Abstract
Aims: The optimal strategy for patients with isolated ostial bifurcation lesions has not yet been determined. We propose the modified flower petal technique for the treatment of Medina type 0,0,1 or 0,1,0 coronary bifurcation lesions.
Methods and results: We selected 64 patients who had Medina type 0,0,1 or 0,1,0 coronary bifurcation lesions. Percutaneous coronary intervention (PCI) was performed with the modified flower petal technique in all patients. After PCI, all patients were followed up to nine months after the intervention. Quantitative coronary angiography (QCA) analyses were performed for both the main and the side branch at baseline, after the stent implantation and at nine-month follow-up. Twenty patients (31.2%) had ostial left anterior descending artery lesions, nine patients (14.1%) had ostial circumflex artery lesions and the other patients had isolated ostial non-left main bifurcation lesions. The procedural success rate was 100%. There was no death, myocardial infarction, subacute or late stent thrombosis at nine-month follow-up. In one patient, in-stent restenosis requiring reintervention was noted.
Conclusions: The modified flower petal technique has excellent acute results and midterm clinical outcomes in the management of Medina type 0,0,1 or 0,1,0 coronary bifurcation lesions.
Introduction
Isolated ostial bifurcation lesions (Medina type 0,0,1 or 0,1,0) represent <20% of coronary bifurcation lesions1,2. Percutaneous coronary intervention (PCI) of this subset of lesions is challenging for the interventional cardiologist because of the technical difficulty and potential risk of serious complications3. Stenting of such lesions may result in incomplete coverage of the ostial lesion or protrusion of the proximal stent margin into the adjacent vessel. Furthermore, potential plaque or carina shift during PCI may compromise the adjacent vessel3,4.
The optimal strategy for patients with isolated ostial bifurcation lesions has not yet been determined. Furthermore, Medina 0,0,1 lesions are usually managed medically because of the absence of reliable percutaneous treatment techniques3,5. Recently, we devised a new technique, called the modified flower petal technique, for the treatment of Medina type 1,1,1 coronary bifurcation lesions6, derived from flower petal stenting which was first defined by Kinoshita et al7. The most important characteristics of this technique are complete coverage of the side branch ostium by stent struts and a lower metallic burden at the carina region6. The aim of this study was to evaluate the technical feasibility, safety and short-term and midterm procedural and clinical results achieved with the modified flower petal technique for Medina type 0,0,1 or 0,1,0 coronary bifurcation lesions.
Methods
PATIENT SELECTION
Between April 2011 and June 2012, we included 64 patients (41 male, 23 female; mean age 60.0±11.2 years) who had Medina type 0,0,1 or 0,1,0 coronary bifurcation lesions. The vessel size had to be ≥2.5 mm by visual estimation on coronary angiography. Patients with acute myocardial infarction (MI), in-stent restenotic lesions, heavily calcified lesions, severe proximal tortuosity, chronic total occlusion, cardiogenic shock or contraindications to prolonged use of antiplatelet agents were excluded. The local ethics committee approved the study.
Treatment options were fully discussed with the patient, and written informed consent for both the PCI procedure and participation in the study was obtained from all patients. All of the patients were brought back for angiography at nine months, which was considered to be part of the study method.
