- coronary artery disease
- bifurcation
- drug-eluting balloon
- angiographic follow-up
Abstract
Aims: Percutaneous coronary interventions for bifurcation lesions are often complex and associated with an unsatisfactory result. The aim of this first-in-man, observational study was to investigate the efficacy and safety of a paclitaxel-eluting balloon in these lesions.
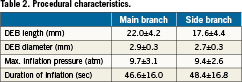
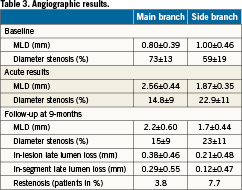
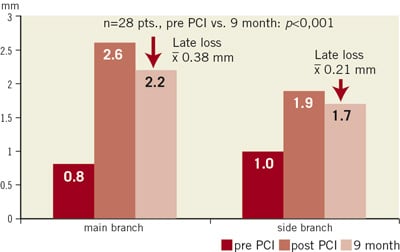
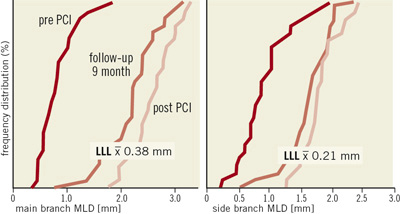
Methods and results: Twenty-eight patients presenting significant coronary bifurcational lesions of the left coronary artery were studied. The main branch (MB) and the side branch (SB) were dilated with a drug-eluting balloon (DEB; SeQuent® Please balloon catheter , 3µg paclitaxel/mm2 balloon surface). An open-cell bare-metal stent (BMS; Coroflex®) was then deployed in the MB. Only if the SB had a TIMI flow Conclusions: Percutaneous treatment of bifurcation lesions with a drug-eluting balloon resulted in a procedural success of 100%. Follow-up angiography at nine months showed DES-like results in MB and SB. However, when the DEB was used in combination with a BMS (MB), the possibility of late stent thrombosis cannot be ruled out. Introduction The treatment of coronary bifurcation lesions is often difficult. The introduction of drug-eluting stents (DES) has lowered the rate of in-stent restenosis in these lesions. Nevertheless, side branch (SB) stenting is still associated with a restenosis rate of more than 10%1. Several large randomised trials2-5 clearly showed that main branch (MB) stenting along with provisional SB stenting has evolved as the method of choice in the majority of patients. Considering these issues, the newly developed drug-eluting balloon may be advantageous as compared to plain old balloon angioplasty (POBA), in particular for the treatment of the SB. In this first-in-man, observational study, efficacy and safety of the DEB in bifurcation lesions were evaluated clinically and by re-angiography after nine months. Methods Patient population PEPCAD V was a prospective, dual centre, single arm, phase-II pilot study. The protocol was approved by the ethic committees of the participating centres. All patients gave their written informed consent. Male and non-pregnant female patients ≥18 years of age with the diagnosis of stable angina pectoris (CCS class 1-3) or unstable angina pectoris (Braunwald class 1-2, A-C) or documented ischaemia were considered eligible for enrolment. An additional eligibility criteria was the presence of a de novo left coronary artery bifurcation lesion, defined as a stenosis ≥70% in either one or both branches of the bifurcation or as a stenosis of ≥50%, if ischaemia corresponding to the target lesion was documented. In both branches, lesion length had to be ≤20mm. The reference vessel diameter had to be between 2.5 and 3.8 mm for the MB and 2.0 and 3.5 mm for the SB. Exclusion criteria were acute myocardial infarction, severe heart failure, cardiogenic shock, stroke, untreated hyperthyroidism and renal failure (GFR<30 ml/min). Procedure First, the SB was dilated with a DEB (SeQuent®Please balloon catheter, B. Braun Melsungen AG, Germany) whether it was stenosed or not. In case of a very severe SB branch lesion the SB branch was predilated. The DEB had to be inflated for ≥30 seconds. Then, the MB was dilated with a second DEB. The balloon diameter was the same as the intended stent diameter, but the DEB had to be longer than the stent by at least 2 mm on each side. Next, a BMS (Coroflex®, B. Braun Melsungen AG, Germany) was implanted within the “footprint” of the DEB to avoid a geographic mismatch. The ostium of the SB was postdilated with an uncoated balloon. Only if the SB had a TIMI flow Follow-up Visits or telephone contacts were scheduled at 30 days and nine months. Adverse events were monitored throughout the entire period of the study. Follow-up coronary angiography was performed nine months after the index procedure. Quantitative coronary angiographic measurements Angiographic analysis was performed by an independent core laboratory (Clinical Research Institute, Rotenburg an der Fulda, Germany). For the quantitative coronary angiographic analysis the computer assisted CAAS II (Pie-Medical, Maastricht, The Netherlands) was used. Angiography was performed after intracoronary injection of nitroglycerine to reveal the highest degree of stenosis. This evaluation was carried out centrally by two independent operators. A difference of ±3% of the relative stenosis between the two readings was accepted. Endpoint definitions and follow-up The primary endpoint of the study was procedural success, defined as a stenosis ≤30% in the MB and ≤50% in the SB along with TIMI III flow. Secondary clinical endpoints were major adverse cardiac events (MACE) up to three years. MACE was defined as cardiac death, myocardial infarction and target lesion revascularisation. Secondary