Abstract
Aims: Isolated, high-grade coronary bifurcation lesions located at the side branch (SB) ostium (Medina type 0,0,1) are uncommon and their specific treatment has not been described.
Methods and results: We have developed an “inverted” technique for the treatment of these lesions, derived from the usual provisional T stenting. We implant the stent from the proximal main branch through the SB, with reopening of the strut through the distal main branch (DMB) and systematic final kissing balloon. We retrospectively reviewed results in 40 patients. The procedural success was 100%, no failure was observed to rewire the DMB or perform the kissing balloon, and a second sent was implanted in the DMB in only three patients (7.5%). No death, myocardial infarction, stent thrombosis or repeat revascularisation occurred within the first 30 days of follow-up. At a mean of 22±14 months, three patients underwent repeat percutaneous coronary intervention (7.5%), with target lesion restenosis (n=2; 5%), other vessel treated (n=1, 2.5%), target lesion revascularisation (n=1; 2.5%), and target vessel revascularisation (n=1, 2.5%).
Conclusions: The “inverted” provisional T stenting technique was safe and highly effective in the management of Medina 0,0,1 coronary bifurcation lesions. Larger trials are needed before its routine application can be recommended.
Introduction
Provisional stenting is the preferred management technique for coronary bifurcation lesions1. The Medina 0,0,1 type2,3 represents <5% of lesions described in published reports,4,5 and is usually excluded from studies of coronary artery stenting2,6,7. This subset of lesions, particularly when Y shaped, is not amenable to standard stenting techniques. Provisional T stenting is a safe and effective technique, associated with favourable short- and long-term procedural outcomes, which have further improved with the availability of drug-eluting stents8. This has long been our technique of choice for the stenting of all coronary artery bifurcation lesions. Medina 0,0,1, are usually managed medically because of the absence of reliable endovascular techniques. However, when the latter fails, we use a technique that aims at achieving complete ostial coverage with minimal main vessel injury. This “inverted” T stenting approach consists of covering the lesion with a stent from a proximal main vessel (PMV)-to-side branch (SB) direction, followed by kissing balloon manoeuvre to open the strut through the distal main branch (DMB). We are unaware of other reports of the immediate and long-term results of this technique, used for this specific type of lesion.
The aim of this study was to evaluate the technical feasibility, safety and short- and long-term procedural and clinical results achieved with “inverted” provisional T stenting for Medina 0,0,1 coronary bifurcation lesions.
Patient population and methods
We retrospectively included in this study consecutive patients treated at our medical centre, using our Cardioreport® and Medireport® databases of 5,001 patients treated by percutaneous coronary interventions (PCI) performed between December 2004 and August 2008. All coronary angiograms and PCI reports were reviewed by two experienced interventional cardiologists, to verify that the type of bifurcation lesions and procedural techniques corresponded the criteria of inclusion in our study. The various bifurcating branches were classified according to Medina et al1 (Figure 1). SB was the branch with the smallest, visually estimated reference diameter in its most proximal, non-diseased segment, and DMB was the largest branch. For example, a patient with an ostial lesion of a first diagonal branch with a reference diameter larger than the mid left anterior descending (LAD) artery was not included in our study.
