
Abstract
Aims: To report clinical outcomes in patients treated with drug-eluting balloon (DEB) versus second-generation drug-eluting stent (DES) for in-stent restenosis (ISR) involving a bifurcation lesion.
Methods and results: Between February 2007 and November 2012, 167 bifurcation restenoses in 158 patients were treated with either DEB (n=73) or second-generation DES (n=85). The EuroSCORE was significantly higher in the DEB group (4.2±3.8 vs. 2.8±2.1, p=0.004). Regarding restenosed stent type, second-generation DES was more frequently seen in the DEB group (26.9% vs. 6.7%, p<0.001). In this group, there was also a trend towards more frequent stenting for a previous ISR (stent-in-stent) as compared with the DES group (25.6% vs. 15.6%, p=0.074). Over a median follow-up period of 701 days, there was no significant difference in major adverse cardiac events (MACE), defined as cardiac death, myocardial infarction including periprocedural myocardial infarction, target vessel revascularisation, between the two groups (p=0.585). Independent predictors of MACE on multivariate Cox regression analysis included stent-in-stent (HR: 2.16; 95% CI: 1.11 to 4.20; p=0.023) and true bifurcation lesions (HR: 2.98; 95% CI: 1.45 to 6.14; p=0.001).
Conclusions: DEB for bifurcation restenosis may be an acceptable treatment option, especially in cases where repeat stenting has not already been performed for the treatment of a previous restenosis.
Introduction
Percutaneous coronary intervention (PCI) for in-stent restenosis (ISR) is associated with high rates of recurrent restenosis and repeat revascularisation1. A previous meta-analysis has demonstrated the effectiveness of drug-eluting stents (DES) for the treatment of patients with ISR in bare metal stents (BMS), which is currently considered the default approach2. On the other hand, treatment with drug-eluting balloon (DEB) is increasingly being used in certain de novo lesions and ISR3,4. Previous papers have reported that DEB use for BMS-ISR is feasible and effective, as compared with uncoated balloon or paclitaxel-eluting stents (PES)5,6. In the updated European Society of Cardiology guidelines, DEB received a class 2a recommendation for the treatment of BMS-ISR. On the other hand, the best treatment for DES-ISR remains controversial, although recent studies have reported that repeat implantation of DES with a different or the same drug is feasible and safe1,7-11. Recently, DEB has been shown to be superior to balloon angioplasty alone and equivalent to PES for DES-ISR12-14.
To date, there are scarce data on PCI strategies for the treatment of ISR (irrespective of stent type) at bifurcation sites, where the best treatment strategy even for de novo lesions is still debatable15-19. The strategies currently utilised in routine clinical practice include the use of specialised balloons such as DEB, cutting and scoring balloons, the implantation of newer-generation DES and the use of rotational and excimer laser atherectomy. Of these, DEB for ISR at bifurcations can be a beneficial and attractive approach in order to suppress further neointima growth and avoid further metal layers. The aim of this study was to evaluate clinical outcomes following treatment with DEB for bifurcation ISR, as compared to second-generation DES.
Methods
We retrospectively evaluated all consecutive patients who underwent PCI with the IN.PACT Falcon (Medtronic, Minneapolis, MN, USA) for ISR involving bifurcation lesions (DEB was used either on the main branch [MB] and/or the side branch [SB]) between February 2007 and August 2012 at four centres: 1) San Raffaele Scientific Institute, Milan, Italy; 2) EMO-GVM Centro Cuore Columbus, Milan, Italy; 3) Ospedale Niguarda Ca’ Granda, Milan, Italy; 4) Clinical Institute S. Ambrogio, Milan, Italy. We also analysed consecutive patients with such lesions treated with second-generation DES as a control group. The first-generation DES used in this study were the CYPHER® (Cordis Corp., Johnson and Johnson, Warren, NJ, USA) and the TAXUS® (Boston Scientific, Natick, MA, USA). On the other hand, the second-generation DES were the XIENCE PRIME™ and the XIENCE V® (Abbott Vascular, Santa Clara, CA, USA), the Promus™ and the PROMUS Element™ (Boston Scientific Corp.) and the Endeavor® Resolute (Medtronic). The bifurcation angle between the MB and SB was measured at the angiographic projection at which it was the widest. Prior to DEB inflation or stenting, predilatation with a non-compliant balloon was encouraged as well as aggressive post-dilatation after stenting. Kissing balloon inflation was routinely performed when double stenting was performed. All patients were pre-treated with aspirin and either ticlopidine or clopidogrel. A 600 mg loading dose of clopidogrel before the index procedure was administered if patients were not pre-treated. Procedural anticoagulation was achieved with either intravenous unfractionated heparin or bivalirudin per the standard of care, and the administration of glycoprotein IIb/IIIa inhibitors was per the operator’s discretion. Following the procedure, an electrocardiogram was performed and cardiac enzyme levels were measured. Patients received aspirin indefinitely and daily clopidogrel (or ticlopidine, if required) for a minimum of: 1) 30 days in cases treated only with DEB; 2) three months in those with BMS following DEB; and 3) 12 months following DES implantation. Clinical follow-up was performed by either hospital visits or telephone contact. Angiographic follow-up was performed if clinically indicated.