angiographic endpoints were binary stenosis rate, late lumen loss, percent diameter stenosis and minimal lumen diameter (MLD) at nine months. Statistical analysis Statistical analysis was performed by the core laboratory using the validated program StatView, version 5.0 (SAS Institute Inc. Cary, NC, USA). The Kolmogorov-Smirnov test was used to prove the Gaussian distribution allowing for calculation of the mean and standard deviation. Non-Gaussian samples were described by median and range. Discriminant variables were evaluated with two-sided Fisher’s exact test. Continuous variables were compared with Students unpaired t-test. Atwo-sided value of p<0.05 was considered statistically significant. Results Baseline characteristics From October 2007 to July 2008, 28 patients were enrolled in the study. All of them had a history of stable angina pectoris. Baseline clinical characteristics are presented in Table1. Bifurcation lesions were located in the left anterior descending artery /diagonal branch (67.8%) or the circumflex artery/obtuse marginal branch (32.2%). According to the Medina classification, lesions were: 0,0,1 (3.6%); 0,1,1 (28.6%); 1,0,1 (10.7%); 1,1,1 (32.1%); 0,1,0 (10.7%); 1,0,0 (7.1%); 1,1,0 (3.6%). Thirteen of 28 patients had single vessel disease, 12/28, 2-vessel disease and 3/28, 3-vessel disease. Procedural characteristics After DEB dilation of the MB and the SB, stents were deployed in all MBs (28/28) and in 4/28 (14.3%) of the SBs. Dissections after DEB occurred in seven (25%) lesions in the MB and in three (10,7%) lesions in the SB. Table2 summarises inflation pressures, duration of balloon inflation as well as lengths and diameters of DEBs and stents. Stents deployed in the MB were 3.2±3.6 mm shorter than the MB DEB. SBs were postdilated with an uncoated balloon in 21/25 (84%) lesions and a final kissing balloon procedure was performed in 2/25 (8%) lesions. Angiographic results Crossing the lesions with a DEB was always possible and procedural success was achieved in all cases. The MLD increased from 0.80±0.39 mm to 2.56±0.44 mm in the MB (p<0.001) and from 1.00±0.46 mm to 1.87±0.35 mm in the SB (p<0.001). Percent diameter stenosis declined from 73±13% to 15±9% (MB, p<0.001) and from 59±19% to 23±11% (SB, p<0.001). At nine months, re-angiography showed an in-stent late lumen loss (LLL) of 0.38±0.46 mm and 0.29±0.55 mm in-segment in the MB resulting in an MLD of 2.2±0.60 mm, as well as an in-lesion late lumen loss of 0.21±0.48 mm and 0.12±0.47 mm in-segment in the SB resulting in an MLD of 1.7±0.44 mm (Table3, Figure 1). For the 24/28 stand-alone DEB procedures, the in-lesion late lumen loss was 0.12±0.40mm and in-segment 0.04±0.37mm. In combination with a bare metal stent (4/28), the in-stent LLL was 0.66±0.59mm and 0.52±0.73 in-segment. Figure 1. Minimal lumen diameter of MB and SB, pre-intervention (PCI), post-PCI and at nine month follow-up. Clinical outcome No MACE occurred up to 30 days. Within the 9-months follow-up, two patients had an asymptomatic restenosis of the SB (7.7%). No TLR was performed. A third patient with symptomatic restenosis in the MB underwent TLR (3.8%). Two late stent thromboses were reported, one definite and one probable, at six and eight months after index procedure. In both patients, the thrombosed vessel could be reopened acutely by balloon dilation alone. One of the two patients was a hypo-responder to both clopidogrel and aspirin. The dose of both agents had to be doubled in this patient. No patient died. Discussion Catheter interventions of coronary lesions involve a bifurcation in 15-20%6. The treatment of bifurcation lesions is usually more difficult as compared to non-bifurcation lesions and the complication rate is higher. Possible complications are acute SB closure (BBC one) and higher rates of restenosis and stent thrombosis (Nordic I and III). There are a number of reasons to explain these special features of a bifurcation lesion. Some are technical, such as carina shifting after stenting the bifurcation, double or triple layers of stents struts and stent distortion, for instance after dilating the SB through the stent struts. Some other reasons may be related to a different tissue distribution and composition of bifurcation lesions. In a recent publication, Garcia Garcia et al7 report their findings of virtual histology in bifurcation lesions. They found that in comparison to non-bifurcation lesions, bifurcation lesions have a larger plaque burden, a larger area of necrotic core in contact to vessel lumen, alarger necrotic core in the downstream segment and a higher number of thin cap fibroatheromas. All these characteristics could make abifurcation lesion more vulnerable for future events. Current interventional treatment of most bifurcation lesions consists in implanting a DES in the MB with POBA and provisional T-stenting of the SB (Nordic Bifurcation Study2, CACTUS study3, BBC one study4). It was the hypothesis of the present study to test a DEB in the treatment of