Abstract
Aims: Paclitaxel drug-eluting balloons (pDEB) could be an attractive option to minimise side branch (SB) restenosis in bifurcated coronary lesions. We compared angiographic and clinical outcomes with pDEB plus bare metal stent (BMS) versus drug-eluting stents (DES) in de novo bifurcated lesions.
Methods and results: This multicentre randomised trial included 108 patients. Sequential main branch (MB)/SB dilatation with pDEB, with provisional T-stenting with BMS in the MB was performed in the pDEB group, and with everolimus DES in the DES group. The primary endpoint was late lumen loss (LLL) at nine months. The secondary endpoint was the incidence of major adverse cardiac events (MACE: death, myocardial infarction, or target lesion revascularisation). In-segment MB LLL was 0.31±0.48 mm in the pDEB group, and 0.16±0.38 mm in the DES group (p=0.15); mean difference was 0.15 mm (upper limit one-sided 95% CI: 0.27 mm; p=0.001; non-inferiority test). LLL in SB was –0.04±0.76 mm in the pDEB group and –0.03±0.51 mm in the DES group (p=0.983). MACE and TLR were higher in the pDEB group (17.3% vs. 7.1%; p=0.105, and 15.4% vs. 3.6%; p=0.045), due to higher MB restenosis (13.5% vs. 1.8%; p=0.027).
Conclusions: pDEB bifurcation pretreatment with BMS implantation in MB showed greater LLL (ns) and increased incidence of MACE compared to everolimus DES. Both strategies showed similar results in the SB.
Introduction
Approximately 15% of percutaneous coronary interventions (PCI) are performed on bifurcation lesions. Approximately 75% of these are authentic, according to the Medina classification1,2. Coronary bifurcation lesions are still a challenge for PCI due to suboptimal results, mainly in the side branch. The use of drug-eluting stents (DES) has not solved the issue, and bifurcation lesions generally have higher rates of restenosis and thrombosis, especially when more complex techniques are used3. Therefore, the provisional side branch interventional strategy is preferred for most bifurcation lesions1,3.
The ideal strategy combining simplicity and efficiency is still elusive. In this regard, the paclitaxel drug-eluting balloon (pDEB) is an attractive therapeutic option, able to deliver the antirestenotic agent paclitaxel in the vessel wall without the need for an in-place stent or polymer. However, its final role in different PCI niches has still to be defined4. pDEB has shown good results for in-stent restenosis5. Some results in PCI of small vessels are conflicting6,7, and very few studies on bifurcations are available, representing only 13% of the DEB registry, compared to 62% for in-stent restenosis8-10.
pDEB could provide an attractive alternative to treat bifurcations in order to minimise side branch restenosis. Our purpose was to conduct a multicentre randomised prospective trial in which pretreatment of main branch (MB) and SB with a pDEB using a provisional T-stenting technique with a bare metal stent (BMS) was compared with the same technique using regular balloon angioplasty and DES.
Methods
The Paclitaxel-Coated Balloon in Bifurcated Lesions Trial (BABILON) is a randomised multicentre study aimed at comparing a provisional T-stenting technique for coronary bifurcation lesions with predilatation of both branches using pDEB followed by BMS implantation in the MB (pDEB group) versus standard predilatation in both branches and DES implantation in the MB (DES group).
PATIENT SELECTION
Eligible patients were those with stable or unstable angina or silent ischaemia, scheduled to undergo PCI for de novo coronary artery lesions (stenosis >50% and <100%) located at the level of a bifurcation, with an MB diameter ≥2.5 mm and lesion length <32 mm and an SB diameter of ≥2.0 mm. Exclusion criteria were: ST-elevation myocardial infarction (STEMI) in the previous 48 hours, unprotected left main disease, restenotic lesions, pregnancy, allergy to aspirin, clopidogrel, heparin or abciximab, active bleeding or a significant increase in bleeding risk, significant renal insufficiency (defined as creatinine >2 mg/dl), severely depressed left ventricular (LV) function (ejection fraction ≤35%), cardiogenic shock, ischaemic stroke within the last six months, contraindication for DES (chronic oral anticoagulant therapy, planned surgery within 12 months of the index procedure, unless dual antiplatelet therapy could be maintained throughout the perioperative period), inability to give informed consent, and life expectancy <12 months.
