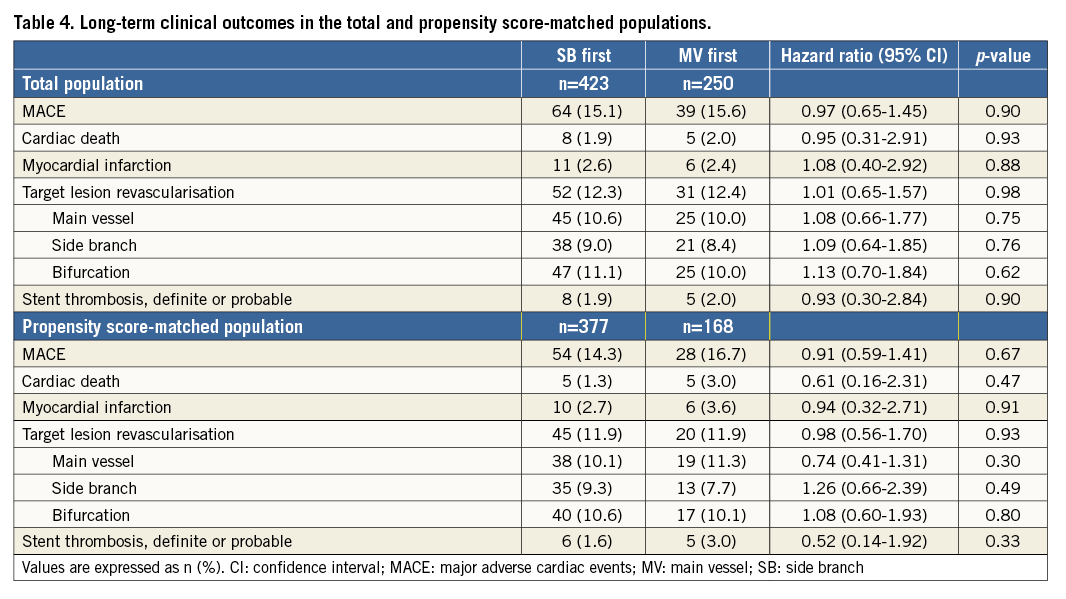
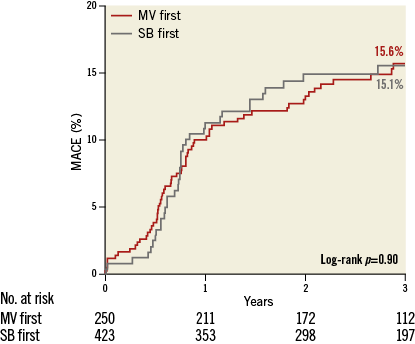
Figure 2. Kaplan-Meier curve for major adverse cardiac events in the total population. Time-to-event hazard curves are presented with Kaplan-Meier estimates and were compared using a log-rank test. MACE: major adverse cardiac events; MV: main vessel; SB: side branch
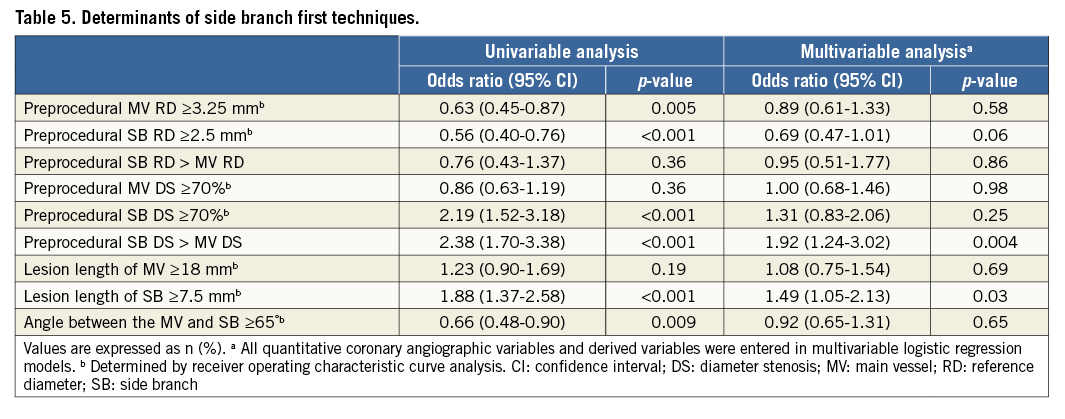
ANGIOGRAPHIC DETERMINANTS OF SB FIRST TECHNIQUES
Multivariable logistic regression analysis identified independent factors associated with SB first techniques (Table 5). Greater preprocedural percent SB diameter stenosis compared to MV stenosis (odds ratio [OR] 1.92, 95% CI: 1.24-3.02; p=0.004) and SB lesion length ≥7.5 mm (OR 1.49, 95% CI: 1.05-2.13; p=0.03) were significantly associated with SB first techniques.
