Abstract
Aims: We sought to determine if outcomes differ between provisional (elective side branch stenting) compared to a routine two-stent strategy (mandatory side branch stenting) for the treatment of bifurcation stenoses of the coronary arteries using drug-eluting stents.
Methods and results: We searched Medline, EMBASE, and the Cochrane library from January 2000 to February 2009 for studies comparing the provisional and two-stent strategies. Six randomised controlled trials, including 1,641 patients, were identified. The relative risk (95% confidence interval) for death, MI, target lesion revascularisation, and stent thrombosis within 1-year of the index procedure for a provisional vs. two-stent strategy were 1.12 (0.42-3.02), 0.57 (0.37-0.87), 0.91 (0.61-1.35), and 0.56 (0.23-1.35), respectively. By quantitative coronary angiography, there was no difference in the difference in means (95% CI) between the provisional and two-stent strategies for percent diameter stenosis (95% CI) in the main vessel or side branch, -1.08 (-2.91 to 0.74) and 1.30 (-3.35 to 5.96), respectively.
Conclusion: While death, stent thrombosis, and restenosis were similar between the treatment groups, MI was more common with the two-stent strategy. Thus, compared to a routine two-stent strategy, provisional stenting yields similar efficacy with superior safety and lower costs.
Introduction
Bifurcation lesions are observed in 15-20% of patients undergoing percutaneous coronary intervention (PCI)1. In these cases, the immediate objectives are to safely establish patency of the parent vessel while not compromising, and in many cases treating obstruction intrinsic to, the side branch. Along with these goals, the maintenance of long-term patency of both vessels is highly desirable. The optimal procedural strategy to achieve these aims in coronary stenoses involving a bifurcation remains controversial. There are two general approaches in the management of bifurcation disease. The first strategy, provisional T-stenting, is characterised by stenting of the main branch and elective stenting of the side branch and is less technically demanding; however, the angiographic results are typically less favourable compared to routine stenting of the side branch. In the second strategy, two stents are used to treat both the main vessel and side branch by the crush, culotte, or other techniques in an attempt to both adequately secure side branch patency and cover the bifurcation carina2-5. While technically more demanding, a two-stent strategy typically yields a superior angiographic result.
A limitation in the treatment of bifurcation stenoses with bare metal stents was the high rates of restenosis, in particular with a two-stent strategy6,7. Whether the marked reduction in restenosis with drug-eluting stents could be extended to the management of bifurcation stenosis was explored in a subgroup analysis of the SCANDSTENT trial8. In this trial, the reduction in restenosis and late lumen loss was greater with the sirolimus-eluting stent compared to bare metal stents. With the marked reduction in restenosis observed with use of drug-eluting stents in non-bifurcation stenoses, it is plausible that treatment of bifurcation stenosis with a two-stent approach using drug-eluting stents could yield superior outcomes compared to a provisional approach. In the present systematic review and meta-analysis, we compare clinical and angiographic outcomes between provisional T-stenting and a routine two-stent strategy, using drug-eluting stents, for the treatment of bifurcation stenoses.
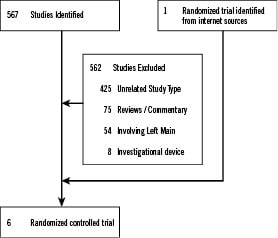
Figure 1. Flowchart of meta-analysis.
Methods
Study objectives and design
The primary aim of the meta-analysis was to compare the outcomes of a one versus two drug-eluting stent strategy for the treatment of bifurcation stenosis in randomised trials. The one stent approach is referred to as the provisional strategy. The outcomes of interest were mortality, myocardial infarction, target lesion revascularisation (TLR), and stent thrombosis defined according to the study protocols. Endpoints were assessed within 1-year of the index percutaneous coronary intervention (PCI). A secondary analysis for restenosis was performed using data from quantitative coronary angiography.
Study search strategy
Using MEDLINE, EMBASE, and the Cochrane Library, we performed searches for possible abstracts using various combinations of the terms “bifurcation” “stent” “provisional” “trial” “drug eluting” in the abstract/title. Two reviewers (S.S.B. and S.K.B.) identified articles eligible for further review by performing a screen of abstracts and titles. If a study was deemed relevant, the manuscript was obtained and reviewed. We also searched conference proceedings from the Scientific Sessions of the American College of Cardiology, American Heart Association, Transcatheter Cardiovascular Therapeutics and of European Society of Cardiology. Websites, including cardiosource.com, TCTMD.com, and escardio.org were also searched for relevant materials. Review articles and prior meta-analysis of the subject were sought. The references of these were reviewed for additional possible studies.
