Abstract
Aims: We report a new stenting technique which was employed in 12 patients to treat coronary bifurcation lesions.
Methods and results: A stent is positioned in the main vessel together with a balloon in the side branch, which is positioned slightly proximal to the main vessel stent that also has enough length to cover the side branch ostium. Both the stent in the main vessel and the balloon in the side branch are inflated simultaneously. Following deflation, a double lumen is created in the main vessel, proximal to the bifurcation. The stent balloon is removed with the side branch balloon left deflated in its initial position. The main vessel is rewired with a third guidewire. The side branch balloon and guidewire are removed. The initial guidewire in the main vessel is directed to the side branch. A balloon is advanced and inflated in the side branch to dilate the struts of the main vessel stent that will provide the side branch entrance. The side branch balloon is left in place. A size matched balloon is advanced on the third guidewire that was advanced in the main vessel and inflated inside the stent with high pressure. Finally, kissing balloon inflation is performed at the bifurcation. Provisional stenting of the side branch can be performed when necessary. Final kissing balloon inflation is recommended after stenting of the side branch.
Conclusions: As a new coronary bifurcation stenting method, the Highway Technique has some advantages in side branch protection, with favourable immediate and 30-day clinical outcomes.
Introduction
The treatment of coronary bifurcation lesions is a major challenge for interventional cardiologists. Various techniques have been invented to provide successful immediate results and long term outcomes.1 Reduced restenosis rates with drug eluting stents have increased the confidence to treat bifurcation lesions.2 After the introduction of drug eluting stents, novel techniques were reported with relatively lower restenosis rates.1-3 Nearly all the techniques recommend final kissing balloon inflation at the bifurcation to increase both immediate success and reduce restenosis rates in long term follow-up.4,5 However, there is limited success to achieve this important step in the procedure because there still are difficulties in placing the main vessel stent without jailing the side branch, which further causes difficulties in rewiring the side branch and finalising cases with kissing balloon. We report on a new technique that has the advantage of positioning the main vessel stent by dilating the cell that will provide side branch access before the proximal part of the main vessel stent is apposed. We consecutively treated 12 patients who had bifurcation coronary lesions in varying locations with this technique.
Methods
The Highway Technique is illustrated in Figures 1 and 2.
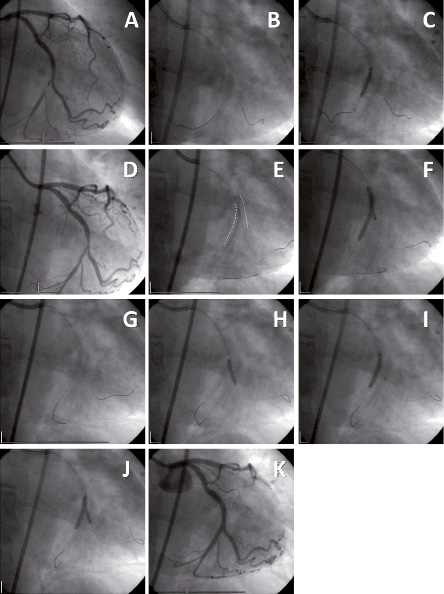
Figure 1. Angiographic images of the Highway Technique.
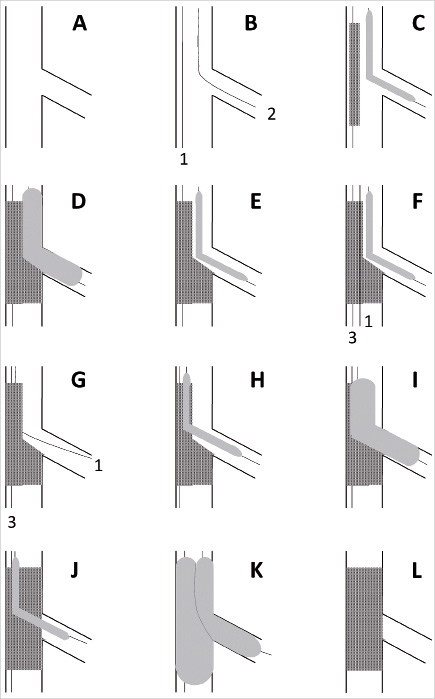
Figure 2. Diagrammatic illustration of stenting using the Highway Technique.