PROCEDURE
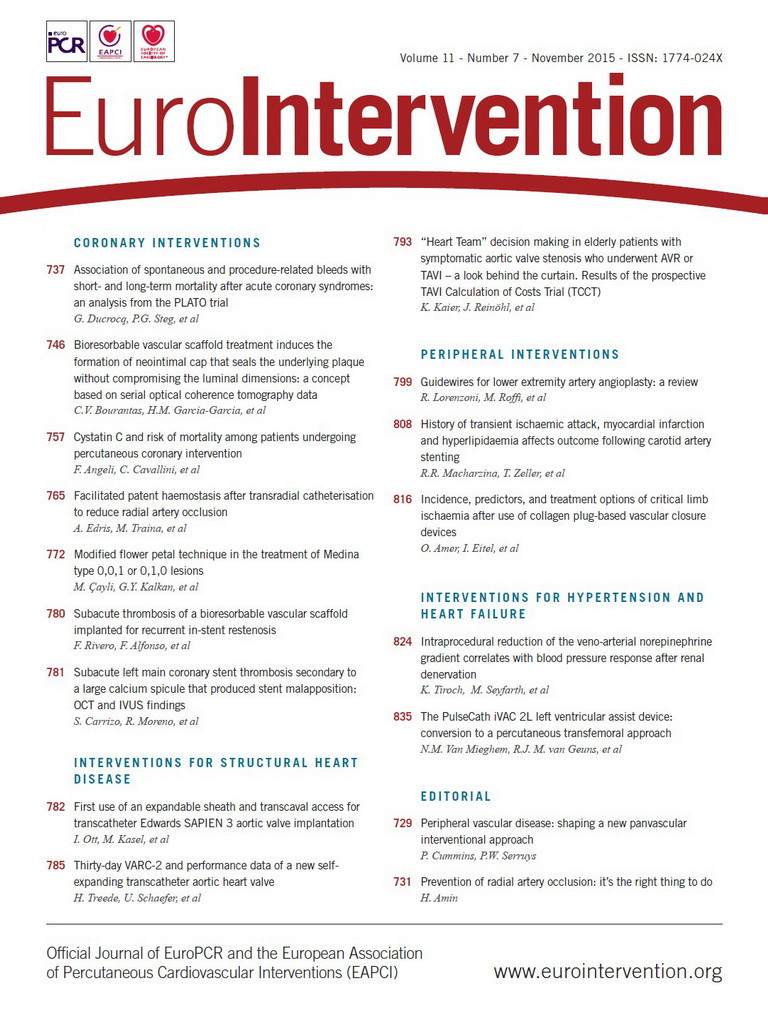
Previously, we have described the steps of this technique for the treatment of Medina 1,1,1 lesions6. The most important difference for Medina 0,0,1 or 0,1,0 is that a second stent was not implanted. The steps of this technique for Medina 0,1,0 or 0,0,1 lesions are illustrated in Figure 1 and Figure 2. A large (7 or 8 Fr) and strong back-up support guiding catheter must be selected for this technique. The procedure starts with wiring of both branches (the first wire into the target branch and second wire into the other branch as an anchor wire). A stent-balloon system is prepared outside of the guiding catheter. First, the plastic stent cover is pulled back slightly to expose the final proximal stent strut (Figure 1A), and the stent delivery system balloon is inflated to 5-6 atmospheres and deflated (Figure 1B). Then, the proximal end of the anchor wire is passed through the final proximal stent strut (Figure 1C). Another balloon is loaded on the anchor wire as an anchor balloon. Proximal markers of stent and balloon are aligned. Then the final proximal strut of the stent is re-crimped by hand (Figure 1D). In this article, one of the most important differences from our previous definition is the location of alignment of the stent and anchor balloon. The anchor balloon was centred on the last proximal stent strut in the previous article, whereas the proximal markers of the stent and the anchor balloon are positioned in the same line in this article. Thus, the stent-balloon system becomes more flexible and allows easy advancement of the stent or balloon into high take-off vessels.
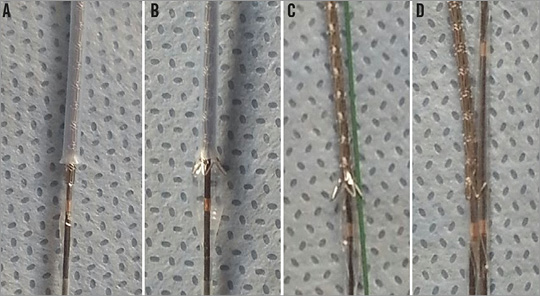
Figure 1. Preparation of the stent-balloon system. A) The plastic stent cover is pulled back slightly to expose the final proximal stent strut. B) The stent delivery system balloon is inflated to 5-6 atmospheres and deflated. C) The proximal end of the second wire is passed through the final proximal stent strut. D) Another balloon is loaded onto the second wire as an anchor balloon. The proximal markers of the stent and balloon are aligned. Then, the final proximal strut of the stent is re-crimped by hand.
