Abstract
Aims: Lesion location might influence the efficacy of the bifurcation two-stent approach relative to the one-stent approach.
Methods and results: One-year outcomes after sirolimus-eluting stent (SES) implantation with the two-stent approach were compared to those with the one-stent approach in left main coronary artery (LMCA) bifurcation (945 lesions) and in left anterior descending coronary artery (LAD) bifurcation (1271 lesions). The two-stent approach was used more frequently in LMCA than in LAD. The target-lesion revascularisation (TLR) rate in the two-stent group was significantly higher than that in the one-stent group in LMCA (24.2% vs. 5.6%, p<0.0001), but not in LAD (9.0% vs. 5.4%, p=0.056). Adjusted odds ratio of two-stent versus one-stent for TLR was 4.93 (3.01-8.08, p<0.0001) in LMCA and 1.15 (0.64-2.07, p=0.63) in LAD, respectively (interactionp<0.0001). Angiographic restenosis rates in the main branch were significantly higher in the two-stent group in both LMCA and LAD (11.0% vs. 4.9%, p=0.02; and 13.2% vs. 6.8%, p=0.02). Restenosis rates in the side branch were significantly higher in the two-stent group in LMCA (35.3% vs. 14.5%, p<0.0001), but not in LAD (15.1% vs. 22.6%, p=0.07).
Conclusions: Risk of TLR after bifurcation stenting in lesions that needed the two-stent approach was significantly different between LMCA and LAD bifurcations.
Introduction
Coronary bifurcation lesions remain a challenge for percutaneous coronary intervention (PCI) and the optimal stenting strategy has not been established in the current drug-eluting stent (DES) era. Several randomised controlled trials comparing complex stenting strategy with provisional side branch stenting strategy mainly in non-left main coronary artery bifurcation lesions consistently demonstrated that there were no differences in both target-lesion revascularisation (TLR) rate and angiographic restenosis rate between the two strategies1,2. In contrast, observational studies mainly in left main coronary artery (LMCA) bifurcation lesions have shown that the bifurcation two-stent approach (stenting both main and side branches), as compared with the one-stent approach (main branch stenting alone), was associated with higher rates of TLR3-5.
We hypothesised that the difference in lesion location may contribute to this apparent discrepancy after the bifurcation two-stent approach between randomised controlled trials and observational studies. This post hoc subgroup analysis of the j-Cypher registry was intended to compare outcomes of the two-stent approach relative to the one-stent approach in LMCA bifurcation lesions and in left anterior descending coronary artery (LAD) bifurcation lesions. The purpose of this analysis was to assess whether the lesion location, especially left main bifurcation, might influence the incidence of TLR and angiographic restenosis after bifurcation stenting.
Methods
Study design and patient population
The study design and patient enrolment for the j-Cypher registry has been described in detail elsewhere6. From August 2004 to November 2006, 12,824 patients were enrolled in the j-Cypher registry for the first time. Among those 12,824 patients, there were 3,410 patients (26.6%) with bifurcation lesions (3,716 lesions). We identified the current study population of 945 patients (945 lesions) in the LMCA stratum and 1,252 patients (1,271 lesions) in the LAD stratum treated exclusively with SES (Figure 1). We compared LMCA bifurcation with LAD bifurcation lesions because the LAD-diagonal bifurcation lesions are the most commonly treated bifurcation lesions in clinical practice. Ostial LAD and ostial left circumflex coronary artery (LCX) lesions without significant LMCA stenosis were included in the LMCA stratum.
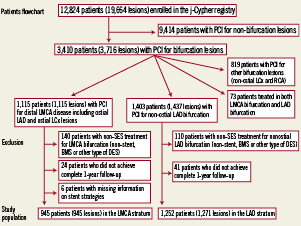
Figure 1. Patient flowchart. BMS: bare-metal stent; DES: drug-eluting stent; LAD: left anterior descending coronary artery; LCX: left circumflex coronary artery; LMCA: left main coronary artery; PCI: percutaneous coronary intervention; RCA: right coronary artery; SES: sirolimus-eluting stent
The relevant review boards in all 37 participating centres approved the study protocol. Written informed consent was obtained from all patients enrolled.