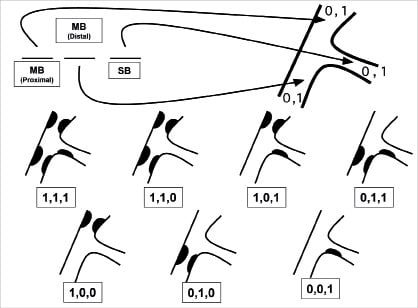
Figure 1. Medina classification of coronary bifurcations. PMB: proximal main branch; DMB: distal main branch; SB: side branch
Procedural success was defined as a) < 30% in-stent residual stenosis, b) < 30% residual stenosis outside the stented segment (i.e., the ostium of the DMB), c) TIMI 3 flow in both branches, and d) no in-hospital major adverse clinical event (MACE), defined as death, myocardial infarction (MI), any repeat revascularisation, stent thrombosis, or haemorrhage requiring a transfusion. MI was defined as an increase in plasma creatine kinase to ≥ twice the upper normal limit. Target lesion revascularisation (TLR) was defined as repeat revascularisation by PCI or coronary artery bypass graft (CABG) surgery of the in-stent segment, or 5 mm proximal or distal to the stent, including the proximal segment of the DMB. Target vessel revascularisation was defined as repeat revascularisation of the target vessel by PCI or CABG. Cardiac or non-cardiac deaths, Q- or non-Q-wave MI, target lesion or vessel revascularisation, CABG, progression of disease in another vessel, restenosis or stent thrombosis occurring during follow-up were ascertained by telephone communications with the patients. Since this was a retrospective study, coronary angiograms were not systematically scheduled during follow-up.
The “inverted” provisional T stenting technique
The main steps followed during an “inverted” provisional T stenting procedure are shown in Figure 2. After the insertion of two 0.014” wires: one in the DMB (recommended) and one in the SB, the diseased vessel is predilated, if appropriate, and a stent is implanted from the proximal main vessel to the side-branch, over the side branch 0.014” wire. The second wire is left in the distal main vessel and jailed. Next, the SB wire is advanced distally through the mesh of the stent from the proximal main vessel to the DMB. A kissing balloon inflation is systematically performed to open the strut at the diameter of the main vessel and without deformation of the stent at the SB ostium. If a satisfactory result is achieved, the procedure is stopped. To optimise our results, we routinely use StentBoost (Philips Medical Systems, Nederland BV, Best, The Netherlands), an angiographic tool developed to detect the presence of inadequate stent expansion9 (Figure 3). A second stent is inserted in the distal main vessel only when a satisfactory result is not achieved after kissing balloon. Figure 4 illustrates the final procedural outcome.
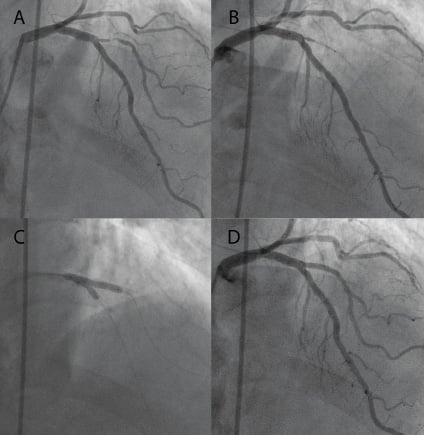
Figure 2.“Inverted” provisional T stenting procedure. A) Baseline lesion of the first diagonal branch without significant involvement of the LAD; B) Placement of the stent from the proximal LAD through first diagonal branch; C) Kissing balloon; D) Final result.
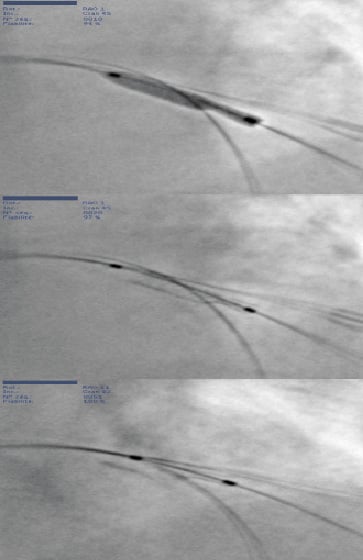
Figure 3. Image enhancement of a stent by StentBoost for a Medina type 0,0,1 bifurcation lesion. Top panel: during stent inflation; middle panel: after deflation of the stent balloon; bottom panel: after kissing balloon. Note the compliance of the Taxus Liberté™ placitaxel-eluting stent which compensates for the different sizes of the DMB and SB.