Study definitions
The measured endpoints were major adverse cardiovascular events (MACE) during the follow-up period. MACE were defined as the composite of cardiac death, myocardial infarction (MI) (including periprocedural MI) and target vessel revascularisation (TVR), and were evaluated on a per patient basis. Target lesion revascularisation (TLR) was also analysed on a per patient and bifurcation basis. In the DEB group, a separate analysis was performed for bifurcation lesions treated for a second restenosis (stent-in-stent restenosis) with DEB when the first restenosis had been treated with a stent. This particular group was defined as the stent-in-stent group.
Death was considered cardiac in origin unless obvious non-cardiac causes could be identified. We defined periprocedural non-Q-wave MI as a creatinine kinase-myocardial band elevation of >3 times the upper limit of normal20. Creatinine kinase was routinely measured in all patients within 12 hours of the procedure and repeated if this measurement was elevated, if there was an intraprocedural complication, or if the patient had evidence of myocardial ischaemia. Non-procedural or spontaneous MI was defined as an elevation of troponin above the upper range limit in combination with at least one of the following: symptoms of ischaemia; electrocardiographic changes indicative of new ischaemia; or the development of pathological Q-waves on the electrocardiogram. TVR was defined as repeat PCI or coronary artery bypass graft (CABG) for the target vessel. TLR was defined as repeat PCI or CABG for the lesion in the previously stented segment or within the 5 mm proximal or distal to the stent edge or site of DEB inflation. The occurrence of stent thrombosis (ST) was defined on the basis of the Academic Research Consortium definitions20. Bifurcation lesions were classified according to Medina by two independent physicians21. Focal, diffuse, or occlusive restenosis was defined according to the Mehran classification22. Chronic kidney disease (CKD) was defined by an estimated glomerular filtration rate <60 ml/min/1.73 m2. The European System for Cardiac Operative Risk Evaluation (EuroSCORE)23 and the Synergy between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) score were calculated24. Procedural success was defined as completion of the procedure with no in-lab complications, final TIMI 3 flow with residual stenosis <30% after stenting and ≤50% when stent implantation was not performed.
Statistical analysis
Values are presented as mean±standard deviation or median (interquartile range [IQR]) for continuous variables or as counts and percentages for categorical variables. Clinical, echocardiographic, angiographic or procedure-related characteristics of patients were compared using the Student’s t-test or Wilcoxon rank-sum test (continuous variables), or the chi-square or Fisher’s exact test (categorical variables), as appropriate. Comparisons of time-to-event curves (Kaplan-Meier method) were performed with the log-rank test. Cox regression analysis using purposeful selection of covariates25 was performed to determine the independent predictors of MACE, using predictors associated with MACE in univariate analysis (p-value <0.2) and those judged to be of clinical importance from previously published literature. To avoid overfitting, the number of independent variables entered into the final multivariable model was limited to a maximum of one for every eight to 10 events. The results were reported as adjusted hazard ratios (HR) with associated 95% confidence interval (CI). All analyses were conducted using SPSS for Windows, version 19.0 (IBM Corp., Armonk, NY, USA) and all reported p-values are two-sided. Values of p<0.05 were regarded as statistically significant.