Patients eligible for the study were randomised to the pDEB or DES group in a 1:1 ratio (Figure 1). Patients were allocated to each treatment group by an independent person, according to a randomisation table. The study protocol was reviewed and approved by the ethics committees of all the participating centres and all patients signed a written informed consent according to the Declaration of Helsinki, as revised in 2002. This trial is registered in the ClinicalTrials.gov website (Identifier NCT01278186).
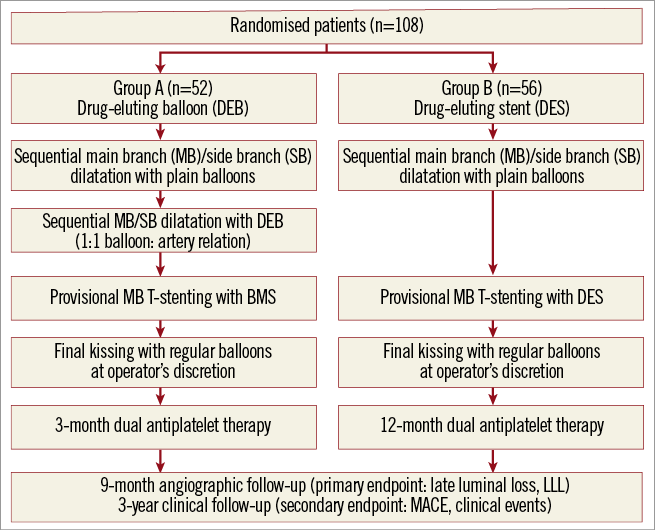
Figure 1. Study flow diagram.
ADJUNCTIVE PHARMACOLOGICAL THERAPY
Patients received aspirin at a daily dose of 100 mg. Oral clopidogrel was initiated at a loading dose of 600 mg before or immediately after the procedure and continued thereafter at a daily dose of 75 mg. Patients in the DES group were prescribed oral clopidogrel for a minimum of 12 months, and patients in the DEB group for three months and for extended periods thereafter at the physician’s discretion. Administration of heparin, bivalirudin or glycoprotein IIb/IIIa inhibitors was left at the physician’s discretion.
INTERVENTIONAL PROCEDURE AND STUDY DEVICE
Sequential MB/SB predilatation with regular balloons was recommended in both groups. In those patients assigned to the pDEB group, sequential MB/SB dilatation with pDEB in a 1:1 balloon:artery relation was performed, followed by provisional T-stenting with BMS implantation in the MB. The pDEB tested was the SeQuent® Please paclitaxel-eluting coronary angioplasty balloon catheter (B. Braun Melsungen AG, Berlin, Germany). The BMS was the Coroflex® Blue cobalt-chromium coronary stent system (B. Braun Melsungen AG) and the DES was the XIENCE V® everolimus-eluting stent (Abbott Vascular, Santa Clara, CA, USA).
In the SeQuent® Please drug-eluting balloon, paclitaxel is integrated into a matrix and hydrophilic substance, the contrast medium iopromide. In this hydrophilic matrix, the lipophilic paclitaxel is then bioavailable and penetrates the wall after application. The paclitaxel dose is 3 µg/mm2.
The minimum inflation time of the pDEB is 40 seconds to allow sufficient drug to be released into the vessel wall. The use of a pDEB longer than the length of the stent was recommended. Provisional T-stenting with DES implantation in the MB was performed in patients assigned to the DES group. Final kissing with regular balloons was encouraged but left at the operator’s discretion. Sequential dilatation was also allowed. If necessary, additional bail-out stenting of the SB was performed, using a stent appropriate to the randomisation group.
CLINICAL AND ANGIOGRAPHIC FOLLOW-UP
Patients were prospectively followed up after discharge at 1, 6, 12 and 24 months. All data available were collected in a common electronic database, which was reviewed at the end of the follow-up period. All clinical endpoints were blindly assigned by an independent clinical events committee.