Definitions
Bifurcation lesion was defined as involving a side branch ≥2.2 mm in diameter. Selection of the bifurcation stenting strategies was left to the discretion of the operators. Technical details of bifurcation stenting were recorded in the case report forms during the index stent implantation procedures. The two-stent approach was defined as stenting both main and side branches, while the one-stent approach was defined as main branch stenting alone. When stenting of the side branch ostium was performed before stenting of the main branch, the procedure was regarded as an elective two-stent strategy. When stenting of the main branch was performed first, the procedure was regarded as a provisional side branch stenting strategy. Decision regarding the final kissing balloon dilatation was also left to the operators.
Myocardial infarction (MI) was adjudicated according to the definition in the Arterial Revascularisation Therapy Study7. Within one week of the index procedure, only Q-wave MI was adjudicated as MI because protocol-specified measurements of periprocedural myocardial biomarkers were not conducted. Stent thrombosis (ST) was defined according to the Academic Research Consortium (ARC) definition. ARC “definite ST” on a lesion-level basis was used as the endpoint for ST8. TLR was defined as either PCI or coronary artery bypass grafting (CABG) surgery due to restenosis or thrombosis of the target lesion that included the proximal and distal edge segments as well as the ostium of the side branches. There was no distinction of whether TLR was clinically- or angiographically-driven.
Coronary angiographic parameters were assessed in each participating centre either by visual assessment or by quantitative angiographic measurement. Vessel diameter, minimal luminal diameter and percent diameter stenosis were reported for both the main branch and the side branch. Lesion length was assessed only for the main branch. Angiographic binary restenosis was defined as percent diameter stenosis >50%.
Statistical analysis
Categorical variables are presented as counts and/or percentages and were compared with the chi-square test. Continuous variables were expressed as mean ±SD unless otherwise indicated. Continuous variables were compared with the t-test or Wilcoxon rank sum test on the basis of their distributions. Analysis of variance was used for comparisons for bifurcation types defined by the Medina classification or for various two-stent techniques.
One-year clinical outcomes were compared between the two-stent approach and the one-stent approach in the LMCA stratum and in the LAD stratum, respectively. The primary outcome measure for the current analysis was TLR at one year after the index SES implantation procedures. TLR and ST were evaluated on a lesion-level basis. All-cause death, cardiac death and MI were assessed on a patient-level basis. We used a logistic regression model rather than the Cox proportional hazard model to assess the risk for the primary outcome measure (TLR), because the timing of TLR was known to be sensitive to physicians’ judgement and, thus, the proportional assumption was not justified9. Those patients with complete one-year follow-up were included in the analysis. Censored cases who died within one year without the occurrence of any endpoint event were excluded from each analysis to make a definite cohort who had survived at one-year or experienced an event until one year: 94 patients who died within one year without the occurrence of TLR were excluded for the analysis of TLR; 38 patients who died within one-year due to non-cardiac causes were excluded from the analysis of cardiac death. Adjusted odds ratios of the two-stent approach versus the one-stent approach and corresponding 95% confidence intervals for the one-year clinical events such as TLR, all-cause death, cardiac death and cardiac death or MI, were estimated with logistic regression models in each stratum. All variables in Table 1 and Table 2 were used as candidates for risk factors, and we selected those with p<0.05 for TLR in the lesion level analysis and for all-cause death in the patient level analysis. In the lesion-level analysis, the model for TLR was adjusted for diabetes, dialysis, hypertension, heart failure and stent diameter <3.0 mm in the main branch. In the patient-level analysis, models for all-cause death, cardiac death, cardiac death or MI were adjusted for heart failure, renal failure, emergent procedure, EuroSCORE≥6, age ≥75 years, male, acute coronary syndrome, shock state at the time of the index procedures, triple vessel disease, extra-cardiac arteriopathy, history of stroke and insulin required diabetes mellitus.
We also constructed logistic-regression models with interaction between the stent strategies and lesion location to assess whether the effect sizes of the two-stent approach were different between the LMCA and LAD strata.
Probability was considered to be significant at a level of <0.05. All statistical tests were 2-tailed. Statistical analyses were conducted by a physician (Mamoru Toyofuku) and a statistician (Takeshi Morimoto) with the use of JMP 8.0.2 (SAS Institute Inc, Cary, NC, USA) software and SAS 9.1 (SAS Institute Inc).
Results
Baseline characteristics
The two-stent approach and the one-stent approach were used in 204 patients (204 lesions) and 741 patients (741 lesions) in the LMCA stratum, and in 219 patients (222 lesions) and 1,033 patients (1,049 lesions) in the LAD stratum, respectively. The proportion of patients with the two-stent approach was higher in the LMCA stratum than in the LAD stratum (21.6% vs. 17.5%, p=0.02).