The prepared stent-balloon system is advanced through the guiding catheter to the target lesion until the anchor balloon stops the advancement of the stent (Figure 2A). In this way, the anchor balloon can prevent excessive stent advancement into the target branch and provide complete coverage of the lesion by the stent struts. First, the stent balloon is inflated and deflated (Figure 2B). Second, the anchor balloon is inflated and deflated (Figure 2C). Then, the stent balloon is inflated again (Figure 2D). Thus, the protruding final proximal strut is in contact with the opposite side of the adjacent vessel wall (Figure 2E). The most important characteristics of this technique are complete coverage of the ostial bifurcation lesion by stent struts without protruding into the adjacent vessel, and a lower metallic burden at the carina region (Figure 3, Figure 4, Figure 5).
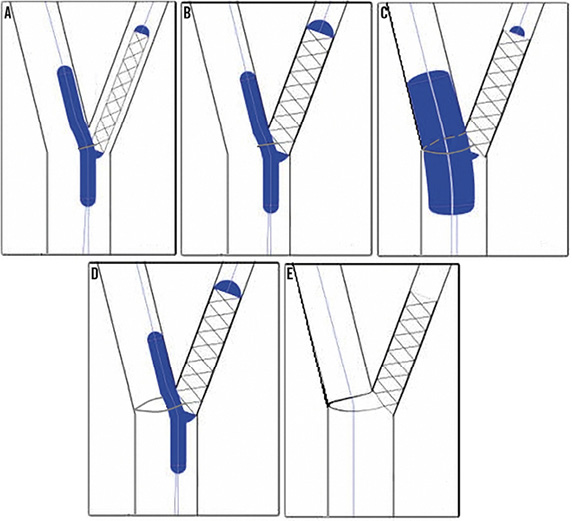
Figure 2. Schematic model presentation of the new technique. A) The prepared stent-balloon system is advanced through the guiding catheter to the lesion location until the anchor balloon stops the advancement of the stent. B) The stent balloon is inflated and deflated. C) The anchor balloon is inflated and deflated. D) The stent balloon is inflated again. E) The protruding final proximal strut comes into contact with the opposite side of the adjacent vessel wall.
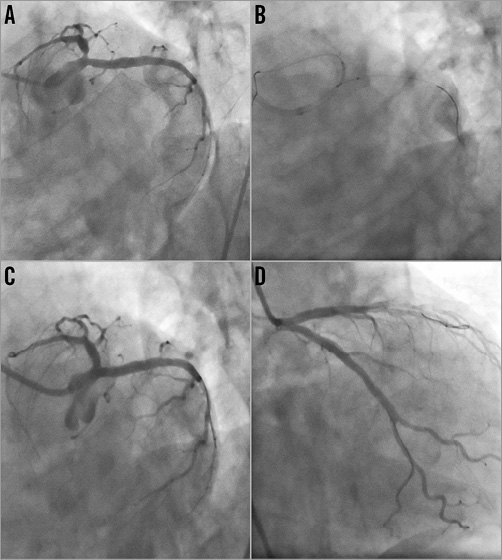
Figure 3. Stenting of isolated LAD ostial lesion with the modified flower petal technique. A) LAD ostial lesion viewed in LAO-CAU projection. B) Positioning of the stent. C & D) Angiographic results after stent implantation.