All patients were asked to undergo angiographic follow-up at nine months. Coronary angiograms obtained at baseline, at stenting completion, and at nine months of follow-up were computer-analysed (Xcelera®; Philips Healthcare, Best, The Netherlands) by two independent and experienced individuals blinded to treatment assignment. An HK bifurcation diameter model was used to estimate the reference diameter of the side branch11. Quantitative measurements of the target lesion were obtained in the “in-stent” zone and in the “in-segment” zone (including the stented segment as well as the 5 mm margins) in the MB and SB. Binary restenosis was defined as a diameter stenosis >50% at angiographic follow-up. Late luminal loss (LLL) was defined as the difference between the minimal luminal diameter (MLD) at completion of the stenting procedure and MLD measured during follow-up.
STUDY ENDPOINTS AND DEFINITIONS
An MB result was considered optimal if there was successful implantation of the stent with residual stenosis <20% and TIMI 3 flow after the procedure. An SB result was considered optimal if there was residual stenosis <50%, TIMI 3 flow and no image suggestive of dissection. The primary endpoint was the in-segment LLL in the MB and SB at angiographic follow-up at nine months. The secondary endpoint was the incidence of major adverse cardiac events (MACE) (composite of death, myocardial infarction [MI], and target lesion revascularisation [TLR]) after 24-month clinical follow-up. MI was diagnosed by persistent ischaemic-type chest pain with a rise in biochemical markers of myocardial necrosis (CK-MB and troponin), at least twice the upper limit of normal laboratory reference values. TLR was defined as a new intervention (surgical or percutaneous) to treat significant luminal stenosis (>50% diameter stenosis by visual estimation) in the treated segment (including the stented segment and the adjacent 5 mm proximal and distal in the MB, and the balloon-treated zone plus 5 mm distal in the SB). Stent thrombosis (ST) was considered according to the criteria for definite ST described by the Academic Research Consortium (ARC).
STATISTICAL ANALYSIS
Sample size calculation was based on a 0.4 mm non-inferiority margin for in-stent LLL. This non-inferiority threshold was determined from previous studies demonstrating that LLL would have no clinical impact if <0.5-0.6 mm12. Since LLL in DES is about 0.15 mm, additional LLL for pDEB should be more than 0.4 mm.
Despite an initial sample size calculated in 190 patients, the study was stopped after the inclusion of 108 patients due to low enrolment rate. This final sample size has 90% statistical power to demonstrate that the difference in mean LLL with pDEB plus BMS is within 0.4 mm of that of DES using a one-sided statistical test with an alpha level of 0.025.
All data are presented on the basis of the intention-to-treat principle. Continuous variables are presented as mean±SD, and categorical variables are described with absolute and relative (percentage) frequencies. Comparisons between the two groups were performed using the unpaired t-test for continuous variables and the Pearson χ2 test or Fisher’s exact test for categorical variables. All tests were two-sided, and a probability of p<0.05 was considered statistically significant. All data were analysed with SPSS version 16 (SPSS Inc., Chicago, IL, USA).