Study identification
We searched through the previously described data sources for possible studies from January 1, 2000 to February 1, 2009. The start date of the search was felt to be appropriate as the first drug-eluting stent was not FDA approved until 2003. The search was not limited to English language literature. We performed text searches for studies that met the following criteria: (1) direct comparison between the provisional and two-stent strategy for the treatment of bifurcation stenosis, (2) reporting of outcomes prior to February 1, 2009, (3) use of a drug-eluting stent, and (4) reporting the rate of restenosis.
Data extraction
We extracted prespecified data elements from each trial, including: study design, stent type, sample characteristics, pharmacologic strategy, sample size, outcome measures, primary endpoint, quantitative coronary angiography data, study duration, and other study characteristics. All outcomes were defined according to the protocol definitions. Two authors (S.S.B. and S.K.B.) independently extracted all trial data (kappa, 0.96). Discrepancies between reviewers were minor and resolved by consensus.
Statistical analysis
Each study was analysed based on the intention to treat principle, except for the trial by Colombo et al which reported analysis based on actual treatment received. The authors of this study were contacted and provided the intention to treat analysis. We performed analysis using both the per-protocol and the intention to treat data for this trial.
From the abstracted data we calculated the relative risk (RR) using the Mantel-Haenszel method for each study outcome to allow for pooling of similar outcomes. The average effects for the outcomes and 95% confidence intervals (95% CI) were obtained using a fixed effects model when heterogeneity was absent or low. To assess heterogeneity of relative risks across trials we used the Cochrane Q statistic (P value≤0.1 was considered significant) and the I-squared statistic. Heterogeneity measured by the I-squared statistic was defined as low, moderate, or high by the following values: 25%, 50%, and 75%, respectively. When the heterogeneity was greater than 50%, a random effects model was used9. When one arm of a study contained no events, we used an adjustment of 0.5. For continuous data, the difference in means (95% CI) was reported. In this analysis, a negative difference in means indicates an advantage for the provisional strategy while a positive value indicates advantage for the two-stent strategy. When the pooled RR was statistically significant we also calculated the absolute risk difference (RD) and 95% CI. A negative RD indicates an advantage for the provisional strategy and a positive RD indicates an advantage for the two-stent strategy. The number needed to treat (NNT) is readily calculated from this measure (1/RD).
Meta-regression using a linear mixed-model was applied to further explore heterogeneity. The restricted maximum likelihood (REML) method was used to estimate the variance components. Covariates considered were key study characteristics such as the crossover rate and quantitative coronary angiography (QCA) data.
Sensitivity analyses were preformed to assess the effects of selected measures of study quality and clinical factors on death, MI, TLR, and stent thrombosis. A funnel plot was used to assess for the presence of publication and other reporting biases by plotting the precision (inverse of the standard error) against the log risk ratio. Using the Begg and Mazumdar rank correlation and Egger’s linear regression method we examined the association between the study size and estimated treatment effects10,11. The Duval and Tweedie non-parametric trim and fill method was used to obtain symmetry in the funnel plot and to determine the impact of hypothetical negative or imputed studies on the pooled estimate12.
The P value threshold for statistical significance was set at 0.05 for effect sizes. Analyses were conducted in Stata 10.0 (Stata Corp., College Station, TX, USA), and Comprehensive Meta-Analysis 2.0 (Biostat, Englewood, NJ, USA). The study was performed in accordance to the recommendations set forth by the Quality of Reporting of Meta-Analysis (QUOROM) work-group13.
Results
Eligible studies
Six randomised controlled trials were identified through the literature search14-19. Each of these trials compared a provisional versus two-stent strategy for the treatment of bifurcation lesions. A total of 1,641 patients were included, with 841 randomised to provisional stenting and 800 randomised to a routine two-stent strategy. Study characteristics are summarised in Table 1 and population characteristics in Table 2.