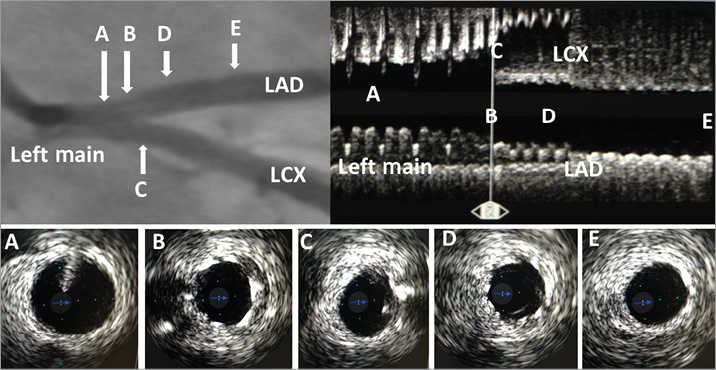
Figure 4. Angiographic image and IVUS findings after stenting of an isolated LAD ostial lesion with the modified flower petal technique. A) Cross-sectional intravascular image of the distal left main coronary artery. B) Cross-sectional intravascular image at the level of the carina shows complete coverage of the ostial lesion by the stent struts. After the procedure, the carina had a good position, without shifting to the LCX. C) Cross-sectional intravascular image of the LCX ostium. There was no plaque or carina shift into the LCX. D) Cross-sectional intravascular image shows well-apposed stent struts at the LAD proximal segment. E) Cross-sectional intravascular image of the LAD, just distal to the stenting area. LAD: left anterior descending artery; LCX: left circumflex artery
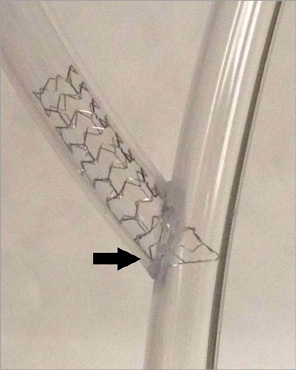
Figure 5. Bench testing of the modified flower petal technique for the treatment of an isolated ostial bifurcation lesion. The final position shows complete coverage of the ostial lesion by stent struts and minimal metallic burden at the carina region. There is no breakage or deformation on the stent.
PREPARATIONS AND FOLLOW-UP
All patients were pre-treated with aspirin 300 mg and clopidogrel 300 mg loading dose, followed by 75 mg daily, at least one day prior to the index procedure. During the procedure, an intra-arterial bolus of unfractionated heparin was administered at a dosage of 70 U/kg. All procedures were performed by using zotarolimus-eluting stents (Endeavor® Resolute; Medtronic, Minneapolis, MN, USA), sirolimus-eluting stents (Coracto™; Alvimedica, Istanbul, Turkey), paclitaxel-eluting stents (Coraxel; Alvimedica) and everolimus-eluting stents (XIENCE V®; Abbott Vascular, Santa Clara, CA, USA). After the procedures, all patients were advised to stay on dual antiplatelet therapy for at least one year. All patients were followed up to nine months after the intervention. All patients adhered to dual antiplatelet therapy during the study period.
DEFINITIONS AND CLINICAL ENDPOINTS
Procedural success was defined as successful implantation of the stent into the target lesion, causing a final residual stenosis ≤30%. Major adverse cardiac events were defined as cardiac death, MI and target lesion revascularisation (TLR). TLR was defined as a repeat revascularisation with a stenosis ≥50% within the stent or in 5 mm proximal or distal segments adjacent to the stent. Stent thrombosis was defined as any of the following: angiographic demonstration of stent closure or intra-stent thrombosis, unexplained sudden death, or MI without concomitant documentation of a patent stent.