Results
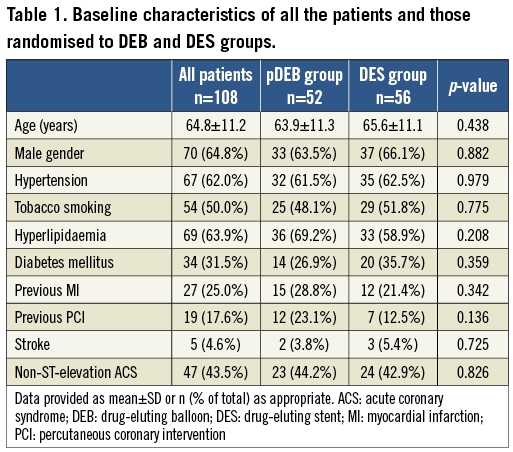
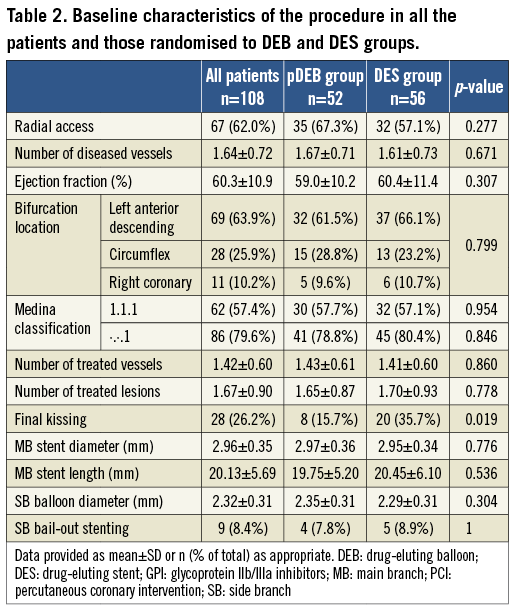
A total of 108 patients were enrolled in eight Spanish centres between January 2010 and January 2012. Table 1 shows the main baseline characteristics of the global sample and the comparison between the DES (56 patients) and the pDEB group (52 patients). The mean age of the study population was 64.8±11.2 years, 65.7% were males, and 31.5% had diabetes mellitus (DM). There was a high percentage of patients with acute coronary syndrome (68.5%). No differences in baseline characteristics were found between randomisation groups. Table 2 shows the variables related to the PCI procedure. The groups were well balanced for all variables.
IN-HOSPITAL CLINICAL OUTCOME
Three (2.8%) periprocedural non-Q-wave myocardial infarctions and one stent thrombosis occurred during hospitalisation, all of them in the DES group. No in-hospital deaths or repeated revascularisation were recorded.
ANGIOGRAPHIC FOLLOW-UP
Angiographic follow-up was performed in 86 patients (80.4%). There were no baseline differences between patients with and without angiographic follow-up. Table 3 summarises the baseline data, measurements after the procedure and at nine months for patients with angiographic analysis. There were no significant differences in baseline angiographic variables between groups, although the length of the lesion in the MB was slightly higher in the pDEB group. Likewise, post-procedural measures showed no differences in MLD between groups.
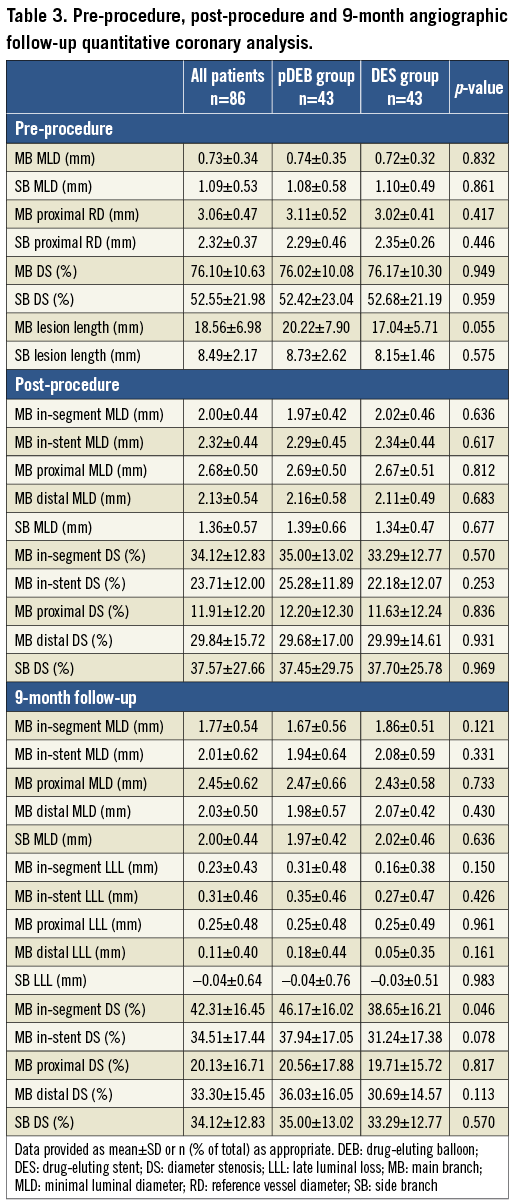
No significant differences were shown in nine-month in-segment LLL in the MB between groups (0.31±0.48 mm vs. 0.16±0.38; p=0.150). The observed difference in the mean of in-segment LLL in the MB was 0.15 mm (SD=0.075). The upper limit of the one-sided 95% CI was 0.273 mm (p=0.001, non-inferiority test). Positive remodelling (with negative LLL) was observed at the SB ostium in both groups in the follow-up visit at nine months, with no significant differences (Figure 2).
