Abstract
Aims: Restenosis and bifurcated lesions represent technically challenging lesions for percutaneous coronary interventions (PCI). Data regarding procedural and clinical outcome of re-PCI for restenosis of stented bifurcated lesions are lacking. Our aims were to evaluate angiographic and procedural results and one-year clinical outcome of PCI for restenosis of stented bifurcated lesions.
Methods and results: Consecutive patients undergoing PCI for restenosis of one bifurcated lesion previously treated by stent implantation at our centre entered the study. The primary endpoint was angiographic and procedural success, defined as final residual stenosis ≤30% in the main vessel with TIMI 3 flow in both MV and side branch, and stenosis ≤50% in the SB without death, myocardial infarction or target vessel revascularisation during hospitalisation. The secondary endpoint was the incidence of major adverse cardiac events at one-year clinical follow-up. The study population included 64 patients treated by PCI on a single restenotic bifurcated lesion. Angiographic and procedural success was achieved in 61 cases (95.3%) whereas the three cases of failure were due to SB residual stenosis >50%. At one year, MACE rate was 18.7% (12/64) with rates of cardiac death, MI and TVR of 1.6% (1/64), 6.2% (4/64) and 18.7% (12/64), respectively. No cases of stent thrombosis occurred. Patients treated by a single drug-eluting stent (DES) on main vessel (MV) had a significant lower rate of MACE at one year as compared to patients treated with balloon only PCI or by double-stenting technique or with a BMS, irrespective of the strategy adopted: 4/37 (10.8%) vs. 8/27 (29.6%); p=0.04.
Conclusions: PCI in restenotic bifurcated lesions can be a good treatment option with high rates of angiographic and procedural success and an acceptable rate of long-term MACE. The use of a single DES implantation may be a promising strategy as it is associated with lower rates of MACE in the long term.
Introduction
Bifurcated lesions and in-stent restenosis (ISR) represent two of the most challenging issues in percutaneous coronary interventions (PCI)1-5, both types of intervention being characterised by an increased technical complexity and higher risk of recurrence. Initially, balloon angioplasty was considered to be an effective treatment of ISR but it soon became evident that the recurrent ISR rate was high. Later, directional and rotational atherectomy6, laser7 and cutting balloon8 failed to demonstrate superiority compared with balloon angioplasty. Coronary brachytherapy results proved to be highly effective in patients with diffuse ISR but this strategy was limited by logistic constraints9,10. In recent years, drug-eluting stents (DES) and drug-eluting balloons (DEB) have emerged as promising new alternatives for patients with ISR11-13, but its optimal treatment remains controversial.
Bifurcation interventions, when compared with non-bifurcation interventions, have a lower rate of procedural success and a higher rate of restenosis1-3. Various techniques have been developed to optimise the treatment of this subset of lesions14-19. The introduction of DES has allowed the reduction of event rates, in particular the rate of main vessel (MV) restenosis20.
Given such premises, treatment of restenosis of bifurcated lesions previously treated by stent implantation can be recognised as highly challenging. The aim of this study was to assess the angiographic and procedural results and the long-term clinical outcome of PCI for restenosis in a stented bifurcation.
Methods
Between March 2005 and December 2007, all consecutive patients treated by PCI for significant restenosis of a single bifurcated lesion previously treated by stent implantation at our institution were included in this study. Procedural, angiographic and clinical data were prospectively collected for all the study population and entered into an electronic database (Cardio-planet V.3.0.8, Ebit Aet S.p.A., Genoa, Italy). Patients aged <18 years or unable to give informed consent, with known hypersensitivity or contraindication to aspirin, clopidogrel, heparin, ticlopidine or contrast dye, with chronic total occlusion, ST-elevation myocardial infarction undergoing primary PCI, cardiogenic shock and bifurcation with MV and/or side branch (SB) diameter ≤ 2.0 mm were excluded.
PERCUTANEOUS CORONARY INTERVENTIONS
All procedures were performed by interventional cardiologists who met minimal proficiency criteria of performance of ≥100 interventional cases per year. PCI technique was left to the operator’s discretion. Final kissing balloon was always attempted in the case of a double-stenting technique, while it was left to the operator’s discretion in the case of single stent implantation.