QUANTITATIVE CORONARY ANGIOGRAPHY (QCA) ANALYSIS
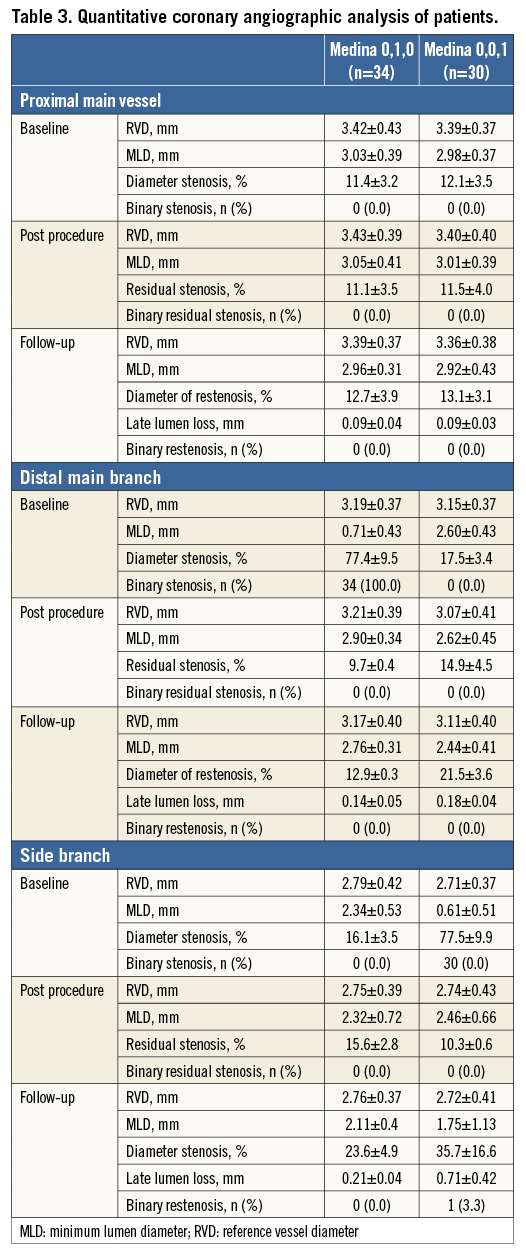
Quantitative coronary angiography analyses were performed at baseline, after stent implantation and at nine-month follow-up using dedicated bifurcation angiographic software (CardiOp-B system version 2.1.0.151; Paieon Medical, Ltd., Rosh Ha’ayin, Israel)8,9. All analyses were performed in consensus by two experienced interventional cardiologists (M. Gür and Z. Elbasan) who were blinded to patient characteristics. QCA of each bifurcation lesion was obtained in three segments: the proximal main vessel, distal main branch and the side branch. For quantitative analysis, at least two orthogonal projections were obtained, and the angiographic frames with homogeneous contrast filling of the segment of interest were selected in a view offering good opening of the bifurcation. According to the algorithm in the dedicated software, reference vessel diameter, minimal lumen diameter (MLD) and diameter stenosis (DS) were measured in three segments. Binary restenosis was defined as >50% diameter stenosis of the target lesion10.
STATISTICAL ANALYSIS
All calculations were performed with Statistical Package for the Social Sciences, version 13.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were expressed as mean±standard deviation, and categorical variables were presented as counts and percentages. A p-value <0.05 was considered significant.
Results
Table 1 shows the baseline clinical and angiographic characteristics of the patients. According to QCA analysis and visual estimation, 34 (53.1%) and 30 (46.9%) of the patients had Medina type 0,1,0 and 0,0,1, respectively. The mean age of patients was 60.0±11.2 years, and 41 (64.1%) patients were male. The most frequent PCI indication was stable angina (82.8%). The lesion localisations were ostium of the left anterior descending (LAD) artery in 20 (31.2%), mid level of the LAD artery in 14 (21.9%), ostium of the circumflex artery in nine (14.1%), ostium of the diagonal branch in 17 (26.6%), and ostium of the obtuse marginal branch in four (6.2%).