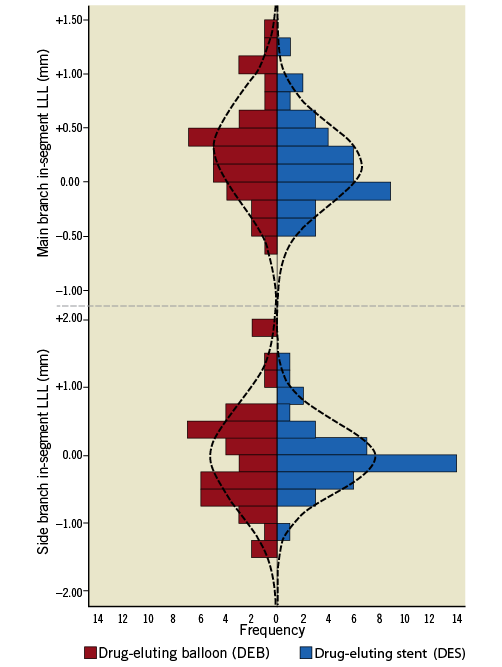
Figure 2. Frequency distribution of in-segment late luminal loss (LLL) values at nine months for DEB (red) and DES (blue) groups in main branch and side branch. Superimposed curves represent normal probability function based on mean and variance of data.
CLINICAL OUTCOME
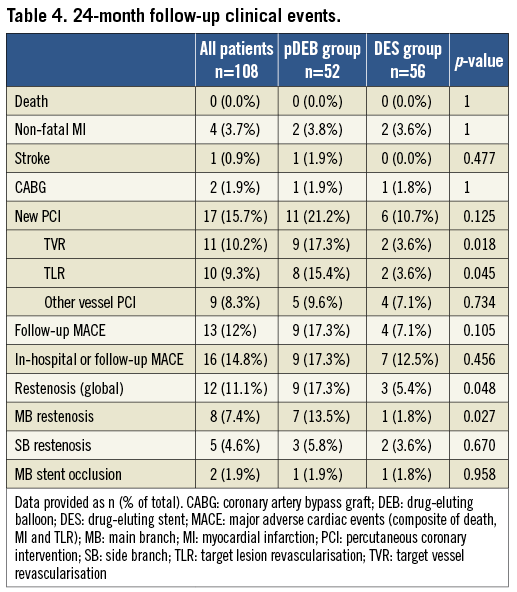
Clinical 24-month follow-up data are presented in Table 4. No deaths were reported during follow-up. Two stent thromboses were reported, one in the pDEB (1.9%; 289 days after the index procedure in a patient without angiographic follow-up) and one in the DES group (1.8%; 10 days after the procedure, being still hospitalised) which was treated with emergency percutaneous coronary intervention. MACE were non-significantly higher in pDEB (7.1 vs. 17.3%; p=0.105). Including in-hospital events, the MACE rate was 17.3% in the pDEB vs. 12.5% in the DES group (p=0.456). TLR was significantly more frequent in the pDEB group (15.4 vs. 3.6%; 0.047). The restenosis rate was significantly higher overall (17.3 vs. 5.4%; 0.048) and in MB-pDEB (13.5 vs. 1.8%; p=0.027) and not significant in SB (5.8 vs. 3.6%; p=0.670).
Discussion
The main results of our study can be summarised in angiographic results and clinical outcomes. In terms of angiographic results, the in-segment LLL in the MB was higher in the pDEB group compared to the DES group, but without reaching statistical significance and there was a very small difference in the in-segment MLD, 0.19 (Table 3). Significant differences were found in the MB in-segment restenosis, with better results in the DES group (p=0.046). However, no differences were found between groups in the case of SB, and positive remodelling in the SB ostium was observed in both groups.