DIFFERENTIAL EFFECTS ON THE RISK FOR TLR BETWEEN MV FIRST AND SB FIRST TECHNIQUES ACCORDING TO ANGIOGRAPHIC FINDINGS
There were significant interactions associated with risk for TLR between the MV first and SB first techniques according to the MV diameter stenosis, relative stenosis severity of the MV versus the SB, or MV lesion length (Figure 3). Patients in the MV first group had a lower risk for TLR when they had bifurcation lesions with MV diameter stenosis ≥70% (p for interaction=0.04), more severe stenosis of the MV than the SB (p for interaction=0.008), or MV lesion length ≥18 mm (p for interaction=0.01).
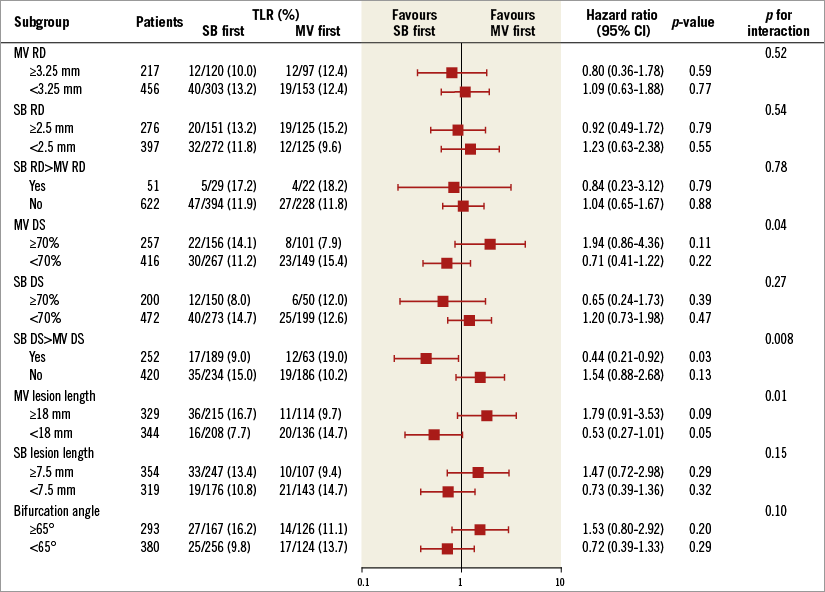
Figure 3. Differential effects on the risk for target lesion revascularisation between main vessel and side branch first techniques according to angiographic findings. Cut-off values were determined using receiver operating characteristic curve analysis. The treatment effects of interaction terms between subgroups on TLR risk were estimated using Cox regression models. CI: confidence interval; DS: diameter stenosis; MV: main vessel; RD: reference diameter; SB: side branch; TLR: target lesion revascularisation
Discussion
Using data from a large, multicentre bifurcation registry, we compared the long-term clinical outcomes from patients treated with MV first or SB first techniques for coronary bifurcation lesions. There are four main findings from this present study: (1) during the follow-up period (median, 36 months; 25th-75th percentiles, 24-52 months), comparable procedural and clinical outcomes were observed between the MV first and SB first groups in the total and propensity score-matched populations; (2) SB occlusion occurred less frequently in patients treated with SB first techniques than in those treated with MV first techniques; (3) SB first techniques were attempted for coronary bifurcation lesions with greater preprocedural percent diameter stenosis of the SB than the MV, or SB lesion length ≥7.5 mm; (4) there were significant interactions for TLR risk between MV first and SB first techniques according to MV diameter stenosis, relative stenosis severity of the MV versus the SB, and MV lesion length.
Meta-analyses of previous randomised controlled trials showed that provisional one-stent techniques were comparable to elective two-stent techniques in terms of clinical outcomes, but superior to elective two-stent techniques in terms of the reduced risk for periprocedural myocardial infarction1. However, patients with complex bifurcation lesions such as large SBs with severe stenosis extending from the ostium were not represented in these randomised controlled trials. Provisional or elective two-stent techniques are still needed for patients with complex bifurcation lesions4. To date, few studies have examined the comparative outcomes from different two-stent techniques, because there are many subtypes, which make it difficult to evaluate the clinical outcome for patients with coronary bifurcation lesions. The Nordic Stent Technique Study showed that the three-year clinical outcomes were similar for patients with coronary bifurcation lesions treated with crush versus culotte stent techniques5. However, the DK-CRUSH III study showed that culotte stenting was associated with significantly increased risks for three-year clinical outcomes compared with DK-crush stenting for left main distal bifurcation lesions6. Our previous study comparing the outcomes between main across side first and SB first techniques failed to show clearly which technique was superior, because we had a relatively small sample size and a short duration of follow-up7. Therefore, we assessed the long-term comparative outcomes after treatment with MV first or SB first techniques during coronary bifurcation PCI using data from a large, multicentre, bifurcation-dedicated registry.