The sirolimus eluting stent was used in all studies except the BBC ONE trial where a paclitaxel-eluting stent was used. The interventional techniques used in the routine two-stent group were those commonly used in clinical practice such as crush, culotte, and T-stenting. All studies have been published except for the BBC ONE trial which was identified in abstract form. The mean clinical follow-up for the six trials was 10 months (range 6-12 months). Two trials reported outcomes beyond 1-year17,20. Angiographic follow-up and quantitative coronary angiography were performed 6-9 months after the index procedure. The rate of angiographic follow-up was 86%, and similar between treatment strategies. All patients received clopidogrel for at least 6-months, except in the trial by Colombo et al where it was prescribed for at least 3-months.
Mortality
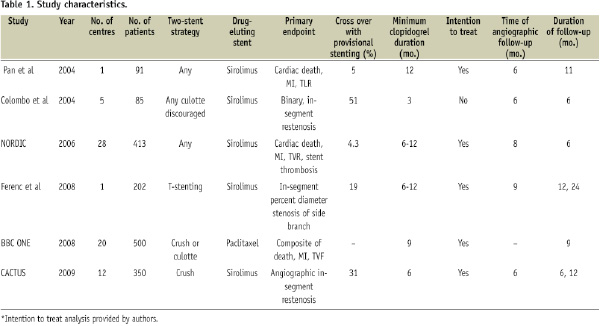
All six trials reported mortality data (Figure 2a).
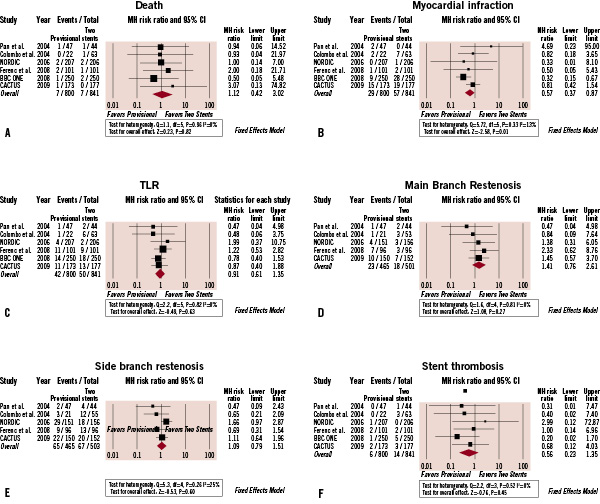
Figure 2. Outcomes from randomised trials. (A) death, (B) myocardial infarction, (C) target lesion revascularisation [TLR], (D) main branch restenosis, (E) side branch restenosis and (F) stent thrombosis. Size of data markers indicates the weight of the study. CI indicates confidence interval. MH indicates Mantel Haenszel.
There were 13 events among the 1,641 patients (0.8%). The incidence in the provisional T-stenting group was 0.9% (7/800) and in the two-stent group was 0.8% (7/841). The corresponding pooled relative risk (95% confidence interval) for the provisional versus two-stent strategy was 1.12 (0.42-3.02), P=0.82, indicating no difference in mortality between the two strategies. There was no evidence of statistical heterogeneity among the studies (P heterogeneity = 0.96).
Myocardial infarction
All six trials reported data on reinfarction from the index PCI (Figure 2b). The RR for MI among five of the six trials favoured the provisional strategy, reaching statistical significance in the BBC ONE trial. In the cumulative analysis, there were 86 events among the 1,641 patients (5.2%). The incidence in the provisional T-stenting group was 3.6% (29/800) and in the two-stent group was 6.8% (57/841); the corresponding pooled RR (95% CI) for the provisional versus two-stent strategy was 0.57 (0.37-0.87), P=0.01. The pooled RD was -3.0%, significantly in favour of the provisional T-stenting strategy (95% CI: -1.0% to -5.0%), P=0.008. The number needed to treat to prevent one MI with the provisional strategy was 33 patients. There was no evidence of statistical heterogeneity among the studies (P heterogeneity = 0.33).
Revascularisation
Data on TLR of the bifurcation stenosis were available from all six trials, except for the BBC ONE trial where target vessel failure was reported (Figure 2c). There was no statistically significant difference between either treatment strategy for TLR in each of the studies. There were 92 events among the 1,641 patients (5.6%). The cumulative incidence in the one stent group was 5.3% (42/800) and 5.9% (50/841) in the two-stent group. The corresponding pooled RR (95% CI) for the provisional versus two-stent strategy was 0.91 (0.61-1.35). There was no evidence of statistical heterogeneity among the studies (P heterogeneity = 0.82).