Baseline patient characteristics were generally similar between the one-stent group and the two-stent group in both the LMCA stratum and the LAD stratum (Table1). However, the two-stent group, as compared with the one-stent group, had a greater number of vessels treated. True bifurcation lesions and use of final kissing balloons were more common and the number of stents used was greater in the two-stent group than in the one-stent group (Table 2).
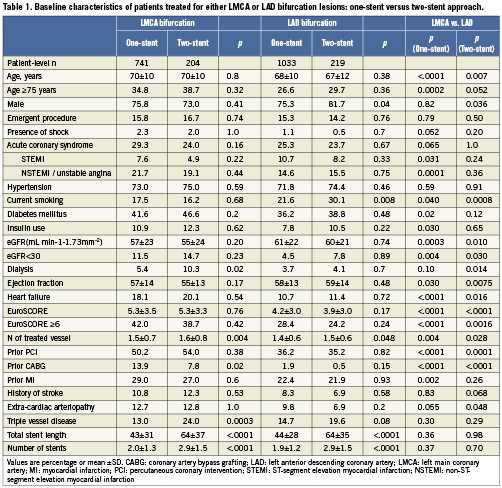
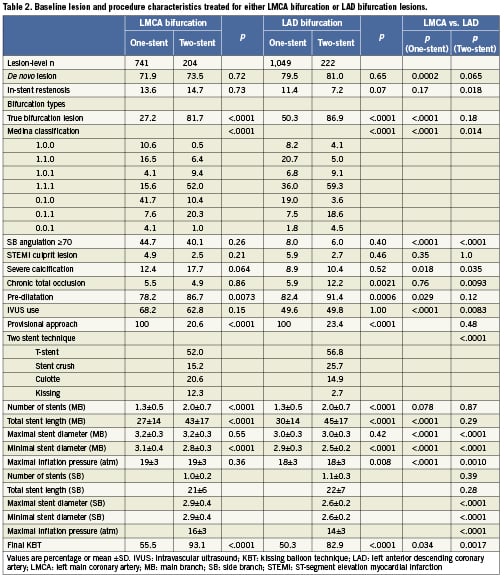
In the comparison between the LMCA stratum and the LAD stratum, obtuse side branch angulation (side branch angulation ≥70 degree) was more prevalent in the LMCA stratum. In the lesions treated with the one-stent strategy, the LMCA stratum included relatively greater proportions of Medina 0,1,0 lesions (41.7% vs. 19.0%), and relatively less proportions of Medina 1,1,1 lesions (15.6% vs. 36.0%) as compared with the LAD stratum.
Stent diameter in both the main branch and the side branch was greater in the LMCA stratum.
Clinical outcome
The two-stent approach was associated with a significantly higher incidence of TLR than the one-stent approach in the LMCA stratum (24.2% vs. 5.6%, p<0.0001), but not in the LAD stratum (9.0% vs. 5.4%, p=0.056) (Table 3 and Figure 2). After adjustment for confounders, the two-stent approach was associated with a significantly higher risk of TLR in the LMCA stratum (odds ratio [OR] 4.93, 95% confidence interval [CI]: 3.01-8.08, p<0.0001), but not in the LAD stratum (OR 1.15, 95% CI: 0.64-2.07, p=0.63) (Figure 3). There was significant interaction between the stent strategies and lesion locations (p interaction <0.0001).
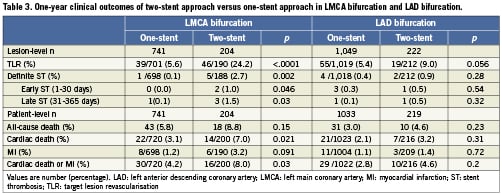
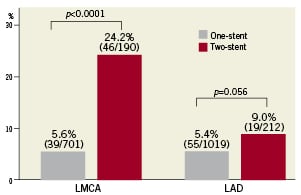
Figure 2. Target lesion revascularisation rates: two-stent vs. one-stent approach in the LMCA and LAD strata. LAD: left anterior descending coronary artery; LMCA: left main coronary artery
Although there were no differences in the adjusted risk of all-cause death between the one-stent and the two-stent strategies in both strata, the adjusted risk of cardiac death was also significantly higher in the two-stent group as compared with the one-stent group (OR 3.19, 95% CI: 1.31-7.76, p=0.011) in the LMCA stratum, but not in the LAD stratum (OR 1.46, 95% CI: 0.55-3.82, p=0.45). However, probability of interaction between the stent strategies and lesion locations was not significant (interaction p=0.42) (Figure 3).