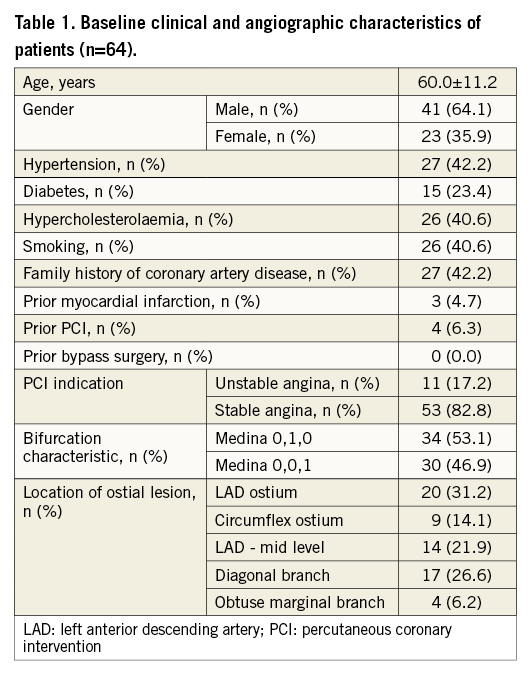
Table 2 shows procedural characteristics. Predilatation of the lesion was performed in 24 patients (43.8%). The procedural success rate was 100%. There was no major complication, but there were two minor intraprocedural complications, including dissection at the distal edge of the stent in two patients (managed by additional stent implantation). The anchor balloon did not prolapse into the target vessel in any patient. Because guidewires were twisted together, we could not advance the stent-balloon system to the lesion location in 10 patients (15.6%). In these patients, advancement of the stent-balloon system was stopped, one of the wires was pulled back to the tip of the stent or balloon, the wires were untwisted, and the stent-balloon system was recrossed into the vessel. Then, the stent-balloon system could be successfully advanced to the lesion location in all patients. There was no major adverse cardiac event during hospital stay.
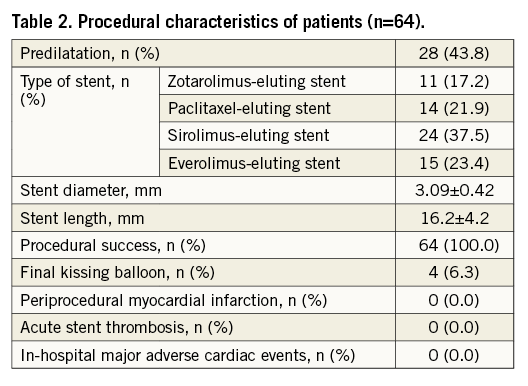
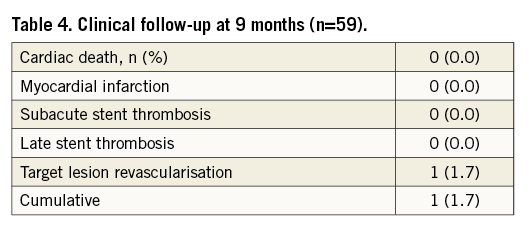
Clinical and angiographic follow-up was available in 59 patients (92.2%). QCA analysis results for both the main and the side branch at baseline, after the procedure and at nine-month follow-up are summarised in Table 3. There was no cardiac death, MI, subacute or late stent thrombosis at nine-month follow-up. Only one patient (1.7%) had binary restenosis as shown by QCA. This patient also had exertional angina and therefore we performed only balloon angioplasty due to focal in-stent restenosis. Thus, only one patient showed a major adverse cardiac event and TLR by PCI (Table 4).
Discussion
The most important characteristics of the modified flower petal technique in patients with Medina 0,1,0 or 0,0,1 lesions are complete coverage of the ostial bifurcation lesion by the stent struts without protruding into the adjacent vessel, a lower metallic burden at the carina region and easy application. This study showed that the modified flower petal technique also offered high immediate procedural success and excellent nine-month outcome in patients with ostial bifurcation lesions.
ISOLATED LAD OR CIRCUMFLEX ARTERY OSTIAL LESIONS
Isolated LAD or circumflex artery ostial lesions are considered to be unfavourable for percutaneous treatment because of the technical difficulty and potential risks. There are no specific recommendations for PCI in isolated circumflex ostial lesions3,11. However, two percutaneous treatment strategies are traditionally recommended in isolated LAD ostial lesions: floating stenting11 (precise stent implantation at the LAD ostium level with minimal protrusion into the area of the carina), and the crossover technique12 (a single stent is deployed from the distal left main vessel into the LAD crossing over the circumflex artery).