All patients were pretreated with aspirin and clopidogrel. A 300 mg loading dose of clopidogrel before the index procedure was administered if patients were not pretreated. The double antiplatelet therapy was continued in all the patients for at least 12 months. During the procedure, patients received intravenous unfractionated heparin to maintain an activated clotting time between 250 and 300 seconds. The administration of glycoprotein IIb/IIIa inhibitors was left to the operator’s discretion.
After PCI, all patients underwent a post-PCI electrocardiogram (ECG) as well as six-hour and 24-hour assessment of creatine-kinase (CK) and creatine-kinase-MB (CK-MB) levels. Thereafter, additional ECGs and enzyme evaluations were performed if clinically indicated.
QUANTITATIVE CORONARY ANGIOGRAPHIC ANALYSIS
Matched orthogonal views were used for three-dimensional quantitative coronary analysis (QCA) (CardioOp-B System; Paieon Medical Ltd, Park Afek, Israel)21 before and after treatment. Angiograms were analysed off-line by two independent investigators blinded to patient identities and outcomes.
STUDY ENDPOINTS
Primary endpoints were angiographic and procedural success. Angiographic success was defined as final residual stenosis ≤30% in the MV with TIMI 3 flow in both MV and SB and stenosis ≤50% in the SB. Procedural success was defined as angiographic success without the occurrence of cardiac death, MI or TVR during hospitalisation.
The secondary endpoint was the incidence of major adverse cardiac events (MACE) defined as the composite of cardiac death, myocardial infarction (MI) and target vessel revascularisation (TVR) at one-year clinical follow-up and the incidence of stent thrombosis. In all cases, the one-year follow-up was performed by clinical visit or phone call. All deaths were considered cardiac unless otherwise documented.
MI was defined as recurrent chest pain or ischaemia equivalent, or the appearance of new pathological Q-waves in ≥2 ECG contiguous leads with post-procedure CK-MB levels above normal or as an elevation of post-procedural CK levels >2 times normal levels with elevated CK-MB in the absence of chest pain or ischaemia equivalent, or pathological Q-waves22.
TVR was defined as clinically-driven revascularisation by either PCI or coronary artery bypass grafting (CABG) involving the treated vessel.
Stent thrombosis (ST) was classified by the Academic Research Consortium definition as definite, probable or possible, and as early (0-30 days), late (31-360 days) or very late (>360 days)23.
Statistical analysis
Data were expressed as mean±SD for continuous variables and frequencies, and percentages for the categorical variables. For comparison of categorical data, χ2 test or the Fisher exact test was performed. For comparison of continuous variables, a two-tailed paired Student’s t-test was used. Statistical significance was declared if the two-sided p value was <0.05. All analyses were performed using SPSS version 14 (SPSS Inc, Chicago, IL, USA).
Results
STUDY POPULATION
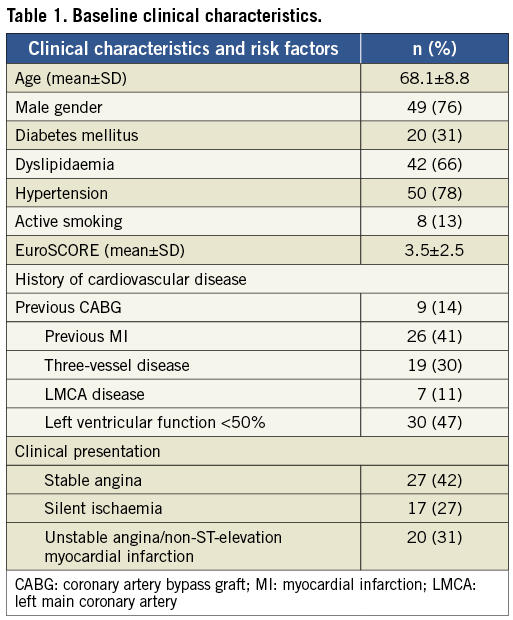
The study population included 64 patients (49 men, age 68±8 years) treated by PCI on a single restenotic bifurcated lesion. Main clinical characteristics of the study population are summarised in Table 1. Briefly, 31% were diabetics, 31% were admitted for acute coronary syndrome and 47% had impaired left ventricular function. Left main coronary artery disease and three-vessel disease were present in 10.9% and 29.6%, respectively.