Main vessel restenosis, measured as binary in-segment restenosis, was reported in five trials (Figure 2d). The rates of restenosis did not significantly differ between the two treatment groups in any trial. The pooled RR (95% CI) for main branch binary restenosis in the provisional versus two-stent strategy was 1.41 (0.76-2.61) without evidence of statistical heterogeneity (P heterogeneity = 0.81).
The rates of side branch binary restenosis were also reported in five trials (Figure 2e). Three trials were non-significantly in favour of the provisional strategy14,15,17. The NORDIC trial was the only study with lower rates of restenosis with the two-stent strategy, a difference that was statistically significant (10.9% vs. 19.2%, P=0.04). In contrast, the rates of restenosis in the provisional and two-stent strategy were similar in the CACTUS trial (14.7% vs. 13.2%). The pooled RR (95% CI) for side branch binary restenosis in the provisional versus two-stent strategy was 1.09 (0.79-1.51) without evidence of statistical heterogeneity (P heterogeneity = 0.26).
Stent thrombosis
Data on stent thrombosis was available from all six trials (Figure 2f). There were 20 events among the 1,641 patients (1.2%). The incidence in the provisional T-stenting group was 0.8% (6/800) and 1.7% (14/841) in the two-stent group. The corresponding RR (95% CI) for the provisional versus two-stent strategy was 0.56 (0.23-1.35). There was no evidence of statistical heterogeneity between studies (P heterogeneity = 0.52).
Quantitative coronary angiography analysis
Quantitative coronary angiography analysis was available from five trials (Table 3).
The reference vessel diameters of the main vessel and side branch were similar between treatment strategies and across trials. The reference vessel diameter of the main vessel ranged from 2.6 to 3.1 mm, and 2.1 to 2.5 mm for the side branch. Moreover, the minimum luminal diameter pre-, post-, and at follow-up, along with percent diameter stenosis for the main vessel and side branch were comparable between treatment groups.
Main vessel restenosis, measured as percent diameter stenosis, was reported in five trials (Figure 3a).
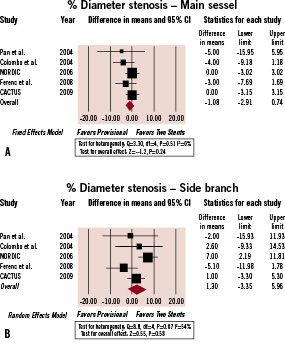
Figure 3. Percent Diameter Stenosis. (A) Percent diameter stenosis of the main vessel, (B) percent diameter stenosis of the side branch. Size of data markers indicates the weight of the study. CI indicates confidence interval. MH indicates Mantel Haenszel.
At follow-up, percent diameter stenosis in the provisional group ranged from 10% to 32% and in the two-stent group from 13% to 25%. The pooled difference in means (95% CI) of the percent diameter stenosis was non-significantly in favour of the provisional strategy, -1.08 (-2.91 to 0.74).
Side branch restenosis, measured as percent diameter stenosis, was reported in five studies (Figure 3b). In the provisional group, percent diameter stenosis ranged from 18% to 31% while in the two-stent strategy it ranged from 19% to 27%. Differences in percent diameter stenosis were only statistically significant in the NORDIC bifurcation study; at angiographic follow-up, the percent diameter stenosis was 31±22 in the provisional group and 24±21 in the two-stent group (P=0.002). The pooled difference in means (95% CI) for the provisional versus two-stent strategy was not statistically different, 1.30 (-3.35 to 5.96). In summary, the QCA data are consistent with the TLR rates which showed no significant difference between the provisional and two-stent strategies.
In meta-regression analysis, we explored whether differences in QCA measures between trials could explain the increased RR for myocardial infarction. The RR for MI across trials was not related to the small differences between studies for the reference vessel diameter (P=0.62), minimum luminal diameter pre intervention (P=0.25), post-intervention (P=0.71), or at follow-up (P=0.68).
Crossover
The crossover from a provisional to a two-stent strategy ranged from 4.3% in the NORDIC bifurcation trial to 51% in the study by Colombo et al. When crossover occurred, the most common strategy employed was T-stenting. The variation between trials in the crossover rates can be attributed to differences in study protocols. The criteria for crossing over from a provisional to two-stent strategy in the NORDIC bifurcation study were very stringent; stenting was only permitted if TIMI flow was zero. In contrast, stenting was mandated for stenosis ≥ 50% in the study by Colombo et al. The crossover rates in the remaining studies were intermediate and more reflective of real world practices. The crossover rate of 31% in the CACTUS trial reflected the more practical criteria for stenting. Side branch stenting was allowed for residual stenosis ≥ 50%, dissection of type B or worse, and TIMI flow ≤ 2. The rate of crossover in the study by Ferenc et al was 19%. In this study, T-stenting of the side branch was performed in cases of flow limiting dissection or residual stenosis of ≥ 75%. In meta-regression analysis, the RR for MI increased with increasing crossover rates; however, this relationship was not statistically significant (P=0.57).