As for clinical outcomes, no significant differences were found in MACE (17.3% in the pDEB group vs. 7.1% in the DES group), although TLR and target vessel revascularisation (TVR) were significantly higher in the pDEB group. These differences were due only to higher restenosis of the main branch. In addition, this intervention does not seem to increase the risk, since the rate of PCI occlusion without pDEB was not higher, as already shown in other studies and in contrast to PEPCAD V data8,9.
In general, studies comparing the use of DES vs. pDEB on native vessels have shown the strategy DEB+BMS to be inferior to DES, especially if the DES used is a limus. Thus, in the PEPCAD III study, also with the SeQuent® Please balloon, the in-segment LLL was 0.20 vs. 0.11 mm (p=0.06). As in our study, the percentage of diabetic patients included was approximately 30%, higher than in studies with other balloons. The MACE rate at nine months was 22.0% in pDEB+BMS vs. 11.8% in sirolimus DES (p=0.001)13. A study in de novo lesions with a similar design but with a layered balloon (second-generation Elutax; Aachen Resonance GmbH, Aachen, Germany) compared pDEB+BMS vs. everolimus DES, and found an in-segment LLL of 1.14 vs. 0.34 mm (p=0.001) and TLR 14% vs. 2% (p=0.001), respectively14. The DEBIUT study, with the DIOR® I balloon (Eurocor GmbH, Bonn, Germany) in bifurcations, randomised patients into three groups: BMS, pDEB+BMS and DES (TAXUS®; Boston Scientific Corp., Natick, MA, USA), with 37, 40, and 40 patients, respectively. This study found an in-segment LLL of 0.49, 0.41 and 0.19 mm (p=0.001), MACE were 29.7%, 20% and 17.5%, and TLR rates were 27%, 20% and 15%, respectively (p=0.4)9. In this study, significant differences between the DEB and DES groups were observed, despite there being only 40 patients in each group, which is most likely because the DEB group had higher LLL than that in our study.
Conversely, when DEB SeQuent Please+BMS was compared with the TAXUS stent, the results were equivalent between groups. In this regard, the PEPCAD IV study in patients with DM found an in-segment LLL of 0.37 vs. 0.35 mm, TLR 8.9% vs. 10.3%, and MACE rates of 13.3% vs. 15.4%, without significant differences15. The superiority of DES over the BMS+pDEB strategy can be extracted from these studies. Some DEBs might be more effective than others, due to different delivery systems or other factors16-18 and, when comparing DEB and DES, greater differences seem to be found when a limus stent is used in place of a paclitaxel stent 13,14,18,19. In this context, it is important to note that this study uses everolimus DES for comparison, while most studies in this field use paclitaxel DES.
Studies with intravascular ultrasound (IVUS) have shown significantly greater neointimal proliferation with pDEB+BMS than with DES. In a subanalysis of the PEPCAD III study, neointimal hyperplasia was 0.69±0.49 mm for the first method, compared with 1.08±0.53 mm for DES20. However, optical coherence tomography (OCT) in other studies, such as DEB-AMI, suggests morphological changes induced by the DEB drug (such as the percentage of uncovered and malapposed struts) that are closer to the effect of DES than to BMS alone21. Various hypotheses have been considered such as, for example, that the geographical miss or implantation order may reduce effectiveness of the drug delivered by the DEB. This issue was answered in an interesting study in OCT showing that the strategy of implanting the stent first and then the balloon or vice versa did not influence the outcome. However, slightly better apposition and reference of the balloon covering the lesion can be achieved placing the BMS first and then the DEB22. An analysis of the case studied in this report suggests that there is some axial and longitudinal diffusion of the drug delivered by the pDEB22. Therefore, among the limitations of this technique, the time-limited antirestenotic effect of DEB may be relevant, being less than necessary to counteract the chronic proliferative stimulus generated by the BMS7,18.