A typical circumflex artery – obtuse marginal branch bifurcation lesion is shown in Figure 1A. Both the main vessel and side branch are wired and alternatively dilated. A balloon 2 mm in diameter is advanced into the side branch and a stent is advanced into the main vessel to fully cover the bifurcation and lesion in the main vessel. The side branch balloon is retracted into the main vessel with its proximal marker protruding 2-3 mm proximally to the main vessel stent (Figure 1E). This proximal positioning (highway) of the side branch balloon is important to prevent jailing of the side branch balloon by the main vessel stent. Both the stent balloon and the side branch balloon are inflated simultaneously with appropriate pressures. Following simultaneous deflation of the balloons, the stent delivery balloon is removed and the side branch balloon is left in place. As a result, the stent is fully apposed to the main vessel wall distal to the bifurcation, whereas a carina and a double lumen is produced by the proximal part of the stent in the main vessel, at the level and proximal part of the bifurcation (Figure 3). A third wire (guidewire number 3) is advanced to the main vessel through the stent lumen, whilst the second lumen is occupied with the side branch balloon (Figure 1G). The side branch balloon and wire (guidewire number 2) are removed. A balloon, matched in size and diameter to the stent, is advanced from guidewire number 3 to the main vessel and positioned distally to the bifurcation. The guidewire number 1 that was in the main vessel is redirected to the side branch through the cell of the stent that is close to the side branch. A 2 or 2.5 mm balloon is advanced to the rewired side branch and inflated in order to dilate the cell that will further provide entrance to the side branch (Figure 1H). Following deflation of the side branch balloon, the balloon that passed through the stent is positioned inside the stent and dilated with high pressure (Figure 1I). A kissing inflation of the main vessel and side branch balloon is performed. This final kissing balloon inflation can be performed after changing the side branch balloon with an appropriate reference diameter matched balloon (Figure 1J). The procedure can continue with a stent implantation in the side branch (provisional side branch stenting). As part of this technique, a final kissing balloon is recommended whether a stent into the side branch is placed or not. Final result shows patency in both the main vessel and side branch (Figure 4).
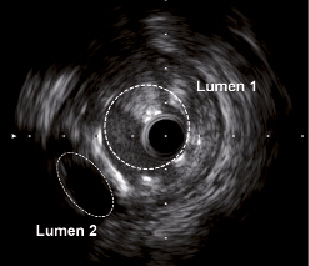
Figure 3. IVUS study demonstrating the second lumen created by the side branch balloon which is inflated simultaneously with the main vessel stent.
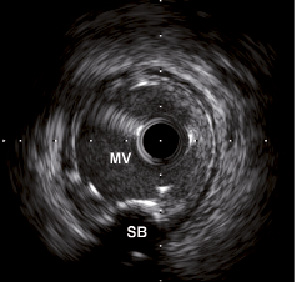
Figure 4. IVUS study demonstrating post-intervention complete ostial coverage of the side branch. (MV: Main vessel, SB: Side branch)
In all cases femoral access was used for the insertion of guiding catheters. The procedures were performed through 8 Fr guiding catheters because of safety concerns.
QCA analysis was performed using Paieon CardiOp-B 3D software for bifurcation lesions (Paeion Inc, New York, NY, USA).
Intravascular ultrasound (IVUS) was performed in selected cases which show complete stent coverage in the ostium after stent implantation and wide patency in the main vessel.
Concomitant medications
All patients received aspirin 100-300 mg and a 300 mg loading dose of clopidogrel prior to the procedure. Clopidogrel 75 mg/day was prescribed to all patients for one year, regardless of drug eluting stent or bare metal stent implantation. During PCI, 10,000 IU of heparin was administered intra-arterially.