Results
PATIENT DEMOGRAPHICS
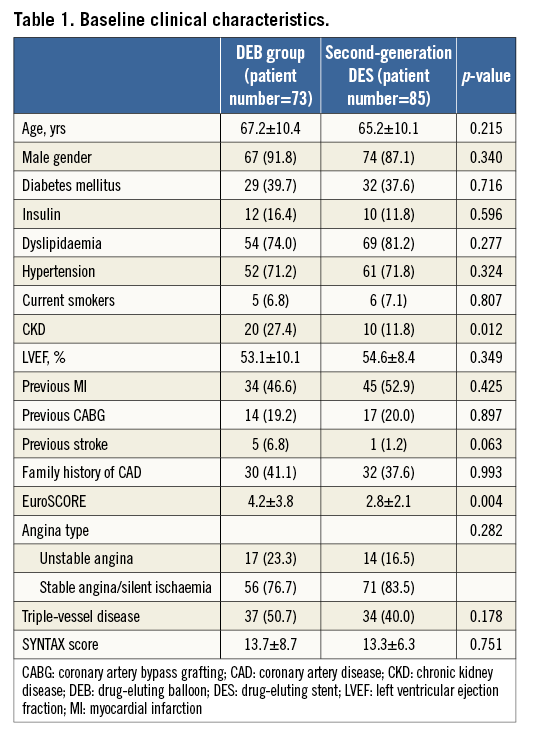
During the median follow-up period of 701 (IQR 353-1,087) days, a total of 167 bifurcation restenoses in 158 patients were treated either with DEB (78 bifurcations in 73 patients), or second-generation DES (89 bifurcations in 85 patients). The baseline clinical characteristics are shown in Table 1. EuroSCORE was significantly higher in the DEB group (4.2±3.8 vs. 2.8±2.1, p=0.004) due to higher incidences of CKD (27.4% vs. 11.8%, p=0.012) and previous stroke (6.8% vs. 1.2%, p=0.063). In both groups, the incidence of diabetes was relatively high (39.7% vs. 37.6%, p=0.716).
ANGIOGRAPHIC AND PROCEDURAL DETAILS
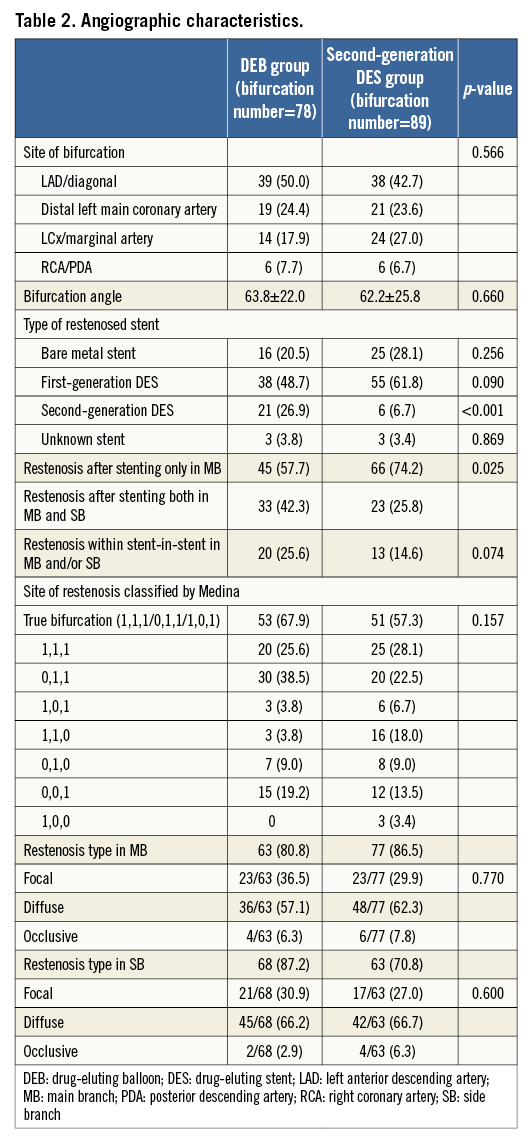
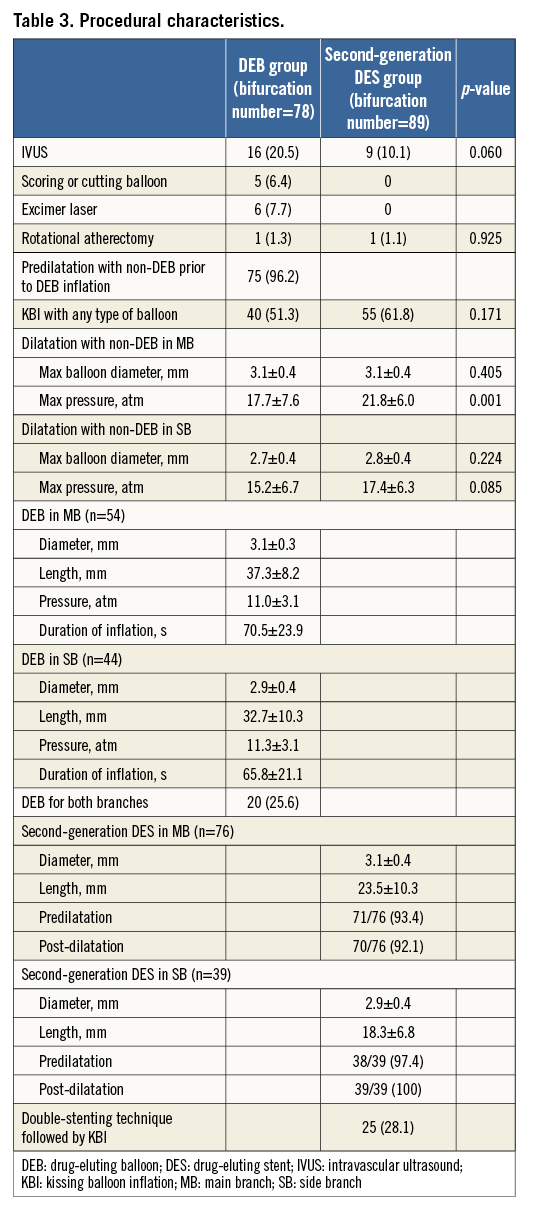
Angiographic characteristics are shown in Table 2. Regarding restenosed stent type, second-generation DES was more frequently seen in the DEB group (26.9% vs. 6.7%, p<0.001). Also in the DEB group, findings which made operators avoid further stenting were more frequently observed, such as restenosis of both the MB and SB (42.3% vs. 25.8%, p=0.025) and restenosis within stent-in-stent (25.6% vs. 14.6%, p=0.074), as compared to the DES group. There were no significant differences in the incidence of true bifurcation defined as Medina 1.1.1/0.1.1/1.0.1 (67.9% vs. 57.3%, p=0.157) as well as restenosis patterns observed either in the MB (p=0.770) or SB (p=0.600). Procedural