Procedural characteristics
In each trial, final kissing balloon inflation was recommended with a two-stent strategy. This also included those cases where crossover from a provisional to two-stent strategy was necessary. However, final kissing balloon inflation was not routinely recommended in all studies for provisional stenting. Routine final kissing balloon inflation was recommended with the provisional strategy in the CACTUS trial by Ferenc et al and Colombo et al.
Contrast volume and procedural times were available from two and three studies respectively. In the NORDIC bifurcation trial, the provisional stenting group had lower procedural duration (62±51 vs. 76±40 minutes; P<0.0001), fluoroscopy time (15±9 vs. 21±10 minutes; P<0.0001), and contrast volume (233±93 vs. 282±117 mL; P<0.001). Procedural time was also lower with the provisional strategy in the BBC ONE trial, 57 vs. 78 minutes. In contrast, in the study by Ferenc et al, the difference between the provisional and two-stent strategies for procedural duration (51±23 vs. 56±25 minutes; P=0.16), fluoroscopy time (13±7 vs. 15±9 minutes; P=0.20), and contrast volume (204±86 vs. 203±109 mL; P=0.94) did not significantly differ. The differences in procedural characteristics between these studies may relate to the stenting strategy used in the two-stent group. In the NORDIC bifurcation and BBC ONE trials the operator was permitted to use more complex stenting strategies, including the crush and culotte techniques which are generally technically more demanding. In contrast, the recommended two-stent strategy in the study by Ferenc et al was T-stenting which is less technically challenging and likely accounts for the lower procedure times in the two-stent group.
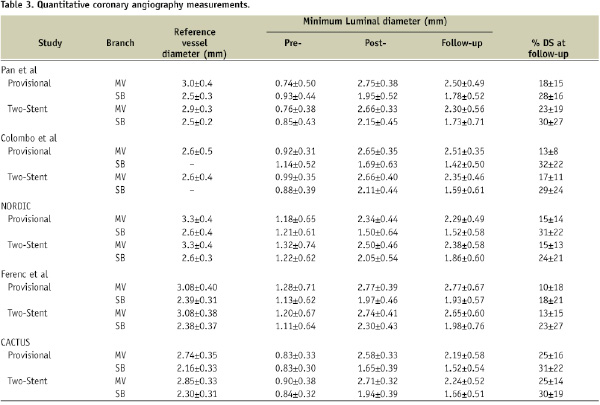
Sensitivity analysis
We examined the robustness of the findings to different assumptions in a sensitivity analysis for mortality, myocardial infarction, TLR, and stent thrombosis (Figure 4).
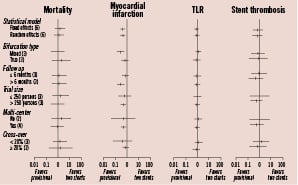
Figure 4. Sensitivity analysis. Estimates are reported as relative risk (95% confidence interval) across key study characteristics.
The overall effect calculated by either a fixed or random effects model yielded similar overall estimates for each endpoint. In stratified analyses across key subgroups, there were no significant differences between either stenting strategy; however, myocardial infarction was less with provisional stenting in each strata, and statistically significant in several. As previously noted, crossover rates differed between studies, primarily driven by differences in trial protocols. However, this did not appear to have a notable impact on the outcomes in the sensitivity analysis. Also, larger trials, multicentre studies, and longer follow-up periods were more likely to show an increase in MI with the two-stent strategy.
The study by Colombo et al reported data according to the actual treatment received. When this trial was analysed by the intention to treat principle, the pooled treatment estimates for death (RR, 0.99; 95% CI, 0.35-2.82), MI (RR, 0.57; 95% CI, 0.35-0.91), and TLR (RR, 0.91; 95% CI, 0.59-1.41) were largely unchanged.
Small study bias
Visual inspection of the funnel plot for TLR did not reveal any asymmetry among studies (Figure 5).