Medina et al11 recommended the implantation of a floating stent under angiographic/intravascular ultrasound (IVUS) guidance in the percutaneous treatment of ostial LAD lesions, without disease at the level of the distal left main coronary artery (LMCA) and circumflex origin. With this technique, angiographic compromise of the circumflex ostium was reported in 19 patients (26%), but was significant in only seven patients (10%). They concluded that carina displacement was the main mechanism of compromise of the circumflex ostium11. The European Bifurcation Club reported that, in cases with large bifurcation angles and IVUS documentation of the absence of disease in the distal LMCA, the floating stent technique is acceptable for the percutaneous treatment of isolated ostial LAD lesions3. However, optimal positioning of stenting in this technique is difficult. If the stent is positioned too proximally, it protrudes into the LMCA: this may compromise the circumflex ostium. Conversely, if the stent is positioned too distally, it does not entirely cover the ostial LAD lesion, which may result in acute recoil and late restenosis. Furthermore, stent positioning may be affected by cardiac movements. Therefore, optimal positioning of the stents is very important in this technique. For determining optimal stent positioning, Medina et al11 used IVUS guidance in 70% of cases. In the modified flower petal technique, the stent and anchor balloon are advanced together to the lesion location until the anchor balloon stops the advancement of the stent (Figure 2A). In this way, the anchor balloon can prevent excessive stent advancement into the target vessel and provide complete coverage of the lesion by stent struts without any manipulation. In our technique, inflation of the anchor balloon at nominal pressure into the adjacent vessel facilitates damage correction through repositioning of the carina.
Cubeddu et al12 proposed the crossover technique as the treatment approach for isolated ostial LAD lesions due to the potential risk of not totally covering the lesion. In this technique, the stent is placed from the distal LMCA to the LAD by crossing the circumflex artery ostium followed by final kissing balloon inflation (FKBI) to correct the carina position. However, this technique has some disadvantages, such as potential incomplete apposition of the stent in the LMCA due to the different diameters of the LMCA and side branch, the requirement of kissing balloon inflation, the use of longer stent lengths and the presence of metal in the LMCA. Furthermore, in an IVUS study, Medina et al11 reported that plaque was not found at the level of the carina in most patients (73%) with isolated LAD ostial lesions. We showed that the modified flower petal technique avoids metallic burden in a disease-free segment such as the LMCA, provides optimal positioning of the stent in the ostium of the LAD/circumflex artery, and does not require routine FKBI to correct the carina position.
ISOLATED OSTIAL NON-LEFT MAIN BIFURCATION LESIONS
Isolated side branch ostial lesions (Medina type 0,0,1) represent <5% of coronary bifurcation lesions and are very challenging lesions (especially in a Y-type bifurcation angle)1,13. The technical challenges are the problem of perfect ostial stent positioning, stent protrusion into the main vessel, and/or poor ostial coverage of the side branch lesion and high risk of plaque or carina shift (in the main vessel)3,4. The optimal strategy for patients with isolated ostial side branch lesions has not yet been determined3. A risk of injury to the main vessel when treating the side branch exists with all PCI techniques. For this reason, this subset of bifurcation lesions is usually managed medically5.
Several techniques, such as placement of a non-inflated balloon in the main vessel3,14 or the Szabo technique15, have been described to enhance the accuracy of stent placement. However, despite the use of these techniques, percutaneous treatment of ostial side branch lesions has an increased risk of incomplete coverage of the side branch ostium or stent protrusion into the main vessel, especially in a narrow bifurcation angle13,16. To overcome these problems, Brunel et al13 proposed the inverted provisional technique, with placement of the stent from the proximal main vessel into the side branch and final kissing, offering the advantage of complete coverage of the ostium. Complete coverage of the ostial side branch is obtained in all cases with this technique. However, this technique has some disadvantages, such as incomplete apposition of the stent in the proximal main vessel due to the different diameters of the proximal main vessel and side branch, the requirement of kissing balloon, the use of longer stent lengths and the presence of metal in the main vessel. Furthermore, strut crossing failure with this technique may compromise the main vessel. In a recently published, small study, Grundeken et al16 successfully treated 12 patients with Medina 0,0,1 lesions using a dedicated side branch stent alone (Tryton Side Branch Stent; Tryton Medical, Durham, NC, USA). This is a modification of the inverted provisional technique (modified Brunel technique). They reported 100% procedural success and acceptable long-term results. The most important disadvantage of this technique is the lack of drug on the bare metal Tryton, potentially resulting in an increase of the restenosis rate. Other potential disadvantages of the modified Brunel technique are insufficient radial strength and incomplete apposition of the wedding bands in the proximal part of the stent and the three panels of the transition zone16.