characteristics are shown in Table 3. Predilatation with non-DEB before DEB inflation was performed in almost all cases (96.2%). Also, in the DES group, both predilatation and post-dilatation were performed in almost all cases. In the DES group, all patients treated by double stenting underwent kissing balloon inflation as post-dilatation. A hybrid strategy (DEB and stenting) was performed in 16 (20.5%) bifurcations in the DEB group. Procedural success was achieved in 74 (94.9%) bifurcations in the DEB group and 88 (98.9%) in the DES group (p=0.130).
CLINICAL OUTCOMES
No deaths or TVR were recorded in the two groups during hospitalisation. However, there were five (6.8%) and four (4.7%) cases of periprocedural MIs in the DEB and DES groups, respectively (p=0.562). Kaplan-Meier curves for MACE and TLR per bifurcation at two-year follow-up are shown in Figure 1A and Figure 1B. There were no significant differences between the two groups in the incidence of MACE (32.1% vs. 27.6%, p=0.593), cardiac death (5.0% vs. 2.6%, p=0.369), TVR (23.7% vs. 21.8%, p=0.884), TLR per patient (16.6% vs. 17.6%, p=0.875) and TLR per bifurcation (19.1% vs. 16.6%, p=0.861). There were no cases of follow-up MI or definite/probable ST at two years.
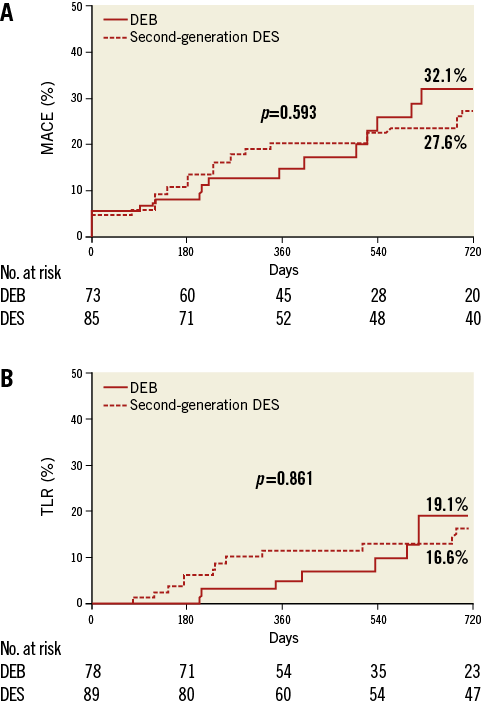
Figure 1. Kaplan-Meier curves (DEB vs. second-generation DES). A) Major adverse cardiac events. B) Target lesion revascularisation per bifurcation.