Finally, when the results of the SB are analysed, little difference is observed. This may be surprising, since pDEB might be expected to be superior to a conventional balloon. However, two important studies including IVUS of the SB before and after the procedure have shown that the majority of cases with significant angiographic stenosis are due to a displacement of the carina, rather than movement of the plaque23,24. Therefore, the potential beneficial effect of the pDEB on the SB ostium may be overridden by the effect of carina displacement.
Additionally, the fact that positive remodelling in the SB ostium was also detected during follow-up in the group without pDEB may have had an influence. Furthermore, stenting of the SB was needed in approximately 8% of both groups, which is consistent with other randomised studies of bifurcations1,3. This mechanism, together with a smaller amount of perfused myocardium compared to a main vessel, might explain the paucity of events related to ostial impairment of the SB.
Our rate of SB restenosis was 15%, almost equal in both groups, which is consistent with studies of bifurcations1,3. The kissing rate was low in both groups, particularly in the pDEB group. The choice of performing either kissing technique or sequential two-step post-dilation of the SB and MV was left to the operator’s discretion, since the latter has been shown to be simpler and at least as efficient as an alternative to final KB technique for provisional stenting of a bifurcation25.
Limitations
The main limitation of the study lies in the reduced number of patients. However, it is in line with similar studies found in the literature. The study was powered and designed to enrol 190 patients and was stopped early due to slow enrolment, which limits the power and conclusions of the study. Furthermore, although 100% angiographic follow-up was not achieved, 80% of patients were followed up, which is again in line with similar studies. Finally, although our hypothesis of non-inferiority in LLL had a broad limit (0.4 mm), this is duly justified by studies of its clinical impact. Our study is underpowered to demonstrate a benefit in some clinical outcomes.
Conclusion
In conclusion, our study in bifurcation lesions with the provisional stenting technique, randomised to everolimus DES vs. pDEB (SeQuent® Please)+BMS (Coroflex® Blue) in the MB showed an in-segment LLL in the MB almost twice as high in the pDEB group compared to the DES group, albeit below statistical significance. No advantages were found in the SB with pDEB strategy, since no differences were found in the SB between groups.
No significant differences were found in MACE, although TLR and TVR were significantly higher in the pDEB group. These differences were due solely to higher restenosis of the main branch.
| Impact on daily practice In bifurcation lesions everolimus-DES present as a superior strategy over BMS+pDEB in the main branch (MB). This is of interest as most clinical events are due to restenosis of the MB. There are no angiographic differences on LLL of the ostium of the side branch (SB) after dilatation with plain balloon or pDEB, whereas there is a positive remodelling at follow-up, independent of the strategy used. So, at the present time, in daily practice, and with the strategy described in our study, there is no advantage of using pDEB in the SB. Future studies with dedicated DES respecting the ostium of the SB (without displacing the carina of the bifurcation) might show an advantage of using pDEB in the SB. |
Acknowledgements
The translation services for this article have been funded with a grant from Asociación Sociedad Extremeña de Cardiología and B. Braun Spain.
Funding
This article received a grant from Asociación Sociedad Extremeña de Cardiología and B. Braun Surgical S.A. Spain.
Appendix
INVESTIGATORS OF THE BABILON GROUP
Hospital Infanta Cristina: José Ramón López-Mínguez, Juan Manuel Nogales Asensio, Javier Doncel Vecino, María Reyes González-Fernández, Ginés Martínez-Cáceres, Antonio Merchán Herrera
Hospital Clínico de San Carlos: Jorge Sandoval, Alberto Cárdenas, María José Vizcaino, Fernando Alfonso, Carlos Macaya
Hospital San Pedro de Alcántara: Sebatián Romani, Javier Fernández-Portales
Hospital Puerto Real: Pedro Martínez Romero
Hospital Clínica Puerta de Hierro: José Antonio Fernández Díaz, Javier Goicolea Ruigómez
Hospital Virgen de la Salud: José Moreu Burgos
Hospital Virgen de la Victoria: Antonio Hernández
Hospital Son Espases: Alfredo Gómez
Conflict of interest statement
None of the authors has any conflict of interest related to the manuscript content or the products used in the study.