During the median follow-up duration of 36 months (25th-75th percentiles, 24-52 months), the MACE rate was 15.6% in patients treated with MV first techniques and 15.1% in patients treated with SB first techniques. These results were consistent with those of the propensity score-matched population from our study, as well as in the Nordic Stent Technique Study5. According to our study and other previous data, there seem to be no best two-stent technique that may be generally recommended for treating coronary artery bifurcation lesions. Therefore, the operator may choose one of the many techniques according to the coronary anatomy of the patient and personal experience. In our study, operators preferred SB first techniques for coronary bifurcation lesions with more severe stenosis of the SB than of the MV or in cases of long SB lesion length. These practice patterns probably reflect the operators’ intention to avoid SB occlusion during the procedure. SB ostial stenosis and lesion length were proposed as independent factors associated with SB occlusion in our previous study8.
We performed subgroup analyses to identify differential treatment effects between two-stent techniques and risk for TLR according to specific lesion subsets. The treatment effect varied depending on MV diameter stenosis, relative stenosis severity of the MV versus the SB, and MV lesion length. The MV first techniques had a lower risk of TLR when applied to bifurcation lesions with MV diameter stenosis ≥70%, more severe stenosis of the MV than of the SB, or MV lesion length ≥18 mm. These results suggest that the MV first treatment strategy for more severe lesions in the MV than in the SB or the SB first treatment strategy for more severe lesions in the SB than in the MV could reduce the TLR risk in patients treated with two-stent techniques for coronary bifurcation lesions. One possible explanation is underexpansion of the second stent; during two-stent techniques, implantation of the first stent ensures good stent expansion and warrants preservation of vessel patency. However, it is possible for the second stent to expand insufficiently in cases of severe lesions after a complex procedure, and this is associated with a high incidence of TLR.
Limitations
Our retrospective study had several limitations. First, the choice of two-stent technique was not randomised and could reflect individual operator preference. Some angiographic and procedural characteristics, including left main disease, use of non-compliant balloon, and final kissing balloon inflation, were different between the two groups in the total population. To reduce the selection bias for the use of two-stent techniques and potential confounding effects, we performed a propensity score-matched analysis. Nevertheless, we were not able to correct for unmeasured variables, and it is difficult to predict how residual confounding can impact on clinical outcomes. Second, this study included a relatively small number of patients, and was therefore underpowered for comparison of clinical outcome. We assessed the differential effects on TLR risk between MV and SB first techniques across various angiographic subgroups. Although the results of a subgroup analysis should be interpreted carefully, it may be possible to generate a hypothesis regarding the relationship between two-stent techniques and long-term clinical outcomes. Third, intravascular ultrasound data for evaluating vessel size, plaque distribution, stent underexpansion, stent malapposition, or incomplete stent coverage of SB ostium bifurcation stenting were not available in the COBIS II registry. Fourth, we analysed coronary angiograms using single-vessel quantitative coronary angiography software, which might be inaccurate when used in bifurcation lesions due to the specific anatomical characteristics of bifurcations. Finally, large numbers of patients were treated with first-generation DES. Adequately powered registries or randomised trials using newer-generation DES are needed to evaluate the safety and efficacy of the two-stent techniques for coronary bifurcation PCI.
Conclusions
The clinical outcomes were similar for patients treated with MV first or SB first two-stent techniques. Coronary bifurcation lesions requiring two-stent techniques were treated using “more severe lesion first” techniques, which might offer a favourable clinical outcome.
| Impact on daily practice Treatment strategies using “more severe lesion first” two-stent techniques were significantly associated with favourable clinical outcomes. |
Acknowledgements
We appreciate the excellent statistical support from Joonghyun Ahn, MS, and Keumhee Cho Carriere, PhD, at the Samsung Biomedical Research Institute.
Funding
This work was supported by the Korean Society of Interventional Cardiology, Seoul, Republic of Korea.
Conflict of interest statement
The authors have no conflicts of interest to declare.