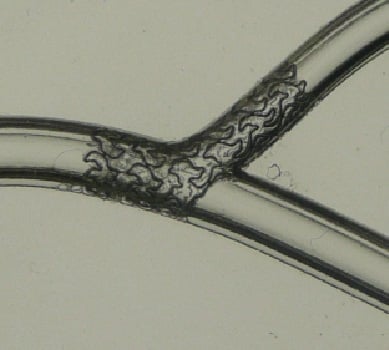
Figure 4. Bench testing of a Taxus Liberte™ stent after provisional T stenting and kissing balloon for the treatment of a Medina 0,0,1 type lesion. Final position, note that this allows a total ostial coverage.
Stenting procedure
According to the protocol routinely implemented for PCI in our centre, all patients received oral aspirin, 75 to 160 mg daily, and a 600-mg bolus of clopidogrel at least 12 hours before PCI. A bolus of unfractionated heparin, 50 IU/kg, i.v., was administered at the onset of the procedure, supplemented by a 2000-IU bolus for procedures lasting > 1 hour.
Using a Philips Medical System device, quantitative coronary analysis was performed on the selected cases pre- and postprocedure.
Statistical analysis
The data are expressed a means ±SD (range) or, when appropriate as numbers and percentages of observations.
Results
Study population
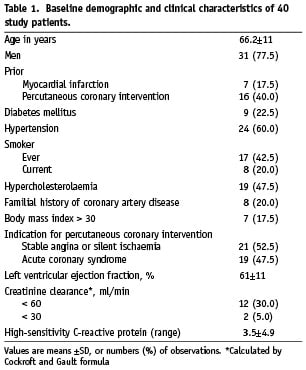
The study population comprised 31 men and nine women, whose mean age was 66.2±11 years. Their clinical characteristics, coronary risk factors and results of preprocedural laboratory tests are summarised in Table 1. These characteristics are similar to those usually observed. Coronary artery disease was diffuse in 32.5% of patients, and 40% had undergone previous PCI.
Angiographic observations
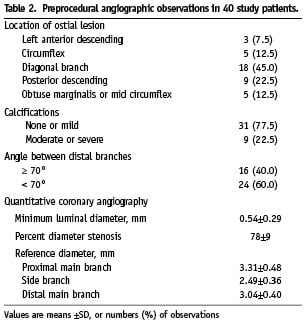
The target Medina 0,0,1 lesions were located at the ostium of 1) diagonal branches in 18 patients (45%), 2) the posterior descending artery in nine (22.5%), 3) left circumflex in five (12.5%), 4) left marginal branches in five (12.5%), and 5) left anterior descending artery in three (7.5%) patients (Table 2). Single-vessel disease was present in nine patients, 18 had 2-vessel and 13 patients had 3-vessel disease. Additional angiographic characteristics are shown in Table 2.
Procedural observations
The main procedural characteristics are shown in Table 3. Diagnostic angiography and PCI were performed in a single procedure in six patients, while the 34 remaining patients underwent planned PCI. The radial vascular access was used in 17 (42.5%) and the femoral access in 23 (57.5%) patients. We decided to implant drug-eluting stents (DES) in 37, and bare metal stents (BMS) in three patients. All procedures but one were performed using a 6 Fr guiding catheter, while in one procedure we used a 7 Fr guiding catheter. No patient received preprocedural treatment with a glycoprotein IIb/IIIa inhibitor.
All patients underwent “inverted” provisional T stenting with final kissing balloon manoeuvre, and 16 lesions were predilated, of which three were treated with rotational atherectomy. Placement of the stent from the PMB to SB, and rewiring of the DMB was successful in all patients. Dissections occurred in three patients (7.5%), of whom two had received paclitaxel-eluting (PES) and one had received an everolimus-eluting stent. Moderate (n=1), or severe (n=2) calcifications were present at the bifurcation in all three patients. One additional PES and one everolimus-eluting stent were each placed in the DMB of two of these three patients<, and an additional Coroflex® Blue PMS (B Braun, Melsungen AG, Melsungen, Germany) was placed in the third patient. Ultimately, 92.5% of the procedures were completed with a single stent and kissing balloon in the bifurcation lesion. Since other lesions were treated during the index procedure in 26 patients, a mean of 2.15 stents per patient were implanted.