bifurcation lesions. Since the SB is rarely stented, the DEB could be particularly helpful to reduce the restenosis rate of a SB lesion. In this respect, we were encouraged by the results of the PEPCAD I trial8. In this trial, de novo coronary artery lesions in small coronary vessels (mean reference vessel diameter of 2.35mm) were treated with a DEB only (82/118 patients) or, in case of dissection or elastic recoil, in combination with a BMS (32/118 patients). LLL for the whole PEPCAD I group was 0.32±0.56. If we only consider patients treated with the DEB, LLL was 0.18±0.38mm. However, LLL was significantly higher (0.73±0.74mm) in patients, where a BMS was implanted after the DEB. This less favourable result was probably most likely related to geographic mismatch between the DEB and the BMS. From these data we conclude that the SB of a bifurcation lesion may also benefit from a DEB to reduce the incidence of restenosis. If we use a DEB for the SB, the DEB will also be partly placed in the MB proximal to the bifurcation and deposit paclitaxel there. Since no data are available for a combined use of a DEB and a DES, using the DES in the MB was considered to pose an unknown risk. To avoid this overlap of drug delivery, we used the DEB for the MB in combination with a BMS. The BMS used in our study was the Coroflex® stent, an open cell design stent, which is not distorted in case of SB dilation through the stent struts11. Therefore, final kissing balloon dilation was not considered mandatory. Such an approach was feasible in all 28 patients. In 24/28 patients the SB was treated with a balloon only and no BMS was necessary. At nine months follow-up, the restenosis rates in the SB and in the MB were low, 7.7% and 3.8%, respectively (Figure 2). At follow-up, there was only a LLL of 0.38±4.6mm in the MB, a result which appears to be significantly better as compared to LLL seen after BMS9,10. In the SB, LLL was only 0.21±0.48mm, a result which may be described as DES-like. This characteristic behaviour is also reflected by typical MLD distribution curves. The MB curve shifts markedly to the right after DEB and stenting with only a minor leftward shift after nine months. In the SB, the acute curve and the nine month follow-up curve remain almost superimposed, indicating a negligible LLL. Generally these results are comparable to the results of bifurcation studies3 with DES. Figure 2. Cumulative frequency distribution curves, pre-PCI, post-PCI and at nine month follow-up). Two patients experienced late stent thrombosis. One at six, and the other at eight months. According to the protocol, both patients were already under aspirin monotherapy at this time. In one of the two patients, platelet aggregometry was performed, indicating hypo-responsiveness to both, aspirin and clopidogrel. One patient had a clinically driven TLR. No patient died. It is difficult to evaluate the risk of stent thrombosis, since both incidences observed were associated with incomplete stent expansion at deployment. What are the conclusions and clinical implications of this trial? A consensus group was asked to answer this question and develop recommendations for the use of the DEB in bifurcation lesions.12 These recommendations differ in various aspects from PEPCAD V. Predilation, for example, is recommended as an obligatory step for both branches using a conventional balloon with a balloon-to-vessel ratio of 0.8-1.0. In case of a good angiographic result in both branches, DEBs are used for SB and MB. In case of a major dissection or a reduced TIMI flow after predilation, usually a DES is implanted. Alternatively, the SB is first dilated with the DEB. Then, a BMS is deployed in the MB followed by a DEB (to avoid geographic mismatch). Only in case of amore than 75% residual stenosis in the SB or reduced TIMI flow, final kissing balloon dilation is performed. Dual antiplatelet therapy is recommended for a period of 12 months after DEB/BMS. Certainly, future studies are needed to show how this strategy compares with others presently used, for instance, DES in the MB and conventional balloon dilation of the SB. Obviously, it would be also very interesting to know whether the combination of a DES in the MB and a DEB in the SB would turn out as a valid and safe approach. Furthermore, the possibility of using DEB only in bifurcations deserves evaluation. Acknowledgement The study was supported by B. Braun Melsungen AG, Germany. Database was provided and basic statistics was performed by Unverdorben M and Degenhardt R, Clinical Research Institut, Herz- und Kreislaufzentrum, Rotenburg an der Fulda, Germany. Conflict of interest statement D.Mathey has received speaker fees from B.Braun. M.Boxberger is an employee of B.Braun. F.Kleber has a consulting agreement with B. Braun and has received lecture honoraria and free scientific research grants from B.Braun, Eurocor, Invatec-Medtronic and Biotronik). I.Wendig and K.Bonaventura have no conflicts of interest to declare. References