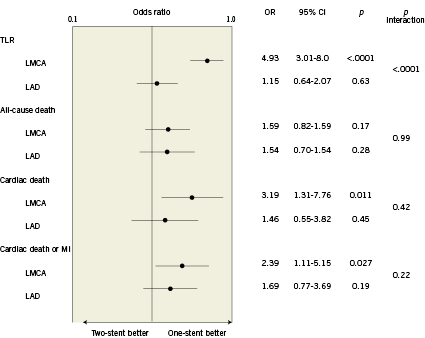
Figure 3. Adjusted odds ratios of two-stent vs. one-stent approach for each endpoint in the LMCA and LAD strata. The p value for interaction represents the likelihood of interaction between the lesion location of LMCA or LAD and the treatment effect of one-stent or two-stent. LAD: left anterior descending coronary artery; LMCA: left main coronary artery; MI: myocardial infarction; TLR: target lesion revascularisation
Angiographic results
Among 1,651 lesions (74.5% of the whole cohort) with follow-up angiogram within one-year after the index procedures, 1,449 lesions were available for quantitative angiographic analysis. Median interval between the index stent implantation procedure and the follow-up angiographic evaluation was 240 (inter-quartile range: 186-270) days. The angiographic restenosis rate in the mainbranch was significantly higher in the two-stent group than in the one-stent group, both in the LMCA stratum (11.0% vs.4.9%, p=0.02), and in the LAD stratum (13.2% vs. 6.8%, p=0.02), respectively. The angiographic restenosis rate in the side branch was significantly higher in the two-stent group than in the one-stent group in the LMCA stratum (35.3% vs. 14.5%, p<0.0001), but not in the LAD stratum (15.1% vs. 22.6%, p = 0.07) (Table 4 and Figure 4).
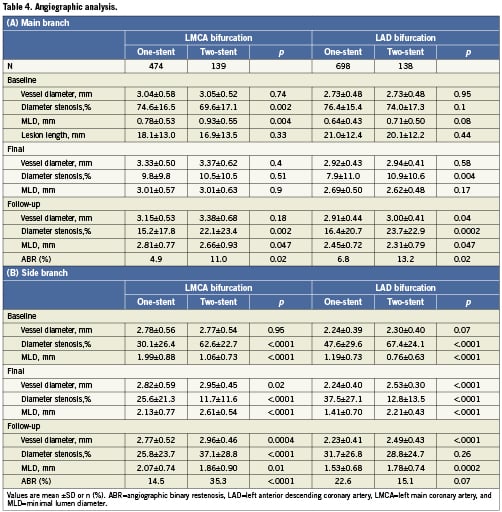
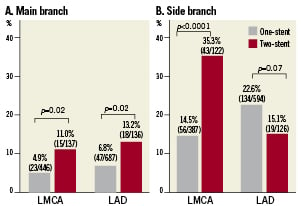
Figure 4. Angiographic binary restenosis in the main branch (A) and in the side branch (B). LAD: left anterior descending coronary artery; LMCA: left main coronary artery
Discussion
The main finding of this study is that the incidences of TLR and angiographic restenosis after stenting of bifurcation lesions that needed the two-stent approach were different according to the lesion locations (i.e., LMCA bifurcation vs. LAD bifurcation). The rate of TLR was significantly higher in the two-stent group than in the one-stent group in the LMCA bifurcation, but not in the LAD bifurcation. The difference in the rate of TLR could be explained by the higher rate of restenosis in the side branch after use of the two-stent approach in the LMCA bifurcation.
In the drug-eluting stent era, several randomised controlled trials comparing complex approaches with simple approaches have consistently demonstrated that there were no differences in both TLR rate and angiographic restenosis rate between the two strategies1,2. Recent meta-analyses of randomised studies comparing simple stenting strategy versus complex stenting strategy in coronary bifurcation lesions have also showed that there were no significant differences between the two different strategies with respect to the rates of cardiac death, TLR, and angiographic restenosis, although there was an increasing risk of MI and concern about increasing ST in the complex strategy group10,11. In the most recently published large randomised trial of bifurcation stenting strategies (BBC-ONE)12 using paclitaxel-eluting stents (PES) for non-LMCA bifurcation lesions, the systematic two-stent strategy as compared with the simple strategy resulted in a comparable rate of target-vessel revascularisation (TVR) and a higher rate of MI.