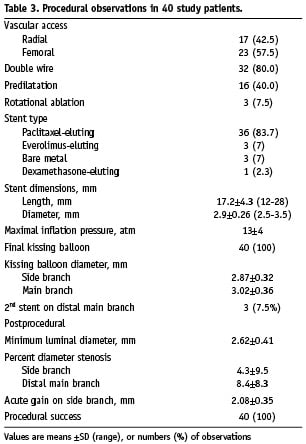
The procedural success was 100%. There was no major complication and five minor intraprocedural complications, including three type A or B dissections after kissing balloon (managed without additional stenting), one dissection at the distal edge of a stent placed in a diagonal branch, (managed by implantation of an additional stent) and a mild guide wire-induced distal extravasation of contrast material, which resolved spontaneously during the procedure.
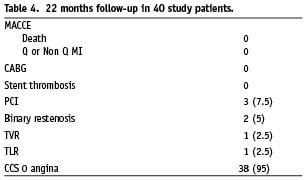
In hospital and 30 days clinical outcomes
No death, MI, repeat PCI, stent thrombosis or haemorrhagic complication occurred before discharge of the patients from the hospital. A slight postprocedural increase in serum troponin concentration was observed in nine patients, without associated rise in serum creatine kinase above the upper normal limit. The patients were discharged from the hospital at a mean of 1.2±0.7 days after PCI. They were advised to continue treatment with aspirin, 75 to 160 mg/day, indefinitely, and clopidogrel for at least for six months after implantation of a DES, or one month after implantation of a BMS. During a follow-up of 30 days, no MACE occurred and no patient discontinued dual antiplatelet therapy. At a mean follow-up of 22 months (Table 4), we observed no death, no Q or non-Q MI, no stent thrombosis. A repeat PCI was required in three cases, on target bifurcation lesion in one, TLR 2.5%, on treated vessel in one, TVR 2.5%, and angiogram showed a significant non treated DMB lesion (binary restenosis 5%). At follow-up, 38 patients were angina-free (95%).
Discussion
The optimal management of coronary bifurcation lesions remains both challenging and the object of considerable debate. The heterogeneity of several characteristics, including lesion size and location, amount of calcification, and angulation between arterial branches on the one hand, and the variable experience among interventional cardiology centres on the other hand, complicates the interpretation and comparison of published studies. The preferred strategy for the treatment of Medina 0,0,1 lesions is also debated10. A risk of injury to the main vessel when treating the side branch exists with all PCI techniques, and treatment decisions must be made on a case-by-case basis, depending on the patient’s clinical presentation. Optimal medical therapy remains the preferred first-line treatment, particularly for single-vessel coronary artery disease and in presence of stable angina, while CABG should be systematically considered for 3-vessel disease.
The placement of a single stent in the ostium has been suggested for ostial SB lesions. Several techniques, including predilation or atherectomy, placement of a non-inflated balloon in the main vessel8,11 or the Szabo technique12, which consists of passing the proximal end of a second guide wire through the last cell to anchor the stent, have been described to enhance the accuracy of the stent placement. The main advantage of an ostial stent is the avoidance of its placement in a vessel that is not significantly narrowed on angiographic examination. However, despite the use of these techniques, the accurate placement of a SB stent at the ostium remains challenging, particularly when the angle between the DMB and the SB is < 90°, with a potential risk of placement of the stent too distally, leaving a gap in the scaffolding and drug delivery to the proximal SB, or too proximally, leaving the proximal struts protruding into the main vessel.