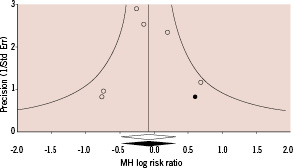
Figure 5. Small study bias. Funnel plot with pseudo 95% confidence limits for assessment of publication bias for target lesion revascularisation. Open circles represent original studies. Solid circles represent hypothetical or imputed studies. Open diamond represent the pooled treatment effect from the original studies. The sold diamond and vertical line represent the pooled treatment effect incorporating the imputed studies.
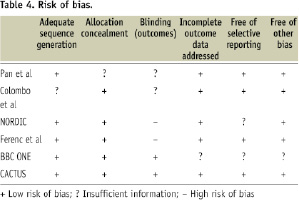
In support, the Begg rank correlation test and Egger’s regression test were not statistically significant, p=0.85 and p=0.86, respectively. The Duval and Tweedie trim and fill method yielded one negative hypothetical study to achieve symmetry in the funnel plot. The inclusion of this imputed study did not significantly change the pooled RR or 95% CI. In aggregate, these findings do not suggest the presence of publication bias. Study quality was appraised using a risk of bias table (Table 4).
Discussion
In this meta-analysis of six randomised trials including 1,641 patients there was no difference in efficacy, measured as TLR or percent diameter stenosis, between provisional T-stenting and a routine two-stent strategy for the treatment of bifurcation lesions. While death and stent thrombosis were similar between the two treatment groups, MI was more common with the two-stent strategy. The relative and absolute reduction in MI with provisional stenting was 43% and 3.0%, respectively (P=0.01). The higher rate of MI with a two-stent strategy is consistent with the results of the individual trials. In five of the six trials identified, there was an excess of MI with a two-stent strategy.
The present results are further supported by the absent or low between trial heterogeneity for death, MI, restenosis, and stent thrombosis, and the consistency of the findings across key study characteristics in sensitivity analyses and meta-regression. Moreover, QCA parameters were similar between treatment groups. In meta-regression analysis, the small between trial differences in reference vessel diameter, minimum luminal diameter pre-intervention, post-intervention or at follow-up did not explain the observed increase in MI.
Efficacy
Among the the six randomised controlled trials, there was no statistically significant difference in rates of restenosis between the provisional and two-stent strategies. Target lesion revascularisation was 5.3% with the provisional strategy and 5.9% with the two-stent strategy (P=0.63). These results are supported by data from quantitative coronary angiography analysis. The percent diameter stenosis in the main vessel or side branch at angiographic follow-up did not significantly differ by treatment strategy (P≥0.24). In sensitivity analysis, the RR for restenosis did not differ across key study characteristics such as: bifurcation type, duration of follow-up, and crossover rates. These data are consistent with an observational study of 477 patients in which provisional T-stenting had a TLR rate of 5.2%21.
Safety
The midterm results from these trials suggest that the provisional and two-stent strategy result in similar rates of death and stent thrombosis, an observation that was consistent across several key study characteristics. However, the rates of MI within 1-year of the index PCI were greater with the two-stent strategy in all trials except Pan et al and statistically significant in the BBC ONE trial. In the pooled analysis, provisional stenting was associated with a relative 43% reduction (P=0.01) and an absolute 3.0% reduction in MI (P=0.008) compared to the two-stent strategy. The treatment of 33 patients with the provisional strategy may prevent one myocardial infarction. While the two-stent strategy used differed between some trials, the rates of MI were lower with the provisional strategy in each study suggesting no specific two-stent strategy could account for the higher MI rate. The simplicity of the provisional T-stenting strategy may yield additional benefits such as shorter procedure times, lower volumes of contrast, and cost savings. In fact, procedural duration was significantly shorter with the provisional strategy in two of the three trials reporting this data16,17,19.
Limited data are available on outcomes beyond 1-year. The NORIDC bifurcation trial and the study by Ferenc et al reported outcomes beyond 1-year. In the NORDIC bifurcation trial, the rates of death, MI, and definite stent thrombosis were similar between the provisional and two-stent strategy at 14 months, 2.4% vs. 1.0%, 2.0% vs. 1.0%, and 1.0% vs. 0.5%, respectively (P=NS)20. In the study by Ferenc et al, the composite of death and MI at 2-years was similar between routine T-stenting and provisional T-stenting groups (P=0.72).