Endpoints and definitions
The primary endpoints of our study were to determine procedural success and 30-day major adverse coronary event (MACE) incidence. MACE was defined as death (any cause), non-fatal myocardial infarction (MI) and target lesion revascularisation (either repeat PCI or surgery). Angiographic success was defined as less than 20% of residual stenosis in the main vessel or side branch of the bifurcation. Procedural success was defined as angiographic success without the occurrence of death, MI, emergency surgery or TLR before discharge. MI was defined as the presence or absence of new pathological Q waves on the surface electrocardiogram plus an increase in creatine kinase (CK) more than three times the upper limit of the normal range, with a concomitant increase in its MB isoenzyme. To meet this endpoint criterion, patients who had initially presented with Q-wave MI had to have suffered symptomatic recurrent ST-segment elevation with a rise in CK and/or cardiac troponins and/or angiographic verification of target vessel occlusion. TLR was defined as any repeat PCI or surgery because of restenosis (diameter stenosis ≥50%) within the stent or in the 5 mm distal or proximal segments, associated with symptoms or objective signs of ischaemia. Bifurcation lesions were classified according to the Medina system.6
Twelve consecutive patients with a bifurcation lesion were enrolled for this technique. Patients were included only if their side branch was >2 mm. Cardiac enzymes (creatine kinase, MB sub-fraction and troponin T) were analysed at six hours and 24 hours post-procedure. All patients were discharged after 24 hours post-procedure. A follow-up angiography is planned for these patients at six months. In this report we present the immediate and 30-day results of the patients.
Results
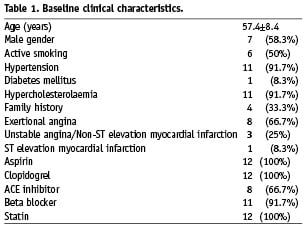
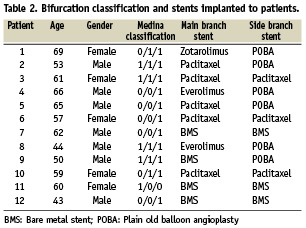
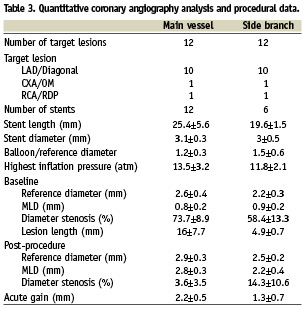
Between February and March 2008, 12 consecutive patients with bifurcation lesions were included. The baseline clinical characteristics are presented in Table 1. The distribution of bifurcation lesions were: 10, left anterior descending artery (LAD)/diagonal; one circumflex artery (CXA)/obtuse marginal (OM) branch and one, right coronary artery/posterior descending artery. Classification of the bifurcation lesions and stents implanted to individual patients are presented in Table 2. Quantitative coronary angiography (QCA) analysis and procedural data are presented in Table 3. The mean reference diameter was 2.6±0.4 mm in the main vessel and 2.2±0.3 in the side branch. The stent length was 25.4±5.6 mm in the main vessel. The highest inflation pressure was 13.5±3.2 atm in the main vessel and 11.8±2.1 atm in the side branch. In all of the cases, the side branch was rewired, and in only six (50%) cases the stent was implanted to the side branch. No difficulty was experienced in advancing the stent to the side branch in any case. All of the cases were finalised with a kissing balloon. Angiographic success was achieved in 100% of patients.
Time to recross the side branch after main vessel stent deployment was 3.5±1.2 minutes and fluoroscopy time for the total procedure was 28.7±9.1 minutes.
The patients’ hospital courses were event-free. Troponin T levels were slightly elevated in two (16.6%) patients during the 24 hours follow-up, however, none of the patients had an increase three times the upper normal limit for CK and its MB isoenzyme. During the 30 day follow-up period none of the patients had MACE. Exercise electrocardiograms were performed in all patients at 30 days and all were free of ischaemia and symptoms.
Discussion
Bifurcation lesions remain a major challenge for the interventional cardiologists. It has many issues to overcome in order to achieve favourable immediate and long term outcomes. In regard for immediate results, the patency of the side branch is a crucial requirement, especially in side branches >2.5 mm in diameter that perfuse a necessary amount of myocardium. Another technical difficulty is the rewiring of the side branch and crossing of stents through the main vessel stent to the side branch. The jailing of the side branch ostium causes further difficulties in long-term follow-up when disease progression occurs in the side branch and an access is needed. Even in the absence of ostial side branch lesion, side branch loss can be observed due to stent jailing or plaque shifting.7-9 When the side branch is <2.5 mm in diameter, occlusion of the side branch might be neglected, whereas in larger side branches patency is of utmost importance. Initial wiring of the side branch is not always protective, and rewiring sometimes can be difficult. Many techniques have been evolved to overcome certain problems, mainly concentrating on good stent coverage of the side branch ostium together with favourable apposition of the main vessel stent. None of the techniques was shown to be superior to the rest.