PRE-PCI ANGIOGRAPHIC CHARACTERISTICS AND PERCUTANEOUS CORONARY INTERVENTIONS
The angiographic characteristics of the study population are shown in Table 2. In all cases, the strategy selected was decided by the operator according to: 1) angiographic lesion characteristic; 2) complexity of the case; 3) personal preferences. The bifurcation most frequently involved was the left anterior descending artery-diagonal (50% of the cases). The stent distribution after the first PCI on target bifurcation lesions was: MV stenting only 72% (46/64), MV+SB stenting 22% (14/64) and SB stenting only 6% (4/64) (Figure 1). The restenotic process involved both MV and SB in 53% (34/64) of the cases, MV only in 38% (24/64) and SB only in 9% (6/64) (Figure 2).
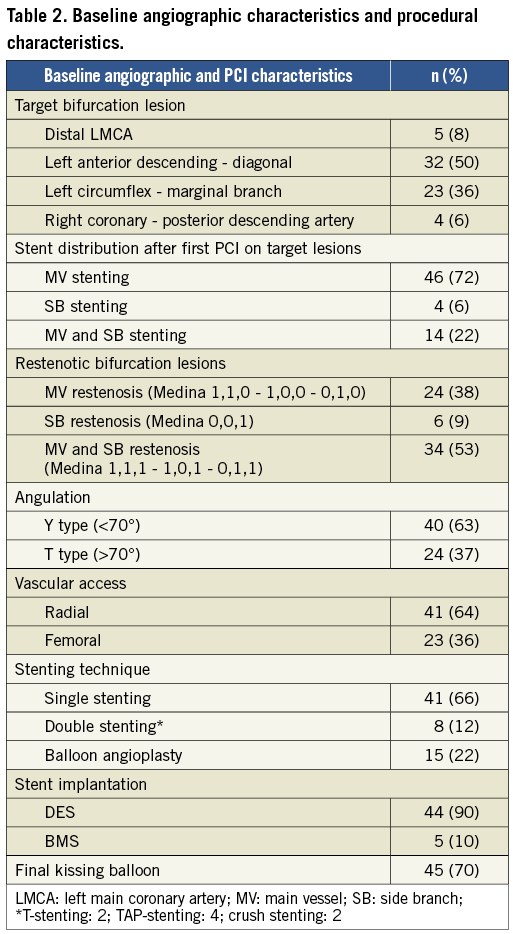
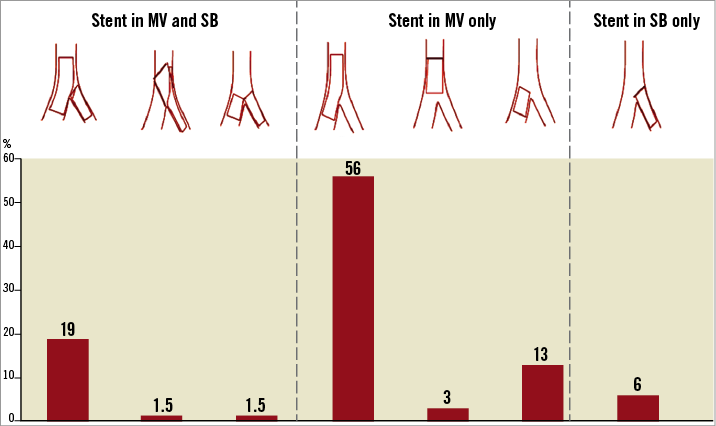
Figure 1. Stent distribution after first PCI in target bifurcation lesions.
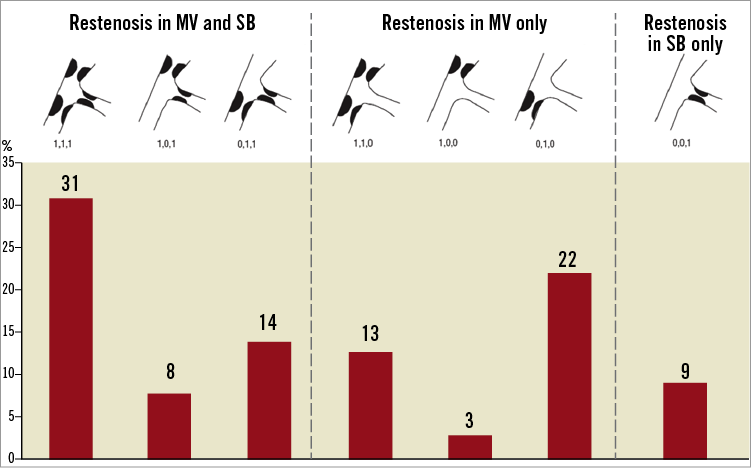
Figure 2. Baseline angiographic characteristics of the restenotic bifurcation lesions.