Crossover
Provisional stenting should be regarded as a treatment strategy in which crossover to a two-stent approach is appropriate for a suboptimal result. Registry data suggest that the crossover rate with the provisional stenting strategy in the “real world” is likely closer to that observed in the CACTUS trial and by Ferenc et al, 19% and 31%, respectively. In both single and multicentre registries, the crossover rate has ranged from 22% to 34%21-23. In aggregate, these data suggest that when a provisional stenting strategy is employed, approximately 20-30% of patients will likely crossover to a two-stent strategy. The decision to crossover will be operator dependent but the protocols from the trials included in the current analysis do provide some insight, in particular the CACTUS trial and the study by Ferenc et al. For smaller side branches, the criteria of Ferenc et al seem reasonable and are supported by fractional flow reserve analysis. Frenec et al advocated stenting the side branch for stenosis of >75% severity. In an observational study of 94 jailed side branches with stenosis, no lesion with a stenosis of 50-75% had a FFR ≤ 0.75, suggesting these moderate lesions may not warrant stenting24.
Anatomic variability
Not all bifurcations are suitable for a provisional T-stenting strategy. Long segments of disease in the side branch and acutely angled branches may require a two-stent strategy. Among the various two-stent strategies, including the crush, culotte, and T-stenting, the optimal approach remains undefined. However, the present analysis provides some insight into outcomes between the techniques. In the CACTUS trial, the crush technique was the preferred two-stent strategy whereas in the study by Ferenc et al T-stenting was recommended. The rates of TLR in the two-stent groups of the CACTUS and Ferenc et al trials were similar, 8.9% and 7.3%, respectively. In support, the rates of major adverse cardiovascular events and restenosis were also similar between the culotte and crush techniques in the NORDIC Bifurcation Stent Technique study20. Therefore, currently no particular two-stent strategy appears superior to another and the operator may choose based upon comfort and experience among the various techniques. Dedicated bifurcation stents are under development and investigation; these devices may provide an advantage over both provisional T-stenting and current two-stent strategies25-27.
Economic impact
In the present analysis we observed that a provisional strategy is associated with lower contrast volumes, shorter procedure and fluoroscopy times; in particular, when compared to the more complex two-stent strategies such as the crush and culotte techniques. In addition to these potential benefits, the provisional strategy is also likely to be associated with cost savings. With similar efficacy and improved safety, and taking into consideration the expected 20-30% crossover rate, provisional stenting is likely to yield a cost savings by decreasing the need for additional DES in the treatment of many bifurcation stenoses.
Limitations
Most studies included in the present analysis report mid-term results (up to 12 months) from the index PCI. While two trials reported favourable outcomes beyond one year, the outcomes beyond this time frame, in particular after the discontinuation of clopidogrel, warrant further study. Also, the present study does not directly address the role of a final kissing balloon inflation with the provisional strategy. Bench testing suggests that final kissing balloon inflation may be advantageous by opening the stent struts into the ostium of the side branch, and prevent the stent from deforming in the main vessel28. In each trial, a final kissing balloon inflation was recommended in the group randomised to a two-stent strategy. Routine final kissing balloon inflation was recommended with the provisional strategy in the CACTUS trial, by Ferenc et al, and Colombo et al. While final kissing balloon inflation has been shown to be of value with a two-stent strategy, additional studies addressing whether a final kissing inflation is required after provisional stenting are warranted. Also, left main stenosis was an exclusion criteria in these studies. Accordingly, the optimal approach, a one or two-stent strategy, for the management of left main bifurcations is not addressed in the present analysis.
This meta-analysis was performed at the study level. Availability of individual patient data could improve the reliability of the findings and permit more flexible analyses. However, a major limitation of individual patient data analyses remains the inability to obtain patient level data from all investigators, unpublished studies in particular. Therefore, the selective inclusion of studies in individual patient data meta-analysis can introduce publication and other biases.
Conclusions
In this meta-analysis of randomised trials, the use of a one-stent strategy with provisional T-stenting of the side branch yielded similar rates of restenosis, death, and stent thrombosis up to 1-year from the index PCI compared to a two-stent strategy. However, the rates of MI were significantly lower with the provisional strategy. Therefore, with similar efficacy and superior safety, provisional T-stenting should be considered the primary strategy for the treatment of bifurcation stenoses when anatomically suitable, with crossover to a two-stent strategy when deemed necessary. Longer-term follow-up is necessary to determine the durability of these observations.