Actually, routine usage of two stents does not offer clinical advantages as compared to provisional use of two stents.2,10,11 However, in the presence of a large side branch with severe lesions, two stent intended strategies should be considered. In case of sharp angles, provisional T stenting has the disadvantage to cover the ostium adequately. Therefore, techniques such as crush or cullotte might be considered as alternative methods, which on the other hand create important risks for stent thrombosis by creating double or triple stent struts.12 TAP stenting, which is a recent technique, provides some additional benefits over crush stenting with full ostial coverage and lesser stent struts.13 Our technique gives the opportunity to continue with TAP stenting when a second stent is needed for the side branch. Therefore, the operator has the opportunity to decide during the procedure if the result for the side branch is not appropriate with balloon dilatation only. Complete ostial coverage is a crucial issue and by using our technique the operator has the ability to decide whether to use provisional T stenting or TAP stenting according to the angle of the side branch.
In the past few years, crush stenting has provided ease in managing bifurcation lesions whereas high restenosis rates have raised the necessity of a final kissing balloon.5,14 It is shown that success in rewiring the side branch and performing a final kissing balloon could not be possible in all cases. Also, treating bifurcation lesions with a single stent in the main vessel was reported to be superior to stenting both the main vessel and side branch.11 Therefore, provisional stenting of the side branch is recommended. Our technique provides a unique method to protect the side branch. By creating a double lumen at the level of the side branch ostium after stenting the main vessel and inflating a balloon at the side branch with the balloon protruding into the main vessel, the side branch ostium remains open. Rewiring of the side branch through the main vessel stent and crossing a balloon through the stent struts provides opening of the struts that will appose to the side branch ostium. This step is the most important part of our technique, which protects the side branch ostium from jailing and makes the further steps easier in treating the side branch. Another advantage, is the ability to conclude the procedure with a single stent implantation in the main vessel, leaving the side branch stentless. The open strut in front of the side branch ostium also provides easy access for stent delivery as compared to provisional side branch stenting. In addition, the operator has the chance to change the technique in any step, especially when there is difficulty in crossing the balloon through the struts of the main vessel stent to the side branch.
Although rewiring of the main vessel seems to be a difficult step, giving a U-shape to the tip of the guidewire provides easy access through the under-inflated main vessel stent. In addition, the second lumen to the side branch is occupied by the side branch balloon, that also assists the rewiring of the main vessel. With this technique we had 100% success without passing the new wire behind the proximal struts. In all cases an appropriately sized balloon easily passed through the re-wired main vessel stent, therefore we did not need IVUS confirmation. However, in case of difficulty passing the balloon through the main vessel, IVUS confirmation could be considered to check whether the guidewire is in correct position or has passed through the struts of the main vessel stent.
The Highway Technique is suitable for all bifurcation lesions except for Medina 0/0/1, which only involves a side branch. This strategy is based on main vessel stenting and providing easy access to the side branch. In order not to induce restenosis in a healthy main vessel, alternative techniques might be used for Medina 0/0/1 bifurcation lesions.
Increase of cardiac enzymes three times the upper normal limit is an important predictor of prognosis after PCI.15 Cardiac enzymes are expected to increase in cases where repeated inflations are performed. In our experience, the course of the cardiac enzymes was within normal limits and none of the patients had an increased CK level three times above the upper normal limit.
The intended inflation of the side branch safety balloon could be a potential risk for restenosis in a healthy uninvolved side branch. This might be a relative disadvantage of this strategy in bifurcation lesions with uninvolved side branches. We will be able to discuss this issue when angiographic follow-up data will to be available.
Although immediate and 30-day outcomes are favourable, the value of this technique will be validated when angiographic follow-up results would be available at six months.