Procedural data are are reported in Table 2. In particular, 66% (41/64) of patients received single stenting on MV, 12% (8/64) double stenting and 22% (15/64) balloon angioplasty only. A DES was implanted in 90% of patients receiving a stent (44/49). Final kissing balloon was performed in 70% (45/64) of cases (always in double-stenting technique and 56% in single-stenting cases).
QUANTITATIVE CORONARY ANGIOGRAPHIC ANALYSIS
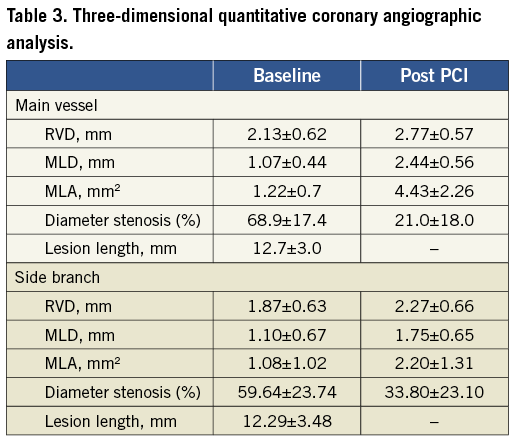
MV and SB three-dimensional QCA results at baseline and after procedure are summarised in Table 3. The CardioOp-B system21 was able to provide automatic three-dimensional reconstructed analysis in 96.9% of cases (62 patients). Major improvements in diameter and area were documented in both MV and SB by 3-D-QCA analysis (main vessel MLA 1.22±0.7 vs. 4.43±2.26 mm2; main vessel MLD 1.07±0.44 vs. 2.44±0.56 mm; side branch MLA 1.08±1.02 vs. 2.20±1.31 mm2 and side branch MLD 1.10±0.67 vs. 1.75±0.65 mm). No significant differences in the QCA results were found according to the technique adopted.
ANGIOGRAPHIC, PROCEDURAL AND CLINICAL OUTCOMES
Angiographic success was achieved in 61 cases (95.3%). The three cases of failure were due to SB residual stenosis >50%. The rate of procedural success was 95.3%, as no in-hospital MACE occurred. Clinical follow-up was available in all patients at one year. Total MACE rate was 18.7% (12/64), with rates of cardiac death, MI and TVR of 1.6% (1/64), 6.2% (4/64) and 18.7% (12/64), respectively. The only cardiac death was observed in a patient who suffered NSTEMI due to repeated bifurcation ISR sent to cardiac surgery and who died in the postoperative period. Concerning the patients who presented with TVR at follow-up, nine (14%) were treated by re-PCI and three (4.7%) by CABG. There were no cases of stent thrombosis.
Patients treated with double-stenting techniques had a non-significant higher rate of MACE at one year as compared to patients treated by single stent on MV (2/8 [25%] vs. 6/41 [14%]; p=0.27). Kissing balloon (KB) technique was performed in 45 cases (100% in double-stenting techniques); in this group, MACE was present in 10/45 (22.2%) vs. 2/19 (10.5%) in cases without KB (p=0.23). Results and details about each strategy are shown in Table 4.