Szabo et al15 described a bifurcation technique for the treatment of isolated ostial bifurcation lesions by using the target wire and the anchor wire. In this technique, the anchor wire which passes through the most proximal stent strut helps to prevent excessive progression of the stent beyond the ostium and facilitates the precise stenting of the ostium. Recently, Gutiérrez-Chico et al17 reported that the Szabo technique is more accurate than the conventional technique in avoiding malpositioning of the stent. However, the Szabo technique is not the ideal technique due to technical difficulties. The anchor wire can be prolapsed into the target branch and the stent can advance excessively into the target branch, leading to incomplete coverage of the target branch ostium in the Szabo technique18. In our study, the anchor balloon did not prolapse into the target vessel in any patient. Because the anchor wire and the anchor balloon together provide stronger support, they do not prolapse into the target branch in the modified flower petal technique. In this way, the modified flower petal technique provides complete coverage of the target branch ostium. The most important difference between the modified flower petal technique and the Szabo technique is the expansion of the most proximal stent cell to the opposite vessel wall in the main branch. Therefore, in contrast to the Szabo technique, there is no protrusion of the stent strut into the main lumen in the modified flower petal technique. Furthermore, we think that due to the stent and anchor balloon being advanced together, the modified flower petal (MFP) technique has increased pushability compared to the Szabo technique.
Today, there is no consensus regarding the best technical approach for Medina 0,0,1 lesions3. We propose the modified flower petal technique for the treatment of this subset of bifurcation lesions. In this technique, the guidewire and balloon which are placed into the main vessel restrain the further advancement of the side branch stent, leading to complete coverage of the side branch ostium without protrusion of the stent into the main vessel. Unlike previous techniques, this technique provides complete coverage of the side branch ostium and does not require routine FKBI, and the presence of metal in the main vessel is minimal.
Limitations
This study is a single-centre experience with a relatively small sample size. This technique was not compared with other techniques such as floating stenting, the crossover technique, the Szabo technique or the inverted provisional technique. However, this is the first study to have evaluated the technical feasibility, safety and immediate and midterm procedural and clinical results achieved with the modified flower petal technique for Medina type 0,0,1 or 0,1,0 coronary bifurcation lesions. After these encouraging results, further larger randomised studies with longer follow-up, including comparing our technique with other techniques, are needed. In this study, twisting of wires was noted in only 10 patients (15.6%). However, this situation did not affect the success of the procedure. Another important disadvantage of our technique is decreased flexibility of the stent during advancement of the stent-balloon system. For this reason, this technique is not suitable for tortuous lesions. Intravascular ultrasound, or even better, optical coherence tomography, would certainly have been able to assess this result more accurately, but these were not performed systematically.
Conclusions
This study showed that the modified flower petal technique has excellent acute results and midterm clinical outcomes in the management of Medina type 0,0,1 or 0,1,0 coronary bifurcation lesions. It also has a number of advantages, such as complete lesion coverage while protecting the adjacent vessel, and a lower metallic burden at the carina region. However, additional randomised studies with larger sample sizes and longer follow-up are necessary to establish the long-term safety and efficacy of this technique.
| Impact on daily practice PCI of isolated ostial bifurcation lesions is challenging and associated with higher procedural and medium-term complication rates. The optimal strategy for patients with isolated ostial bifurcation lesions has not yet been determined. We propose a new technique, the “modified flower petal technique”, for the treatment of this subset of bifurcation lesions. Unlike previous techniques, this technique is easy to apply, provides complete coverage of the side branch ostium and does not require routine FKBI. |
Conflict of interest statement
The authors have no conflicts of interest to declare.