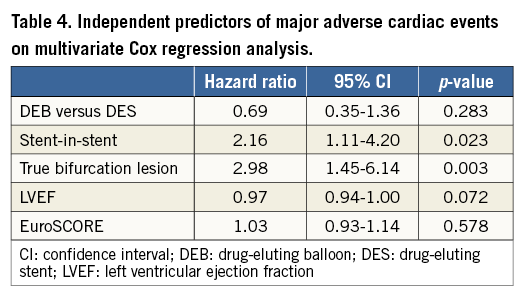
Further analysis in the DEB group, focusing on stent-in-stent vs. first restenosis, demonstrated significant differences in MACE (65.6% in stent-in-stent vs. 16.4% in first restenosis, p<0.001) and TLR per bifurcation (54.1% in stent-in-stent vs. 2.6% in first restenosis, p<0.001) between the two groups (Figure 2A, Figure 2B). In the first restenosis group, restenosed stent types were BMS in 20.7% of cases, first-generation DES in 50% of cases (25.9% sirolimus-eluting stents and 24.1% PES), and second-generation DES in 24.1%. Information regarding stent type was not available in 5.2%.
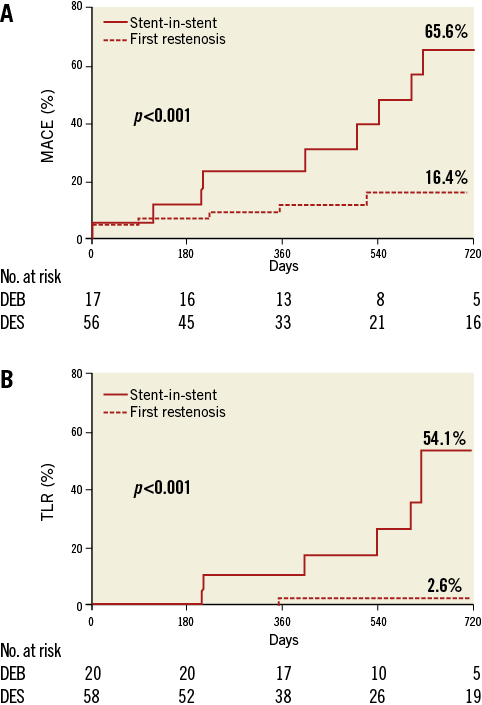
Figure 2. Kaplan-Meier curves (stent-in-stent vs. first restenosis in DEB group). A) Major adverse cardiac events. B) Target lesion revascularisation per bifurcation.
INDEPENDENT PREDICTORS OF MAJOR ADVERSE CARDIAC EVENTS
Independent predictors of MACE on multivariate Cox regression analysis were stent-in-stent (HR: 2.16; 95% CI: 1.11 to 4.20; p=0.023) and the presence of true bifurcation lesions (HR: 2.98; 95% CI: 1.45 to 6.14; p=0.003) (Table 4).
Discussion
The main findings of our study regarding the clinical outcomes following DEB and second-generation DES use for ISR at bifurcation sites are:
1. The incidences of MACE were similar in the two groups at two-year follow-up (32.1% in the DEB group vs. 27.6% in the second-generation DES group) despite the fact that the DEB group had a higher EuroSCORE mainly due to a higher incidence of CKD and higher incidence of stent-in-stent as compared with the second-generation DES group.
2. Independent predictors of MACE were stent-in-stent and the presence of a true bifurcation lesion.
3. DEB use for first restenosis (non stent-in-stent) was associated with acceptable clinical outcomes.
To the best of our knowledge, there have been no studies except for case series that have specifically examined the treatment with DEB for bifurcation ISR. Furthermore, no previous studies reported clinical outcomes following second-generation DES implantation for these specific lesions. Ideally, further stenting at the same site should be avoided, especially if this has already been performed leading to two overlapping stent layers, as this increases the risk of recurrent restenosis and ST. DEB is therefore an attractive therapeutic tool for bifurcation ISR. In this study, we examined all patients who underwent treatment with DEB for such lesions irrespective of bifurcation technique and stent type initially implanted, comparing those treated with currently available DES. Thus, our data represent a real-world experience for the treatment of bifurcation ISR.