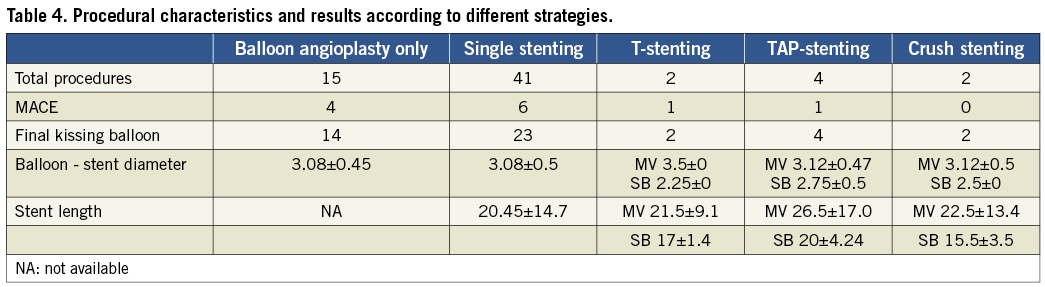
To evaluate MACE according to the stent used, we allocated patients to one of two groups: DES patients vs. non-DES patients (BMS or balloon angioplasty only). A trend was observed towards a lower incidence of MACE at one year in the DES group as compared to the non-DES group (4/44 [9%] vs. 4/19 [21%]; p=0.18). We then compared the rate of MACE at one year in the group of patients treated by a single DES on MV with the rate of MACE at one year in the group of patients treated with balloon only PCI or double-stenting technique or BMS, irrespective of the strategy adopted. The patients treated by a single DES had a significantly lower rate of MACE at one year as compared to the patients treated by all of the other strategies adopted (4/37 [10.8%] vs. 8/27 [29.6%]; p=0.04) (Figure 3).
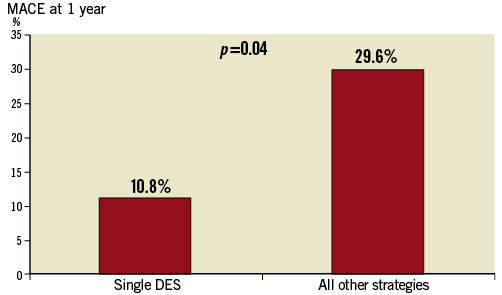
Figure 3. MACE at 1 year in patients treated with a single DES strategy versus MACE at 1 year in patients treated with all other strategies.
Interestingly, all the events at one year registered in the group of patients treated with a single DES were TVR, all treated by a re-PCI.
Discussion
Our study is one of the first specific reports on PCI treatment of in-stent restenosis in bifurcated lesions and focused on the angiographic success rate of such complex procedures as well as on their clinical efficacy in terms of in-hospital and long-term clinical outcome. To the best of our knowledge, there are only two studies analysing this issue: the study from Costa et al24 which reported the outcomes of five patients treated with brachytherapy for bifurcation-ISR and the experience of Kim et al who reported DES treatment for specific LMCA BMS restenosis25. In the remaining studies which evaluated ISR, bifurcation restenoses were analysed along with other lesions, despite the known differences in terms of treatment techniques and outcomes.
Data from several studies show that MACE rates after treatment of ISR or bifurcated lesions is about 15% for each condition1,2,26,27. Interestingly, in our population the angiographic success rate was high with only three cases of failure due to SB residual stenosis >50%. Moreover, no coronary events occurred during hospitalisation after the procedure. Finally, MACE rate at one year was 18.7% and was principally driven by TVR.
The operator’s decision to use DES in most of the patients corresponds with data coming from both ISR and bifurcation trials, where DES improved angiographic success and clinical outcome when compared with BMS and balloon angioplasty5,12,20,28-30. Likewise in our study, we found a non-significant trend to better clinical outcomes in patients treated by DES as opposed to BMS or balloon angioplasty only. Moreover, we found a significantly better outcome with single DES implantation as compared to all other strategies, showing concordance with previous studies on bifurcation lesions reporting clinical advantages of provisional stenting as compared to double-stenting techniques31,32. Interestingly, we found a trend towards a lesser incidence of MACE in patients in whom the KB technique was not performed: these finding can probably be explained by less complex bifurcation lesions and by the treatment technique.
Study limitations
The drawbacks of this study are typical of single-centre observational studies33. Thus, no definitive conclusions on the optimal technique for the treatment of ISR of bifurcated lesions can be derived from our results. As the stenting technique was left to the operator’s discretion, it is possible that more complex procedures were performed in more complex lesions, resulting in a potential bias of selection. Other limitations include the small study population and the lack of IVUS data, especially important in these complex lesions. During the study, drug-eluting balloons were not available in our institution; their role in this subset of lesions requires evaluation.
Conclusions
In an unselected population of patients with in-stent restenosis of bifurcated lesions, treatment with PCI appears to be safe and effective with high rates of angiographic and procedural success and acceptable rates of long-term MACE. Moreover, provisional single DES implantation appears to be the best option, as it is associated with a lower rate of MACE. Further studies are warranted to assess the best treatment strategy for this complex subset of lesions.
Conflict of interest statement
The authors have no conflicts of interest to declare.