Contrary to the results from randomised controlled trials in non-LMCA bifurcations, observational studies mainly in LMCA bifurcation lesions have shown that the bifurcation two-stent approach, as compared with the one-stent approach, was associated with higher rates of TLR3-5. In our previous study of unprotected LMCA lesions from the j-Cypher registry, the three-year TLR rate was significantly higher in the two-stent group as compared with the one-stent group (31% vs. 11%, p<0.0001)5.
One of the reasons for this apparent discrepancy between the randomised controlled trials and the observational studies seems to be related to a selection bias in the observational studies leading to more complex lesions in the two-stent group. In the current analysis, however, the efficacy of two-stent strategy versus one-stent strategy was different between the LMCA and LAD bifurcations. Therefore, the difference in lesion location might also partly explain the discrepancy between the randomised controlled trials for non-LMCA bifurcation lesions and observational studies dedicated to the LMCA bifurcation lesions. There seem to be different anatomic characteristics such as bifurcation angulation between the LMCA and LAD bifurcations. In our study population, the proportion of lesions with a wide bifurcation angle was significantly greater in the LMCA stratum than in the LAD stratum. In a sub-analysis of the SYNTAX trial studying the relations between LMCA bifurcation angle and clinical outcomes using three-dimensional quantitative coronary angiography, the event rates tended to be lower in patients with a narrower diastolic distal bifurcation angle among patients with ≥2 stents in the LMCA bifurcation (12 month major cardiac and cerebrovascular events: 14.6% in the 1st tertile group, 18.4% in the 2nd tertile and 22.6% in the 3rd tertile group)13. These results might suggest that an obtuse bifurcation angle had an adverse effect on the outcome of the side branch stenting by creating acute bend of side branch.
Restenosis after the bifurcation two-stent approach in the LMCA bifurcation most often involves the ostium of LCX3,4. The ostium of LCX was known to be subjected to vigorous motion during cardiac cycles. Vigorous motion of the coronary artery segment might provide some mechanical stimulation for neo-intimal hyperplasia.
Study limitations
There are several limitations in the present study. First, this was an observational study. Baseline differences of lesion characteristics may bias the comparison between the one-stent and two-stent strategies even after adjustment for confounders. Moreover, there were no protocol specified strategies for bifurcation stenting, and selection bias at operator level possibly influenced our results. Second, because protocol specified measurement of myocardial biomarkers were not conducted after the index procedures, we could not address the concerns for increased incidence of periprocedural non-Q wave MI in the two-stent group. Third, TLR events in the present study included both clinically-driven and angiographically-driven events. Routine follow-up angiography was performed in most of the participating centres. The clinical significance of angiographically-driven TLR of jailed side branch remains unclear. From physiological assessment using fractional flow reserve, angiographic restenosis in the ostial side branch lesions after stenting is not always related to functional myocardial ischaemia14. Fourth, quantitative angiographic data were not evaluated by an angiographic core laboratory, but were reported by the site investigators. Mixing data derived either by visual estimation or quantitative coronary angiography was a clear limitation of this study. Finally, we might be more prone to perform TLR for restenosis of ostial LCX than for restenosis of ostial diagonal branch, because the former usually subtends a larger area of myocardium than the latter. However, the different outcomes of the two-stent approach between the LMCA and the LAD bifurcations would most likely represent a true biological phenomenon, because angiographic restenosis rates in the side branches after the two-stent approach were markedly different between these two lesion locations.
Conclusion
In the LMCA bifurcations, the risk of TLR after stenting in bifurcation lesions that needed the two-stent approach was significantly higher than the risk in lesions that could be treated with the one-stent approach, while the risk was comparable in the LAD bifurcations. The risk of TLR after the bifurcation two-stent approach seemed to be different according to lesion locations.
Acknowledgements
We gratefully thank the members of the cardiac catheterisation laboratories of the participating centres, as well as the clinical research coordinators.
Funding sources
Sponsored by Cordis Cardiology, Japan, Johnson and Johnson K.K., Tokyo, Japan.
The study sponsor was involved in the discussion of the study design. However, the study sponsor was not involved in the analysis, collection of data and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Conflict of interest statement
Dr Kimura serves as an advisory board member for Cordis Cardiology and has received honoraria from Cordis Cardiology. The remaining authors have no conflicts of interest to declare.