The “inverted” provisional T stenting technique, with placement of the stent from the PMB into the SB, offers the advantage of complete coverage of the ostium. The main challenges encountered with this technique are the achievements of 1) complete apposition of the stent despite different diameters of PMB and SB, and 2) an optimal opening of the strut in front of the DMB. The systematic kissing balloon manoeuvre helps overcome these hurdles. However, it has been argued that the kissing balloon manoeuvre creates lesions in the endothelium that might cause the development of restenosis. The stent boost acquisition helped us to confirm if the stent was well opened in several cases. In the study of Mishell9, IVUS and stent boost demonstrated a small difference in minimum stent diameter, 0.043 mm (95% CI: 0.146-0.061 mm), so we decided to examine all our stents with this tool to evaluate quality of stent expansion, but not malapposition.
This first study specifically examined the feasibility and safety of “inverted” provisional T stenting for isolated ostial SB bifurcation lesions and was associated with a 100% procedural success. This is in part due to our over 13 years extensive experience in using the provisional T stenting strategy13. Despite reopening the strut in a large artery with systematic kissing balloon, an additional stent in the DMB was needed in only 7.5% of patients, a percentage similar to best results reported with provisional T stenting2,4, and better than in others studies, which included or excluded Medina type 0,0,1 bifurcation lesions4,6,14,15. The short-term safety of this technique was confirmed by the absence of MACE up to 30 days of follow-up and also for long-term evolution.
DES and BMS have not been compared in a randomised trial for the treatment of bifurcation lesions, which remain an “off-label” indication for the use of DES. However, bifurcation lesions are among the predictors of restenosis and, in post hoc subgroup analyses, DES decreased the restenosis rate in bifurcation lesions15. Therefore, we routinely use DES for bifurcation lesions, except in individual cases, when we judge the risk to be higher than the expected benefit. Furthermore, in the specific case of “inverted” provisional T stenting, when a large myocardial area is exposed to a risk of restenosis, we believe that DES are the stents of first choice.
The type of implanted platform is important, in relation to its mechanical properties. A randomised trial comparing SES with PES in the treatment of bifurcation lesions found significantly lower rates of restenosis and TLR with SES16, results that were consistent with other studies of non-bifurcated lesions17. But as seen on the bench, conformability of the TAXUS™ Liberte™ PES (Boston Scientific, Natick, MA, USA) appears to be highly better than others. These observations, lead us to exclusively use the TAXUS™ Express 2™ and TAXUS™ Liberte™ PES (Boston Scientific, Natick, MA, USA) because of 1) the larger strut opening achieved after kissing balloon demonstrated in bench testing18,19, an essential element in the specific setting of Medina 0,0,1 bifurcation lesions, and 2) the closer apposition of the stent theoretically offered by the higher compliance of PES. Several dedicated stents are being studied in the hope of improving the results of PCI for bifurcation lesions7,20,22. These systems, however, will probably not be of much assistance in the management of Medina 0,0,1 lesions.
Limitations of our study
Our study included a small number of patients, in part because these lesions and their management by PCI are both uncommon. The retrospective design and lack of a control group are additional limitations of this study. The absence of systematic angiographic follow-up might have underestimated the rates of restenosis. Finally, it is possible that preprocedural symptoms could not be attributed to side branch lesion and/or postprocedural absence of symptoms could be attributed to treatment of non-study lesions.
Conclusions
This study is the first to focus on PCI for the treatment of Medina type 0,0,1 bifurcation lesions. Our adaptation of the provisional T stenting technique, by implantation of a stent from the PMB to the SB and systematic kissing balloon manoeuvre in 40 patients, was associated with a 100% procedural success. This allowed us to achieve a successful procedure with implantation of a single stent in 92.5% of the cases. The absence of MACE at 30 days confirmed the high short-term safety of this technique. This was associated with a very low TLR rate of 2.5% and an acceptable reintervention rate of 5%. However, this procedure should be used only after unsuccessful optimal medical therapy. These encouraging results need to be verified by larger trials over longer periods of observation.