Although there are no data focusing on the treatment of bifurcation ISR with DEB, previous studies have examined the role of DEB in overall ISR with variable results. In the Valentines trial (second-generation DIOR®; Eurocor GmbH, Bonn, Germany), the authors reported a 7.4% TLR rate at eight months in a cohort with 63.4% of BMS-ISR (n=250)26. Unverdorben et al reported a TLR rate of 6.3% at 12 months after DEB (SeQuent® Please; B. Braun Melsungen AG Vascular Systems, Berlin, Germany) for BMS-ISR (n=66)5. With regard to DES-ISR, the PEPCAD-DES (PEPCAD DES - Treatment of DES In-Stent Restenosis With SeQuent® Please Paclitaxel Eluting PTCA Catheter) study showed 15.3% of TLR at six months in a group where most patients (78%) were originally treated with limus-eluting stents12. The recently published randomised ISAR-DESIRE 3 (Intracoronary Stenting and Angiographic Results: Drug Eluting Stent In-Stent Restenosis: 3 Treatment Approaches) trial showed that DEB (SeQuent® Please) was non-inferior to PES and superior to uncoated balloon angioplasty in limus-eluting stent restenosis13. The rates of death, MI, TVR, TLR at one year were 2.2%, 2.1%, 24.2%, 22.1%, respectively, in the DEB group, which included 27% of bifurcation lesions. With regard to long-term clinical outcomes following DEB for ISR, the five-year outcome results of the PACCOCATH-ISR (Treatment of In-Stent Restenosis by Paclitaxel Coated PTCA Balloons) I and II have demonstrated that DEB (Paccocath; Bayer AG, Leverkusen, Germany) is safe and associated with reduced TLR (9.3%) as compared with uncoated balloon angioplasty in a population mostly comprising BMS-ISR6. Furthermore, a recent substudy of SCAAR (Swedish CoronaryAngiography and Angioplasty Registry), in which 7.7% were bifurcation lesions, has shown that DEB (SeQuent® Please was used in 82% of cases) was effective in the treatment of BMS-ISR but not in that of DES-ISR11.
In our study, MACE and TLR rates per bifurcation were relatively high but similar in the two groups. Considering the higher EuroSCORE, higher incidence of stent-in-stent and higher incidence of second-generation DES failure in the DEB group, DEB use for bifurcation ISR appears to be an acceptable and reasonable treatment option. Importantly, the TLR rate for DEB-treated first restenoses was satisfactory and similar among the different stent types utilised at the initial PCI. On the other hand, restenosis within stent-in-stent at a bifurcation site is an extremely difficult lesion to treat, with no satisfactory approach as yet available.
One of the possible causes of bifurcation ISR is stent underexpansion. For this reason, aggressive balloon dilatation was performed prior to DEB use in our study. This fact may partially explain our encouraging results in the first restenosis group. Potential advantages of DEB use for bifurcation ISR, besides avoiding further metal layers in an already complex lesion, include the need for shorter dual antiplatelet therapy, minimisation of strut deformation, homogeneous administration of drug to the vessel wall and greater respect of vessel anatomy.
Limitations
Our study has a number of limitations. Firstly, the analysed groups were extremely heterogeneous in their lesion characteristics, such as restenosed stent type, bifurcation stent strategy utilised at the initial PCI, Medina classification, as well as in their procedural characteristics, such as the type of device used in the second-generation DES group. Secondly, as this is a retrospective observational study, the choice of treatment strategy (e.g., DEB or DES) was at the discretion of the operators. Thirdly, the small sample sizes do not allow us to perform a detailed subgroup analysis comparing stent-in-stent vs. first restenosis in the DEB group. Thus, the subgroup analysis performed in our study is based only on univariate analysis. Finally, in view of the group heterogeneity, the different ISR types examined, and the small stent-in-stent restenosis sample size available for analysis, our results should be considered as hypothesis-generating, requiring validation by larger studies.
Conclusions
Our results suggest that DEB for bifurcation ISR may be an acceptable treatment option, especially in cases where repeat stenting has not already been performed for the treatment of a previous restenosis. These results are hypothesis-generating and need to be validated by larger studies.
| Impact on daily practice Drug-eluting balloon (DEB) for bifurcation restenosis may be an acceptable treatment option, especially in cases where repeat stenting has not already been performed for the treatment of a previous restenosis. |
Conflict of interest statement
A. Latib serves on a Medtronic advisory board. The other authors have no conflicts of interest to declare.

